Osteochondrosis and regular back pain affect 60–80% of the population over 30 years of age. Untreated osteochondrosis reduces the quality of life and can lead to disability and disability, so it is important to recognize it in the initial stages of development and seek help from a doctor.
In the article we will talk about osteochondrosis, its symptoms and diagnostic methods, as well as how to distinguish osteochondrosis from other diseases that manifest as back pain and what to do if signs of spinal osteochondrosis appear.
What is spinal osteochondrosis?
Osteochondrosis is a chronic disease in which the core of the intervertebral disc is gradually destroyed. Over time, damage to the intervertebral disc involves other structures of the spine in the pathological process and leads to disorders of the musculoskeletal system and nervous system. Osteochondrosis is also characterized as premature aging of the articular system or as a pathology resulting from damage to the vertebrae, for example, after injury.
The development of osteochondrosis is influenced by many factors, so researchers have systematized the reasons that explain the origin of the disease:
- involutive - inflammatory processes and other damage to the spine lead to premature aging of cartilage, for example, as a result of a sedentary lifestyle;
- degenerative – disorders in the intervertebral discs occur as a result of a failure of metabolic processes, for example, as a result of an unbalanced diet and alcohol abuse;
- dysmetabolic - osteochondrosis occurs due to malnutrition in the intervertebral cartilage due to the fact that with age the number of blood vessels that supply blood with nutrients decreases.
The development of osteochondrosis is a cascade in which one pathological process triggers another. For example, due to age-related changes and a decrease in the number of vessels in the disc, nutrition is disrupted, which leads to a malfunction in biochemical processes and damage to the intervertebral disc.
As degenerative and dystrophic changes develop in the spine, muscle tone and the functioning of the nerve roots that exit the spinal cord through natural openings in the vertebrae are disrupted. This leads to consequences on the nervous and musculoskeletal systems.
Spasm of cerebral vessels in osteochondrosis
Temporary or permanent spasm of cerebral vessels during osteochondrosis is a very dangerous condition. With a slight spasm of blood vessels due to osteochondrosis, the brain in a chronic mode does not receive sufficient amounts of nutrition and oxygen for full activity. Foci of sclerosis of the medulla develop. This can cause the development of encephalopathy even at a young age.
Patients with poor brain function are at risk of becoming disabled and incapacitated within a short period of time. With osteochondrosis, the brain may suffer from a sudden acute spasm of the cerebral blood vessels. If an ischemic stroke develops, then long-term (up to a year) rehabilitation will be required in the future in order to restore all lost functions.
With osteochondrosis, cerebral vessels suffer not only from periodic spasms. If their course is disrupted, they become tortuosity, lengthen, or slow down the speed of blood flow, the processes of formation of cholesterol plaques can begin. Persons with cervical osteochondrosis are at risk for developing cerebral atherosclerosis already at the age of 40–50 years.
Symptoms of spinal osteochondrosis
Osteochondrosis is a chronic disease with periodic exacerbations that are provoked by injuries, a sedentary lifestyle, heavy lifting, hypothermia and psycho-emotional stress. The most common and characteristic symptom for dystrophic disorders in the core of the intervertebral discs is regular aching back pain in different segments: in the neck, chest and lower back.
There are two types of symptoms of osteochondrosis: reflex and compression. Reflex symptoms develop due to irritation of the spinal cord roots. They manifest themselves in the form of spasm or vasodilation, muscle twitching, and weakening of muscle strength. Compression symptoms develop due to compression (usually caused by a herniated disc) of the nerves and manifest as loss of sensation in the affected segment (neck, arms or lower back).
The following symptoms are also characteristic of osteochondrosis:
- tension and soreness in the muscles of the neck and back;
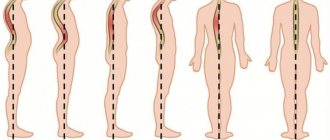
- curvature of the spine to the side, back or forward;
- disturbance of sensitivity and nervous regulation: there is a feeling of goosebumps crawling on the skin, changes in heat and cold on the skin of the back and limbs, numbness in the arms or legs;
- weakening of the muscle strength of the limbs;
- frequent urination – up to 10–12 times a day.
Headaches and dizziness due to cervical pathology
Headache due to diseases of the cervical spine.
When the cervical spine, its ligaments and neck muscles are damaged, the first thing that occurs is limited mobility due to pain.
The most common causes of this are osteochondrosis, arthrosis and spondylosis deformans. Vertebrogenic headaches can be caused by degenerative processes in the intervertebral discs, instability of the cervical spine, uncovertebral and other arthrosis, osteophytes, as well as protrusions and prolapses of the discs.
