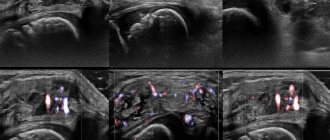
The ultrasound technique is based on the use of ultrasonic waves, which are reflected differently from tissues of different densities. This allows you to effectively examine the knee, wrist and other joints of the human body. The procedure is absolutely harmless, highly informative, and makes it possible to evaluate the smallest structures of different tissues of the articular complex.
When is an ultrasound of the elbow joint prescribed?
An ultrasound of the elbow joint is prescribed if there is:
- prolonged pain in the elbow during movement and at rest;
- limited mobility of the arm at the elbow joint;
- swelling;
- swelling in the joint area;
- redness of the skin of the elbow;
- traumatic damage to the joint;
- suspected joint effusion;
- damage to articular cartilage.
A certain group of patients, due to their professional activities, must periodically undergo preventive ultrasound of the elbow joint. This is due to the fact that during work people make constant similar movements in the elbow joint, which can lead to the development of inflammatory and degenerative processes.
Preparation
Some tests require the use of contrast, which is given to the patient intravenously before the test. Contrast allows subtle morphological changes to be detailed.
- Contrast is injected through a vein in the arm or forearm. If contrast is used, the patient may be asked not to eat or drink anything for 4 to 6 hours before the scan.
- The patient should tell the doctor if he has ever had a reaction to contrast. Before the scan, the patient may need to take antihistamines to safely use contrast.
- Before administering contrast, you must tell your doctor that you are taking a diabetes drug such as metformin (Glucophage). If the patient is taking this drug, then additional measures will be required to reduce the risk of using contrast.
- If the patient weighs more than 300 pounds (135 kg), you need to find out how much weight the CT scanner is rated to carry. Excess weight may cause damage to the scanner's working parts.
Ultrasound of the elbow joint: what it shows
Injuries
- Injury to the collateral ligaments by itself is rare, but occurs in combination with other injuries.
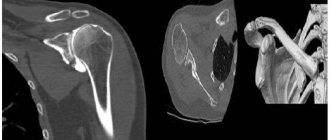
- A fracture can occur in the condyles of the humerus, processes of the ulna, or in the head of the radius.
Bursitis
Bursitis involves inflammation of the joint structures, as well as nearby muscles, tendons and nerve fibers. In this case, a pathological effusion forms in the bursa. The reasons for its appearance are:
- constant hand overload;
- injuries to bones, joints or tendons in the elbows;
- inflammation (arthritis, gout);
- the presence of pyogenic microorganisms in the body;
- autoimmune diseases;
- the presence of specific diseases - gonorrhea, syphilis, tuberculosis;
- intoxication.
Epicondylitis
A disease that occurs as a result of physical overload and overstretching of the tendons, characterized by a disruption of the normal structure in the area of the periosteum and tendon and manifested by pain. The following factors can trigger the development of epicondylitis:
- frequent exercise, long workouts, monotonous movements;
- injuries;
- the patient has congenital connective tissue dysplasia.
Hematomas
Hematoma, or bruise, is damage to blood vessels, bleeding into soft tissue.
Hemarthrosis is characterized by a uniform defiguration of the joints, hemorrhage stretches the joint capsule, its contours are smoothed out, and it takes the shape of an ellipse or ball.
With hemarthrosis, in contrast to subcutaneous and intermuscular hemorrhages, function is significantly more impaired.
If hemarthrosis of the elbow joint is established, treatment should only be carried out under the supervision of a specialist.
Tendinitis
Tendinitis is an inflammation of the tendons, which is accompanied by a number of changes in the structure and degenerative restructuring of the inflamed areas.
The causes of tendon inflammation are associated with its chronic overload or age-related changes.
Before starting to treat tendonitis with drugs, experts recommend that patients reduce the load on the muscles whose tendons are inflamed.
Tendon injuries
- A rupture of the biceps tendon occurs during severe physical activity, such as sports.
