How does osteochondrosis of the lumbar spine occur?
Since most of the body is supported by the pelvic bone, lumbar osteochondrosis is the most common of all types of osteochondrosis.
The spine consists of the main spongy bone tissue and the intervertebral discs connecting the sections of the ridge. They consist of cartilage tissue, inside of which there is a semi-liquid core. The purpose of the intervertebral discs is to act as hinges, allowing the spine to be flexible and bend in different directions.
Osteochondrosis affects the circulatory system, when it is disrupted, the cartilage tissue of the intervertebral discs loses its strength. The process of tissue degeneration begins, the cartilage dries out and becomes brittle, begins to sag and protrude from the spinal column, unable to withstand the constant load of body weight. The affected part of the ridge begins to gradually fold and put pressure on the adjacent nerves, causing severe pain radiating to the leg. This condition is called lumboischialgia. If left untreated, the patient risks significant consequences, including paralysis of the lower body.
Diagnosis of ankylosing spondylitis
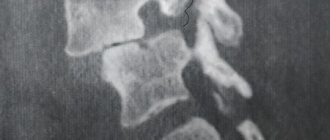
If spondyloarthritis is suspected, the rheumatologist will refer the patient for an X-ray examination of the pelvic bones, which allows visualizing the condition of the sacroiliac joints. At the onset of the disease, changes may be insignificant, but a repeat image after 1-2 years makes it possible to conduct a comparative analysis of the changes that occur as the disease progresses. A more informative method for diagnosing ankylosing spondylitis is MRI, which allows you to see changes in the joints even earlier and better.
Detection of the histocompatibility antigen HLAB27 is an important argument in favor of the diagnosis of spondyloarthritis.
Among laboratory tests, the determination of ESR and C-reactive protein (CRP) is considered mandatory (see rheumatological examination). These indicators allow you to assess the intensity of the inflammatory process.
To identify extra-articular manifestations of the disease, a biochemical blood test, ECG, echocardiography and fluorography are prescribed.
The greatest difficulty is identifying ankylosing spondylitis in the early stages. For this, it is important not only to assess the structural changes of the skeleton and laboratory test data, but also to study the family history, as well as the clinical features of the course of the articular syndrome, which requires a certain professionalism on the part of the doctor.
1 Fluorography
2 General blood test
3 Immunological blood test
Why is osteochondrosis of the lumbar spine dangerous?
The initial stage of development of lumbar osteochondrosis appears in protrusion, when the intervertebral disc begins to go beyond its limits, protruding with a root between the vertebral sections. Further, when the disease progresses, there is a violation of the integrity of the fibrous ring from which the gel-like core flows out, this condition is called intervertebral hernia. In the process of irritation and pinching of the spinal nerve, the nerve becomes inflamed, causing severe pain, that is, lumbar osteochondrosis ultimately progresses to radiculitis.
Another consequence that is likely in the absence of therapeutic measures for lumbar osteochondrosis is sciatica. Sciatica is an inflammation of the sciatic nerve. In this condition, the patient experiences severe pain in the lumbar region, which is reflected by pain in the leg, which may be accompanied by muscle numbness. Due to severe pain, a person tries to avoid putting pressure on the painful side, curving the spine, which further aggravates the blood circulation of the discs, provoking a further process of destruction.
Another possible consequence of lumbar osteochondrosis is acquired compression myelopathy, in which the spinal canal narrows due to disc proliferation, impairing blood circulation.
Due to acquired instability of the spine, the column begins to sag from the sacral area, affecting adjacent organs. Women can get problems with the uterus, ovaries, men risk impairing potency.
And finally, the most dangerous consequence of lumbar osteochondrosis is the acquisition of cauda equina syndrome. In its advanced form, the disease affects all nerves from the first to the last vertebra, resulting in complete or partial paralysis of the legs and buttocks.
Characteristics of pain in the sacrum
The nature of the pain is one of the signs that the doctor takes into account when searching for the root cause.
Pain in the sacrum combined with pain in the lower back
Pain in the sacrum may appear due to a violation of the bone structure of this part of the musculoskeletal system, or be caused by any disease. If the latter is established, then all diseases that lead to pain in the sacrum are combined with the word sacrodynia. In this case, the pain can often radiate to other parts of the spine and lower torso, and then the patient says that either the lower back, or the tailbone, or the sacrum hurts. If you have pain in the sacrum and lower back at the same time, the source of this pain can be any reason. One of the main causes of pain in both cases is osteochondrosis. But only a doctor can say exactly where this source is and for what reason it arose. This will require a careful and thoughtful diagnosis.
Pain in the sacrum on the right and left
Pain may appear on the right or left if the sacral vertebrae are displaced, for example, due to injuries or bruises. Soreness on both sides often occurs due to inflammation and infection in the area, and may be accompanied by limping or leg cramps. If pain in the lumbosacral spine appears on the right and left even while sitting, then it is necessary to urgently consult a doctor for competent treatment.
