Spondyloarthrosis (osteoarthritis) is a common pathology of the lumbar spine. Spondyloarthritis of the lumbosacral spine is more common in older people, but it can also develop in people who do heavy physical work, are obese, or in anyone who has had a previous spinal injury.
Osteoarthritis of the lumbar spine develops in the joints that connect the segments of the spine. Each vertebra is connected to another vertebra in three places. In front of the spinal cord, the vertebrae are separated by the spinal disc. Behind the spinal cord, the vertebrae are connected by two small joints called facet joints. These joints, along with the intervertebral disc, allow the spine to move and perform movements such as bending and extension or rotation of the back.
Treatment of spondyloarthrosis of the lumbar-sacral spine can be either conservative or surgical, and the choice of treatment tactics depends mainly on the clinical picture.
Causes
Common causes of osteoarthritis of the facet joints of the lumbar spine are:
- Degenerative changes in joints and wear and tear of joints over time.
- Disc degeneration can cause the distance between vertebrae to decrease, which will increase stress on the facet joints, accelerating wear and tear on these joints.
- Backward movements of the trunk (extensions) can put pressure on the facet joints, which can lead to degenerative changes.
- A sudden fall or injury, such as a car accident, can damage the facet joints, increasing and accelerating wear and tear on the joints.
- Genetic factors may influence your likelihood of developing degenerative joint disease.
- Repetitive stress injuries, such as lifting or carrying heavy objects, can cause joint irritation and degeneration.
Kinds
Depending on the course of the pathological process, spondyloarthrosis is divided into several types:
- Degenerative – the structure of the intervertebral disc is disrupted, the articular surfaces are destroyed.
- Deforming – under the influence of osteophytes, the vertebrae change their shape.
- The facet is a pathological process that develops in the joints located between the spine and ribs.
- Ancholysing – in other words, ankylosing spondylitis, during which numerous injuries and deformations of the joints occur.
- Dysplastic – accompanied by a complete disruption of the structure of the joints.
- Polysegmental – affects several parts of the spine simultaneously.
- Uncovertebral – the disease is localized between the spinous processes in the area of the first and second cervical vertebrae.
Symptoms
Symptoms of spondyloarthrosis of the lumbar spine will depend on which motor segment is most damaged and the degree of impact on nearby nerve structures.
Symptoms can range from mild to severe and can mimic those of disc disease:
- Back pain or radicular pain radiating into the buttock, into the leg and extending down to the back of the knee, less commonly to the front of the leg or foot.
- Pain and tenderness are localized at the level of the facet joint involved in the pathological process.
- Muscle spasm and forced changes in posture.
- Loss of movement, such as the inability to straighten, bend the body to the side, or maintain an upright position for long periods of time.
- There may be disturbances in walking and standing in cases of severe pathological process
- Sitting is usually more comfortable.
- Change in normal lumbar curvature or lordosis.
- Development of stenosis-like symptoms.
- Stiffness in the joints after a period of rest.
- Pain after excessive activity and pain relief after rest.
- There may be some swelling at the level of the pathologically changed facet joints.
- Muscle weakness in the lower extremities or symptoms of cauda equina syndrome due to the development of spinal stenosis
General clinical picture
The disease is classified based on severity . The first stage is asymptomatic or with vague symptoms. Occasionally, discomfort appears in the back, but few take them seriously.
This is followed by thinning of the cartilaginous tissues, and the mobility of the cartilaginous vertebrae decreases. In advanced forms of the disease, their movement can be completely blocked. Further development of pathology can be avoided by using conservative treatment methods and performing special exercises.
The development of dangerous complications begins with stage 2 spondylosis deformans. With this form of the disease, it is impossible to heal with just gymnastics and massages. To eliminate symptoms, blockades are used.
Diagnostics
A patient who has been experiencing back pain or stiffness for more than two weeks should see a doctor for a physical examination.
Disease history
The physician must evaluate the patient's medical history, examine symptoms, pain characteristics, and joint function, how and when symptoms began, and how they have changed over time.
The doctor also needs to find out the presence of concomitant pathology, previous treatment, family history and bad habits (for example, alcohol consumption, smoking, etc.),
Physical examination. The doctor will need to perform a physical examination to evaluate the patient's general health, muscle and bone condition, nerve conduction, reflexes, and spinal joint mobility.
The doctor also needs to obtain information about the patient's muscle strength, flexibility, and ability to perform activities of daily living, such as walking, bending, and standing.
The patient may need to perform some movements so that the doctor can understand the range of motion and determine which movements increase symptoms.
Instrumental diagnostic methods
Radiography
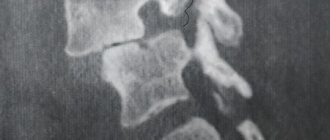
- a doctor may order an x-ray to see if there is injury to the spinal joints and how extensive it is. X-rays can show cartilage loss, bone changes, and the location of possible bone growths (osteophytes).
Additional diagnostic methods that may be required to exclude other causes of pain or confirm the presence of spondyloarthrosis:
PAT.
A bone scan is used to rule out inflammation, cancer, infection or a small fracture.
CT scan
can be performed to more accurately measure the degree of narrowing of the spinal canal and morphological changes in surrounding structures.
MRI.
Magnetic resonance imaging is a method that can provide a very detailed morphological picture of the spinal cord, nerve roots, intervertebral discs, ligaments and surrounding tissues.
Treatment
Treatment of spondyloarthrosis of the lumbosacral spine is aimed at both reducing symptoms and stopping the progression of pathological processes in the joints or bones.
Most doctors take a conservative approach in the initial phase of treatment, and only then consider invasive options, but only if symptoms do not respond to conservative therapy or severe neurological signs develop.