- A triceps tendon rupture causes pain in the back of the elbow. When raising the arm above the head, extension does not occur in the elbow joint or occurs only with significant effort.
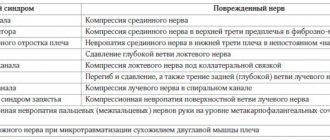
Cubital tunnel syndrome (ulnar nerve compression syndrome)
In this article we will talk about cubital tunnel syndrome, which is sometimes called cubital tunnel ulnar nerve compression syndrome. Nerves carry impulses from the brain and spinal cord to all organs of the body, and these impulses also give signals to muscles to move and are responsible for the sensitivity of the skin. When a nerve is compressed, then, accordingly, it cannot work normally and the conduction of nerve impulses is disrupted. Naturally, the disturbance in the conduction of nerve impulses is stronger when the pressure on the nerve is greater.
We are all familiar with the situation when, having hit the back-inner part of the elbow on something hard, we feel a sharp pain, a shooting along the forearm, which can reach the fingers. In such situations, we just hit the ulnar nerve, and the lumbago from the elbow down to the little finger goes exactly through the area that the ulnar nerve provides impulses (innervates). Yes, this is a strong and sharp pain that occurs with a single blow to the ulnar nerve, but imagine what will happen if you constantly press on the ulnar nerve? Not as hard as when hit, but a little and constantly? It is this situation, when the ulnar nerve is compressed in the canal, that is called compression syndrome, and the resulting disturbance in the conduction of impulses along the nerve in such a situation is called ulnar nerve neuropathy. Ulnar nerve neuropathy itself can occur due to other reasons, for example, due to compression in other places (lower or higher), but if the ulnar nerve is compressed precisely in the cubital canal, then, accordingly, in this case the diagnosis can be formulated as follows: neuropathy of the ulnar nerve due to compression syndrome in the ulnar (cubital) canal.
Cubital tunnel syndrome is the second most common cause of compression neuropathies (ie, pain due to nerve compression) after carpal tunnel syndrome.
Anatomy
The ulnar nerve emerges from the cervical plexus of nerves, travels down the arm and into the fingers. The ulnar nerve is responsible not only for the sensitivity of the skin of the little finger and the adjacent half of the ring finger, but also gives commands to some muscles that move the hand (the interosseous muscles that extend and spread the fingers to the sides, and the muscles that adduct the thumb). If the ulnar nerve is damaged, gripping with the hand will be difficult.
On its way, the nerve bends around the elbow from behind and slightly inwards - this place is called the cubital (ulnar) canal. This canal is formed by muscle tendons (flexor carpi ulnaris, flexors and pronators), ligaments and bone (internal epicondyle of the humerus and olecranon).
Ulnar nerve and cubital tunnel
Causes of compression of the ulnar nerve in the cubital canal
There is no clear and single important cause of compression of the ulnar nerve in the cubital canal. There are several reasons for the development of this syndrome, the importance of each of which varies from person to person.
It is believed that one of the most common causes of compression of the ulnar nerve is repeated trauma. For example, during repeated monotonous movements or when playing sports. Tension of the flexor carpi ulnaris (the beginning of this muscle in the form of an arched tendon forms one of the walls of the cubital tunnel) leads to compression of the ulnar nerve. Of course, normally the tension of this muscle will not lead to compression of the nerve, but if there is a lot of movement, then inflammation will develop - the edges of the inflamed tendon arch become thicker, the canal space, accordingly, becomes smaller, and the nerve will begin to hurt. Often this mechanism for the development of neuropathy occurs during the bench press, when the hand holding the barbell is tense for a long time.
The ulnar nerve can also be compressed by external reasons - if, for example, you like to put your elbow on the side of the car door next to the glass.
Another common cause is a change in the anatomy of the cubital canal. After fractures of the condyles of the humerus, fractures of the olecranon, the formation of cysts, bone spurs, the space of the cubital canal may become narrower, which will lead to compression of the ulnar nerve.