Characteristic reflex tension of the muscles of the neck and occipital region. These pains largely depend on the position of the head during the day and during sleep. They intensify with an uncomfortable position of the head and neck, sneezing, walking and coughing. Constant heaviness in the head often accompanies those who Spends a long time in front of a computer monitor without changing position. Pain also occurs in those who often experience psycho-emotional overload.
Vertebrogenic vertigo is pathogenetically associated with degenerative changes in the cervical spine. Proprioceptors of the neck are involved in coordinating movements of the eyes, head and body position, that is, in spatial orientation. The neck contains formations that directly control balance, the state of vascular structures (carotid and vertebral arteries), as well as the cardiovascular system. Neck movements are also invariably associated with head movements. Thus, dizziness resulting from neck movement may be due to disturbances in vestibular, visual, vascular, neurovascular, or cervicoproprioceptor mechanisms.
The diagnosis is established on the basis of X-ray confirmation of problems with the spine (including the presence of cervical osteochondrosis, protrusions or herniations of intervertebral discs, anomalies in the development of vertebrae, etc.), as well as in the presence of a characteristic clinical picture that includes the following symptoms
• Pain in the neck, radiating (radiating) to the back of the head
• Muscle tension in the occipital region
• Dizziness
• Noise in ears
• Flashing of flies before the eyes
• Limitation of head turns
Diagnostics
• radiography of the cervical spine in two projections
• Doppler ultrasound of the neck and head vessels with functional tests (head rotations)
• MRI of the brain and craniovertebral junction to exclude focal pathology. Treatment of headaches.
Treatment should be comprehensive, as is the treatment of any problem with the spine.
• muscle relaxants and non-steroidal anti-inflammatory drugs
• post-isometric relaxation of neck muscles and manual therapy
• reflexology
• various physiotherapeutic techniques (SMT, darsonval, electrophoresis)
Prevention of headaches To avoid relapses and exacerbations, you should also take into account some recommendations
• Try to avoid drafts and hypothermia, as this will lead to even greater muscle tension and will serve as the beginning of an exacerbation of the disease.
• If you have long-standing cervical osteochondrosis, then circular movements of the head are contraindicated for you. Such movements put too much stress, especially on the lower cervical spine (when throwing the head back), which can lead to increased pain.
• Remember the rule of five NOTs:
-o don't throw your head back
-do not turn your head in the direction where your neck hurts
-do not tilt your head when lifting weights
-do not write or read with your head down
- do not sleep on a pillow that is too high
• It is important to constantly monitor your posture - it should be correct no matter what you are doing at the moment - sitting, lying, walking.
• When there is no acute period of the disease, it is necessary to do therapeutic exercises, which are aimed at relieving tension in the cervical spine.
Where can osteochondrosis lead to?
Pain due to osteochondrosis is localized not only in the back. They spread to the upper and lower extremities. To your feet:
- buttocks;
- back and sides of the thighs;
- lower leg and inner ankle;
- back of the feet;
- toes;
- heels.
Pain can also spread into the arms to:
- deltoid muscle;
- the outer edge of the hand, down to the fingers;
- back of the hand;
- three middle fingers;
- ring finger and little finger (rare).
Symptoms of osteochondrosis and brain damage
Osteochondrosis, with a negative effect on the brain, gives certain clinical symptoms. The first signs that the brain is suffering from osteochondrosis are symptoms of ischemia or oxygen starvation. In each patient they can manifest themselves with varying degrees of intensity.
“Osteochondrosis of the head” can give the following symptoms:
- severe tension headaches (they usually occur after a busy day at work or after sleeping in an uncomfortable position, when the muscles of the neck, collar area and back of the head become numb);
- dizziness of an orthostatic nature (when changing body position, for example, when getting up from a sitting or lying position);
- tinnitus associated with insufficient patency of the cervical cerebral vessels;
- decreased mental performance, concentration, and ability to solve serious problems;
- constant weakness, drowsiness, apathy, low mood;
- depression, suicidal thoughts;
- panic attacks;
- interruptions in heart function.
With the development of acute vascular insufficiency, an ischemic stroke may occur. In this case, a person experiences numbness of the upper and lower limbs on one side of the body, numbness of the facial muscles, speech impairment, loss of consciousness (with extensive strokes). May be fatal. In milder cases, paralysis of the body is observed, which requires long-term rehabilitation.
How is osteochondrosis diagnosed?