Aching pain in the sacrum
Acute and aching pain in the lumbosacral spine often occurs due to the appearance and development of pathologies of internal organs - kidneys, prostate, intestines, appendages, etc. If the pain is aching in nature and does not subside even during a period of rest (for example, in a lying position), then perhaps we are talking about an oncological disease in which metastases have already penetrated into the sacrum. Also, aching pain is characteristic of lumbosacral radiculitis, with displacement of the sacroiliac joint. The pain may radiate to the knee or the back of the thigh.
Causes of lumbar osteochondrosis
The reasons why this disease is acquired most often include the following:
- low intensity physical activity;
- diseases of the thyroid gland, cardiovascular system, gastrointestinal tract;
- high physical activity, weightlifting;
- diseases of the vertebral joints, in particular rheumatoid arthritis
- vertebral underdevelopment;
- flat feet;
- spinal injuries, especially those in the lumbar and cruciate regions;
- incorrect metabolism;
- spinal degeneration associated with age-related changes.
The risk group for lumbar osteochondrosis includes people who:
- have a curvature of the spine;
- suffer from obesity and metabolic disorders;
- are in a bent position for a long time;
- have a hereditary predisposition;
- are in an environment of increased stress;
- have sleep disorders, get little rest;
- subject the body to hypothermia;
- are representatives of such professions as loaders, builders, drivers, and also have specialties related to constant presence at the computer.
What is spondyloartitis
Ankylosing spondylitis is a chronic inflammation of the axial skeleton - the spine and iliosacral joints, leading to gradual ossification of the joints and limitation of their mobility (ankylosis - stiffness of the joint due to fusion of bones with each other). The term “ seronegative spondyloarthritis ” refers to a whole group of diseases, the common clinical manifestation of which is inflammatory damage to the spine, and the laboratory manifestation is a negative rheumatoid factor (i.e., seronegativity for this factor).
The following diseases are types of seronegative spondyloarthritis:
- Ankylosing spondylitis (ankylosing spondylitis);
- reactive arthritis;
- psoriatic spondylitis;
- spondyloarthritis in Crohn's disease;
- undifferentiated spondyloarthritis.
Common manifestations of this group of diseases include:
- pain and stiffness in the lumbar spine and buttocks (projections of the sacroiliac joints), increasing at rest and decreasing with movement;
- presence of the HLA-B27 gene;
- pain and swelling in the joints of the lower extremities, often asymmetrical;
- frequent damage to ligaments and tendons (discomfort in the heels, Achilles tendon).
A distinctive feature of ankylosing spondylitis is changes in the ligaments of the spine, their compaction and gradual ossification. This leads to the fact that the human spine loses its flexibility and becomes as rigid as bamboo.
Unfortunately, at the initial stage of the disease, spinal spondyloarthritis is confused with osteochondrosis and incorrect treatment is prescribed. It can often take several years for a correct diagnosis to be made. If treatment for ankylosing spondylitis is not started on time, it can lead to immobilization of the spine and joints, complications such as interruptions in the functioning of the heart, damage to the lungs and kidneys. Disability due to spondyloarthritis is by no means uncommon in the case of improper or delayed treatment.
Symptoms of lumbar osteochondrosis
In addition to the pain that those suffering from lumbar osteochondrosis experience, especially during periods of heavy stress, there are also other symptoms of this disease, which manifest themselves in the following:
- dull pain that moves from the source of inflammation to the leg;
- increased pain when lifting something heavy, changing body position, coughing, sneezing;
- when you stay in one position for a long time, blood accumulates in the lesion, and at the slightest attempt to change position, sharp pain occurs;
- constant tension in the back muscles;
- lumbar lumbago at the slightest hypothermia;
- numbness of the thigh, gluteal muscles, lower leg and foot;
- tingling sensation in the legs;
- arterial spasm to the point of pulselessness;
- pathology of sweat glands;
- drying of the skin in the area of pain and loss of sensitivity.
How to treat pain in the sacrum?
Any independent actions are excluded. In order to know how and with what to remove and treat the lumbosacral spine if it hurts, you need to know the cause of pain in it and have a medical education. Therefore, at the first signs, consult a doctor.
Pain relief (anesthesia)
Treatment is tailored to the cause and individual patient's situation. But most people are prescribed painkillers to relieve pain - these can be either tablets and ointments, or drugs for intramuscular and intravenous administration. If the pain is very severe, the patient may be prescribed a blockade (analgesic complex) of the painful area. The blockade is introduced into the spinal canal in the sacroiliac region or in those areas of the muscles where the main pain syndrome is concentrated.