Cubital tunnel syndrome can also appear after a severe injury to the elbow.
Symptoms
Cubital tunnel syndrome most often manifests itself (not necessarily all of these symptoms are present at the same time):
- A feeling of stiffness, pain, numbness in the little finger and in the half of the ring finger adjacent to it.
- Weakness and pain when gripping with the hand and extending the fingers.
- Pain in the cubital canal itself, a feeling of tightness in the elbow.
These problems may begin gradually and progress. Often complaints are stronger in the morning, after sleep, when the elbow has been in a stationary, often bent position for a long time - many people like to place their bent arm under their head or under a pillow. In this case, problems may arise when moving the hand - it is difficult to pick up a kettle, type on the keyboard, play the guitar, etc. After a few minutes to hours, the severity of these symptoms usually decreases. If cubital tunnel syndrome is not treated promptly, the problems may worsen and the complaints become permanent.
If the initial symptoms of cubital tunnel syndrome do not go away within a few weeks, you should consult a doctor.
Diagnosis
The doctor examines the hand, forearm, elbow and shoulder, and neck, trying to determine the level at which compression of the ulnar nerve occurs. The sensitivity of the fingers, certain movements of the hand, Tinnel's symptom (increased symptoms when tapping the fingers along the cubital canal) are checked.
A doctor's examination for cubital tunnel syndrome can be unpleasant or even painful, but this is necessary to clearly determine the cause of the pain.
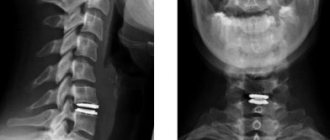
In most cases, the diagnosis can be established only by examination, but sometimes, in doubtful cases, the doctor may prescribe an additional examination that will determine the presence of non-standard causes of compression of the ulnar nerve (bone spurs, fractures and their consequences, arthritis, etc.) . The most commonly prescribed are x-rays, computed tomography and MRI.
X-rays show bones, CT scans also show bones, but in more detail, and MRI (magnetic resonance imaging) shows soft tissues (muscles, ligaments, cartilage, etc.). Sometimes the doctor uses ultrasound to make a diagnosis.
You don’t need to prescribe these studies yourself before an examination or consultation with a doctor - in most cases, this simply leads to a pointless waste of your time and money, but it can also lead you down the wrong path, because the conclusions of these studies should only be evaluated together with the examination!
In some cases, your doctor may order electromyoneurography (EMNG), which can evaluate the degree of nerve conduction disturbance and sometimes help determine the level at which the nerve is being compressed (neck, shoulder, elbow, forearm, or hand). Electromyoneurography is also useful in those rare cases when nerve compression occurs at two levels simultaneously.
Treatment
In most cases, in the early stages, when symptoms are inconsistent, conservative treatment is effective, i.e. non-surgical treatment .
Conservative treatment includes limiting exercise, stopping training, and anti-inflammatory drugs.
It is necessary to eliminate repeated repetitive monotonous movements, give up the habit of placing your elbow on the side of the car door next to the window. If your job does not allow you to temporarily abandon monotonous elbow movements, then give yourself breaks more often.
If you work at a desk, place something soft under your elbow. Do not let your elbow hang over or rest on the edge of the table when using the mouse or keyboard.
In other words, you need to eliminate as much as possible all those movements that cause pain or discomfort.
If you sleep with your bent arm under your head or under a pillow, try tying a roll of a terry towel to the front (flexor) surface of your elbow to limit flexion. This type of nighttime bandaging can be effective not only when you sleep with your arm bent, but also in other cases of cubital tunnel syndrome.
It is important to use non-steroidal anti-inflammatory drugs, for example, Voltaren gel 3-4 times a day for 2-3 weeks. You need to smear your elbow with anti-inflammatory drugs constantly, regardless of whether there is pain or not. The fact is that these drugs not only relieve pain, but fight the inflammation itself, which is accompanied by swelling, thickening of the soft tissue component of the walls of the cubital canal, and, accordingly, compression of the nerve itself.