Diagnosis of osteochondrosis is based on a survey, physical examination and instrumental examination methods. Specific examination methods are determined during consultation.
The doctor begins the diagnosis by collecting an anamnesis: identifying the probable causes of back pain, establishing the location of the pain and its duration, identifying the presence of concomitant pathologies, for example, allergies, congenital diseases and drug intolerance. Next he moves on to inspection. The physical examination is performed standing or sitting. The doctor can identify the curvature of the spine, evaluate muscle strength and reflexes, and look at the color of the skin. To detail the picture of the disease, you need to consult with related specialists: a neurologist, neurosurgeon, oncologist, rheumatologist and phthisiatrician.
A neurologist makes a diagnosis of “osteochondrosis” if:
- regular aching back pain;
- increased pain when lifting weights, sneezing, coughing;
- numbness and a feeling of aching in the joints;
- decreased range of motion in joints;
- muscle spasm;
- damage to the nerve roots;
- changes on an x-ray of the spine.
Do you need an X-ray of the spine?
X-ray of the spine or spondylography is one of the mandatory examinations for osteochondrosis, with the help of which structural disorders of the spine can be identified. Spondylography allows you to find pathological changes, for example, thinning of the intervertebral disc. Typically, for the cervical, thoracic and lumbosacral spine, x-rays are taken in two (and sometimes three) projections for greater detail.
Computed tomography and magnetic resonance imaging make it possible to identify pathologies associated with osteochondrosis: disc herniation and reduction of the lumen of the spinal canal, protrusion of the intervertebral disc into the spinal canal and compression of the spinal cord.
Osteochondrosis of the cervical spine
With cervical osteochondrosis of the spine, two main symptoms appear - cervicago and cervicalgia. Cervicago is an acute painful cervical lumbago that appears when moving the head and due to tension in the muscles of the cervical spine. Cervicalgia is aching and severe pain in the neck. Cervicalgia is accompanied by paresthesia - a disturbance of sensitivity in the form of numbness and a sensation of crawling on the skin.
If damage to the nuclei of the intervertebral discs of the neck progresses, cervical radiculitis appears - painful sensations in the back of the head. The pain is characterized by regularity; in addition, it intensifies occasionally, especially when moving the head.
This triad - cervicalgia, cervical radiculitis and cervicago - can be complicated by the syndrome of nocturnal hand dysesthesia, in which sensitivity is distorted. For example, a warm object may feel cold to your fingers, but if you shake your hands, sensitivity is restored.
Is osteochondrosis curable or not?
A modern sedentary lifestyle has led to the emergence of osteochondrosis (from other Greek ὀστέον, meaning bone and χόνδρος, meaning cartilage). People facing this disease are wondering whether it is possible to treat this disease or whether it is impossible. We will try to give answers in this article.
The concept of osteochondrosis and its symptoms
Osteochondrosis is a chronic disease accompanied by pain in the back and neck, difficulty in flexion and extension, numbness in the hands and other symptoms. There are few adults who have not experienced similar manifestations of it. The danger of this disease lies in the fact that it develops over a long period of time, the initial signs, as a rule, go unnoticed, and a visit to a specialist occurs only when serious symptoms of the disease appear.
As a result of a number of reasons, the spine, which has the ability to withstand heavy physical loads, may begin to experience dystrophic changes in the articular cartilage. Most often, this happens in the intervertebral discs, which connect the hard vertebrae to each other and take on the main load, protecting the vertebrae from damage. When the discs stop performing their functions, depreciation is disrupted and the shape of the spine changes.
Causes of the occurrence and development of osteochondrosis
As long as a person moves, his body develops normally, without causing any health problems. The main cause of osteochondrosis is physical inactivity, in which body functions aimed at adaptation and protection begin to gradually decline (back muscles weaken, this leads to displacement of the vertebrae), which soon leads to illness.
Other causes of the occurrence and development of osteochondrosis include the following:
- heredity;
- overweight;
- poor nutrition, which leads to the loss of microelements needed by the body;
- spinal injuries
(fractures and bruises); - sudden lifting of weight;
- incorrect posture and, as a result, curvature of the spine
; - constant stress and nervous tension;
- a sharp decrease in loads as a result of stopping sports activities.
Consequences of the disease
This disease can lead to:
- cerebral stroke due to impaired oxygen saturation;
- decreased immunity;
- limited mobility in the neck area;
- hypertension, which contributes to the development of heart attack or stroke;
- hypotension, accompanied by lethargy, dizziness, fainting, decreased performance;
- frequent pain in the back of the head, temples and forehead;
- numbness in the hands;
- problems with vision and speech.