Manual therapy, acupuncture, massage
If the lumbosacral spine hurts, how to treat it is known to an experienced specialist who, in addition to medications, can prescribe to the patient such methods of influencing the pain syndrome as acupuncture, manual therapy and massage. These methods are useful when it is necessary to correct existing bone misalignments in the pelvic area, relieve tension and swelling from the muscles, improve blood flow and oxygen supply to the muscles, joints and nearby organs, and also align the position of internal organs if they are misaligned.
Physiotherapy
Physiotherapeutic procedures for pain in the sacrum involve the use of UHF and SMT (impact on painful areas with sinusoidal currents). They help relieve swelling and inflammation in the sacrum and lower back and improve joint mobility.
Stages of the disease
The danger of cervical spondylosis directly depends on what stage it is at. Also, the approach to treatment and the set of therapeutic procedures that will be prescribed by the attending physician depend on the advanced stage of the disease. The following stages of pathology development are distinguished:
- First stage. The cervical curve is already broken, the first signs of numbness and stiffness of the neck are beginning to appear, but movements are not yet limited, osteophytes are still located within the vertebrae. This is the stage at which therapy will be most effective and most likely to lead to full recovery.
- Second stage. Osteophytes begin to gradually fuse with each other (although they do not do this completely yet). As a result, the intervertebral vertebrae begin to be seriously compressed. Mobility is limited, there is a possibility of receiving a third degree of disability.
- Third degree. Osteophytes grow together almost entirely. A person loses mobility to such an extent that he can no longer fully engage in any serious activity. He is assigned the second, or, in the case of a particularly serious development of the disease, even the first degree of disability.
Remember, the later you turn to specialists, the greater the risk that the disease will progress to a stage where its therapy will be problematic. For spondylosis of the cervical spine, treatment is most effective only in the early stages.
Doctors at the Health Workshop treat cervical spondylosis without surgery. Non-surgical methods relieve symptoms of the disease and heal the body.
Our doctor creates a course of treatment individually for each patient. The course takes into account the diagnosis, age, gender and characteristics of the patient’s body. The patient needs to undergo procedures 2-3 times a week. Treatment for cervical spondylosis will take 3 to 6 weeks. The course of treatment consists of the following procedures:
Treatment of cervical spondylosis at the Health Workshop in St. Petersburg solves several problems:
- relieves pain in the back and chest;
- improves the condition of intervertebral disc cartilage;
- strengthens muscles and improves posture;
- improves blood circulation in the spine and surrounding tissues;
- reduces the pressure of bones on each other and strengthens the bone structures of the spine.
To improve the condition of intervertebral discs, we prescribe chondroprotectors - drugs that nourish and restore disc cartilage. Massage of the collar area of the back improves blood circulation in the spine, allowing nutrients to better penetrate to the area affected by the disease. But hirudotherapy stimulates blood circulation best. To reduce pain, we use reflexology, massage, and physiotherapy.
After completing the course, the doctor gives the patient a manual with exercises to strengthen the muscles of the back and neck. The patient can come for consultations with a doctor for free within a year after completing the course.
Inflammation of a herniated disc
Inflammation of a herniated disc does not occur on its own. The nucleus pulposus, which protrudes through a fissure in the annulus fibrosus, does not undergo an inflammatory reaction. It has no nerve endings and consists mainly of protein substances with a gelatinous structure.
These protein substances have a strong irritating effect on the soft tissue surrounding the intervertebral disc. It is this circumstance that triggers the process of inflammation in a spinal hernia.
When a disc herniation becomes inflamed, the following pathological changes occur:
- muscle, tendon and ligament fibers are exposed to a foreign protein structure;
- the immune system, in order to deactivate this effect, draws inflammatory reaction factors into the lesion;
- total expansion of small blood vessels begins;
- increases the flow of lymphatic fluid;
- tissues become swollen;
- the muscles tighten to prevent compression of the radicular nerves.
During palpation, a tense muscle frame is felt. The patient feels stiffness and tension. Any movement causes increased pain.
When inflammation occurs against the background of a disc herniation, it is very important to exclude the possibility of its sequestration (separation from the nucleus pulposus). In such a situation, emergency surgery is indicated, since part of the nucleus pulposus, separated from the fibrous ring of the intervertebral disc, will constantly irritate the surrounding soft tissues and it will be almost impossible to eliminate the inflammatory process.
Symptoms of intervertebral hernia depending on its location
| Symptoms of cervical intervertebral hernia (level C2-Th1) |
|
| Symptoms of thoracic intervertebral hernia (Th1-L1 level) |
|
| Symptoms of lumbar disc herniation (level Th12-S1) |
|
Forecast
With proper and timely treatment, the prognosis is favorable . If therapy is started in a timely manner, the disease can be completely cured.
If complications and neurological disorders appear, treatment will be more difficult and longer, but following all the specialist’s recommendations will help achieve a long-term positive result.
Much is also determined by the patient’s perseverance and discipline. The prognosis will be less favorable with neurological disorders.