In some cases, vitamin B-6 tablets can help treat cubital tunnel syndrome.
Conservative treatment usually gives effect within 3-4 weeks, but sometimes, in persistent cases, it is continued for up to 12 weeks. If sufficient improvement does not occur within 12 weeks, surgery is performed.
Surgery
Surgery may be necessary not only in cases where, after 12 weeks, conservative treatment has not brought sufficient results, but also when:
- despite treatment, complaints due to nerve conduction disorders progress
- initially the complaints were constant and quite pronounced
- there are gross anatomical disorders of the cubital canal (consequences of fractures, the presence of a plate fixing the fracture, etc.).
The operation belongs to the category of “simple”, if, of course, this can be said about operations in general.
The operation is performed under anesthesia - under general anesthesia, intravenous sedation, or regional anesthesia is used, which numbs only one arm.
There are several options for operations that are performed from an incision 5-8 cm long.
Simple decompression. During this operation, part of the thickened canal walls is removed and the tendon arch is dissected. This operation is technically simple, but, unfortunately, it does not always give a lasting effect and after a certain period of light the complaints return again. Sometimes decompression is supplemented by resection (partial removal) of part of the epicondyle of the humerus.
Nerve transposition. The nerve is completely removed from the cubital canal and moved 3-4 centimeters anteriorly. If the nerve is transplanted into the space between the muscle and the subcutaneous fat, then this operation is called anterior subcutaneous transposition. And if the nerve is moved deeper, under the muscle, then, accordingly, the operation is called anterior axillary transposition. The choice of transposition option depends on many features.
According to modern statistical studies, simple decompression and transposition of the nerve are equally effective, but, nevertheless, this does not mean that it is necessary to abandon the relatively complex transposition in favor of simpler decompression.
Scheme of anterior axillary transposition of the ulnar nerve when it is compressed in the cubital canal
After surgery, the elbow is usually immobilized for 10-14 days after subcutaneous transposition and 20-25 days after axillary transposition. After this, movements begin, but after axillary transposition, restrictions on the intensity of physical activity remain for up to 4-6 weeks.
Full recovery from surgery may take several months. It is important to note that in general, a correctly performed operation is very effective, and the long period of gradual recovery is due to the long restoration of nerve cells. Yes, contrary to the well-known proverb, nerve cells are still restored, but very slowly.
The growth rate of axons (processes) of nerve cells is one millimeter per day, and if the distance from the elbow to the tip of the little finger is 30-40 cm, i.e. 300-400 mm, then complete recovery may take 300-400 days. Fortunately, the condition of the nerve is improving gradually, and there is no situation where on the 299th day everything is still bad, but on the 300th everything is fine. In severe cases, when there is neurogenic muscle contracture, i.e. the muscles have already died, deprived of nerve impulses, a complete solution to the problem is impossible, and it is possible to try to restore movements only with the help of other, more complex operations.
| The author of the article is Candidate of Medical Sciences Sereda Andrey Petrovich |
How is an ultrasound examination of the elbow joint performed?
Ultrasound examination of the elbow joint: technique
The patient takes a comfortable position on the couch (sitting or lying), and the doctor treats the examination area with a special gel.
A sensor is applied to the skin, and all information is sent to the computer through it. It is processed and displayed on the monitor in the form of a black and white schematic image.
The ultrasound technique of the elbow joint is painless, the procedure lasts approximately twenty minutes.
Difference between MRI and ultrasound
Before we look at how MRI of joints differs from ultrasound, it is necessary to give clear definitions of each procedure.
Ultrasound examination is a diagnostic technique; scanning is carried out using ultrasonic waves. As a result, the doctor examines the condition of soft tissues and organs. The procedure is harmless. In this case, the doctor reads information about the condition of the meniscus, periarticular soft tissues, and cruciate ligament, but is not able to scan the bones and lungs. MRI is used to study bone tissue.