Some of the most common treatments for lumbar spondyloarthrosis are:
- Physical therapy (PT)
is used to strengthen the muscles of the lumbar spine. Stronger muscles support the spine better and thus reduce stress on the facet joints. - Losing weight
improves symptoms simply by reducing the stress on the lumbar spine. Although weight loss can be difficult for some patients, low-impact exercise (such as swimming) combined with a low-calorie diet can often achieve the results needed to relieve pain. - Drug treatment
. Anti-inflammatory medications can reduce swelling and inflammation in the facet joint area. While over-the-counter medications such as Aleve (naproxen) or Advil (ibuprofen) can often provide sufficient symptom relief, stronger prescription medications such as Voltaren (diclofenac) and Arthrotec (diclofenac/misoprostol) are sometimes required. - The use of cold and heat
can also be effective in relieving pain in the lumbar spine. Heat can help loosen the spine before physical activity, while ice is best used after activity to reduce inflammation. - Manual therapy
. Manipulation is widely used to treat spinal diseases. Although manual therapy does not allow you to restore the full range of motion in the motor segments of the spine and restore the structure of the spine, nevertheless, manipulations can reduce pain and improve mobility. - Epidural injections
include: Injecting a steroid (cortisone or analogues) into the area of the pinched nerve. Cortisone may affect the immune system, thereby reducing localized inflammation and radicular pain.
Additional treatments include acupuncture, massage, magnetic therapy
, naturopathic remedies and other direct or indirect forms of posterior those. Although scientific evidence supporting these alternative treatments is largely lacking, most have few side effects and are reasonable options when used in conjunction with standard medical treatments.
Forecast
With timely diagnosis and proper therapy, the development of the disease can be stopped at its first stage . The difficulty lies only in the disdainful attitude of most people towards osteochondrosis or ignorance of the seriousness of the complications of this pathology.
Risks of complications
A sedentary lifestyle, heavy lifting, intense physical activity (excessive involvement in the gym, for example), a sharp change from a passive lifestyle to an active one - all these are risk factors for the appearance and complications of osteochondrosis.
The development of spinal pathologies is enhanced by metabolic disorders, poor blood circulation, and lack of fluid in the body. These factors provoke flattening of the fibrous ring and thinning of the spinal disc. And then the body turns on protection and begins to build bone tissue in order to distribute the increased load on the spine.
Complications of spondyloarthrosis of the lumbosacral spine
Osteoarthritis rarely causes severe neurological dysfunction due to compression of nerve structures.
However, over time, degenerative changes can cause spinal stenosis, which means that narrowing of the spinal canal can cause compression of the spinal cord and nerve roots.
Spinal stenosis can be a complication of spondyloarthrosis.
Cauda equina syndrome is a disorder caused by compression of the nerves in the lower spinal cord by a tissue overgrowth or intervertebral disc, a rare complication of osteoarthritis that can cause serious neurological problems.
Stages and forms of pathology
The initial form of spondyloarthrosis is asymptomatic . Symptoms of osteochondrosis or spondylosis come to the fore during diagnosis, but damage to small joints is still difficult to notice.
Signs of spondyloarthrosis begin to clearly appear after a significant proliferation of osteophytes. Bone growths change the contour pattern of the joints and narrow the lumen of the joint spaces.
There are 4 degrees of development of the disease:
- Ligaments, joint membranes and intervertebral discs lose elasticity, and the range of motion of the spine decreases.
- Increased load on the discs, partial loss of functioning of the fibrous rings.
- Increased bone growths, ligament degeneration.
- The bone growths are so large that they compress blood vessels and nerve endings and significantly limit mobility.
Surgery
In cases of severe spondyloarthrosis that cannot be treated conservatively, surgery may be indicated.
Generally, surgery is considered if the patient experiences some of the following symptoms:
- Increased radicular pain
- Increased pain or nerve irritation
- Associated disk damage
- If degenerative changes in the facet joints lead to compression of the nerve roots, then radicular syndrome occurs. This causes radicular pain, weakness, and stenosis-like symptoms. In this case, surgery may be indicated to release the nerve root and remove excess degenerative tissue that is putting pressure on the root. One such procedure is called a foraminotomy. In addition, an operation such as vertebral fusion (spinal fusion) is used.
- Vertebral fusion is a surgical procedure used to eliminate movement between adjacent vertebrae. When all other treatments fail to provide relief, spinal fusion may be a reasonable option for treating severe spondyloarthritis.
Self help
- Self-medication is important for pain caused by spondyloarthritis because pain may increase or decrease over several days.
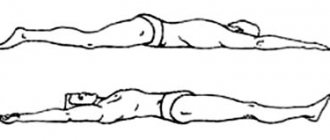
- Experts have found that even if there is pain, staying in bed for a long time is not advisable. Therefore, it is recommended to continue normal physical activity.
- However, you should avoid anything that could aggravate the condition, such as lifting heavy loads.
- Some people benefit from applying heat or ice to treat back pain.
- Sleeping with a pillow between your legs can be beneficial for lower back pain. An orthopedic mattress can also provide good support.
Prevention
In order to prevent spondyloarthrosis, it is recommended to perform the following measures:
- Attending preventive massage sessions is especially important for people leading a sedentary lifestyle.
- Engage in physical therapy – to strengthen the muscle corset and maintain the flexibility of the spine, even regular exercise is enough. Swimming is also recommended.
- Monitor the health of the spine - do not lift weights; when the first pain appears in the lumbar region, immediately consult a doctor, and do not self-medicate. If you have to sit in one position for a long time, do a warm-up every hour.
- Eat right - make sure your diet always contains foods rich in protein, calcium and phosphorus.