An MRI is a large magnet that produces magnetic waves within a specific magnetic field. During an MRI scan, the doctor examines all tissues and organs. The procedure can be used repeatedly and allows one to study the dynamics or consequences of an injury or disease. The question of which is better: MRI or ultrasound is not relevant. The difference is in information content, reliability and price.
Decoding the results
During the procedure, special attention is paid to:
- The structure of bone surfaces - whether they are smooth or not. The same applies to the contours of cartilage tissue.
- The condition of the protrusions on the surface of the condyles - both lateral and medial.
- Features of nerves and tendons.
- The thickness of hyaline cartilage and the uniformity of its structure. Normally, its thickness should be no more than 2 mm.
- The presence of fluid in the projection of the ulnar fossa. If effusion is detected, then we are talking about inflammation of the synovial membrane.
- The presence of fluid under the olecranon. If it is, then there is inflammation of the synovial bursa. If the disease is advanced, the liquid on the screen will be heterogeneous.
- Inflammation of the tendon. If one of the tendons is inflamed, the diagnostician will pay attention to its thickening and reduced echogenicity. With the chronic nature of the disease, calcifications form in the tendon, and the contours lose clarity.
The data obtained should be discussed with the attending physician, who will not only prescribe treatment, but also determine additional diagnostic measures to clarify the nature of the disease.
Difference between X-ray and ultrasound
X-ray scanning is used in traumatology; during the examination, bone tissue pathologies are identified. During the ultrasound scanning process, the condition of bones, ligaments, cartilage, synovial bursa, and articular surfaces is assessed.
The advantage of ultrasound diagnostics is that it is harmless to the human body. X-rays affect the body with ionizing radiation and are prohibited for pregnant women. The radiation exposure received during the examination is taken into account.
Procedure
The scan is performed by an x-ray technician, and the results are interpreted by a radiologist.
Before the procedure:
- Remove all jewelry and any other metal objects.
- Remove some clothing to expose the examination area
During the study:
- The patient will be asked to lie still on a table attached to the CT scanner.
- Contrast material is injected into a vein immediately before tomography
- The scanner table moves into the round hole of the tomograph and moves slightly while scanning. The patient may hear a clicking or buzzing sound when the scanner operates.
- The patient is alone in the scanning room, but the x-ray technologist will observe the patient through an observation window.
- The patient must remain still during the scan. Movement (even small movements) can cause blurry images. The patient may be advised to hold their breath for a short period of time.
- A CT scan of the elbow joint takes from 10 to 30 minutes.
Indications for use
Ultrasound examinations can be prescribed to people with different health conditions. Indications for an ultrasound of the elbow are:
- local edema and tumors;
- pain that bothers you for a long time;
- redness on the skin;
- stiffness when moving;
- injuries;
- neoplasms;
- rheumatism;
- effusion in the joint part or the prerequisites for it;
- damage to the cartilaginous joint.
Since the technique is considered harmless and quite safe, it has no contraindications.
Patient reviews
I'm a former athlete. From personal experience I can say that tennis is not such a harmless sport. Over 10 years of competition and training, there was everything from dislocations and muscle strains to wrist fractures. Ultrasound has always helped determine the degree of shoulder joint dislocation.
Dmitry, Mytishchi
I believe that ultrasound of internal organs is a useful and at times irreplaceable procedure. One day I experienced a dislocated shoulder. Treatment was prescribed only after undergoing hardware diagnostics.
Nadezhda Petrovna, Stavropol
This winter has brought me a lot of worries. The ice was terrible. One terrible day, going outside, I couldn’t stand on my feet and fell. The bruise of the soft tissues of the arm turned out to be severe; moving the limb was very painful. I turned to a surgeon at a local public clinic. The specialist sent me for an ultrasound on the same day, after which he prescribed treatment.
The situation ended well for me.
Thanks to modern medicine and ultrasound techniques of the elbow joint. Do not self-medicate in such cases. You should trust only qualified specialists. Ira, Ufa