That is, we see that osteochondrosis causes a lot of trouble for a person and reduces his quality of life. Therefore, specialized treatment is required.
Is it possible to cure osteochondrosis?
According to some doctors, it is impossible to defeat the disease. At the same time, others say that it is possible by using medications, using traditional methods, massage, manual therapy, and sets of therapeutic exercises.
As scientists have found, if you start treating the disease in the early stages, it is possible to completely restore the functions of the spine. But it is necessary to constantly carry out preventive measures, including:
- maintaining an active lifestyle;
- avoiding heavy lifting;
- engaging in reasonable physical exercise, swimming;
- proper nutrition.
In an advanced stage, when the disease has reached stages 3-4, there is no longer talk of a complete recovery, since in this case the shape of the spine changes as a result of the formation of bone growths, which can only be removed surgically.
But in this case, do not despair.
It is imperative to undergo the necessary course of treatment by contacting specialists. If possible, get a referral for spa treatment. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Osteochondrosis of the thoracic spine
Osteochondrosis of the thoracic spine is most characterized by painful lumbago in the chest area (dorsalgia). Chest pain worsens with moving your arms, sneezing, coughing, and lifting heavy objects. Most often the pain is girdling. Paresthesia also often occurs in the chest. Sometimes damage to the nuclei of the intervertebral discs can be disguised as diseases of the internal organs, for example, gastritis or angina, since pain can be localized in the upper abdomen and in the heart area.
Thoracic osteochondrosis
Pathology of the thoracic spine is characterized by pain throughout the chest, in the back, interscapular region, armpit and hands. Often pain with thoracic osteochondrosis spreads along the intercostal nerves, becoming encircling.
Pain during movements leads to limitation of their amplitude, the person feels constrained. Along with motor disorders, all types of sensitivity, both superficial, cutaneous, and deep, proprioceptive, also suffer.
The pathological process may also involve internal organs that are innervated by the roots of the thoracic spinal cord. Thus, pain may often appear in the heart and behind the sternum, pain in the right hypochondrium, in the liver area, and the functioning of the digestive system is disrupted.
How to distinguish between heart pain or osteochondrosis?
Pectalgic syndrome is pain in the anterior chest wall, which may resemble pain in the heart. Pectalgia can be a sign of both osteochondrosis and heart problems.
However, pain during angina and heart attack differs from pectalgic syndrome due to osteochondrosis. The peculiarity of pain during angina pectoris and myocardial infarction is that it is of a compressive nature and spreads to the left shoulder blade, arm and jaw.
Pectalgic syndrome in osteochondrosis does not spread beyond the boundaries of the anterior chest wall, does not radiate to the arm and shoulder blade, and is not accompanied by fear of death. However, these are only subjective feelings. Therefore, to rule out cardiac pathology, you need to see a doctor and have an electrocardiogram done, which will reveal rhythm disturbances or signs of myocardial infarction.
If the pain begins to spread to the left shoulder blade, arm, jaw, is accompanied by a feeling of fear, is not eliminated by taking nitroglycerin and lasts more than 10–15 minutes, you need to call an ambulance.
Why is lumbar osteochondrosis dangerous?
With osteochondrosis of the lumbar region, lumbago or lumbodynia most often occur - regular lumbago and aching pain in the lumbar region. Due to constant pain, movements are limited: a person cannot bend down, do exercises or lift a heavy object.
Lumbago can go away on its own. However, they are prone to exacerbations, and each exacerbation indicates additional displacement of the intervertebral disc into the spinal canal. If the destruction of the intervertebral disc progresses, lumbosacral radiculitis is formed, accompanied by lower back pain that radiates to the buttocks and thighs.
What is the difference between osteochondrosis and osteoarthritis?
Osteochondrosis and osteoarthrosis (spondylogenic osteoarthritis) belong to the class of diseases of the musculoskeletal system. However, there is a key difference between them: with osteochondrosis, the core of the intervertebral disc is affected, and with osteoarthritis, the intervertebral joints are affected. This makes the difference in symptoms and treatment.
With osteochondrosis, back pain is regular and aching, manifests itself at rest and intensifies with movement, and with spondyloarthrosis, the appearance of pain is associated with extension and flexion of the spine. Typically, the pain syndrome with osteoarthritis of the spine is one-sided and has a cramping nature. Also, spondylogenic osteoarthritis is characterized by morning stiffness, which lasts from 30 to 60 minutes.
VSD or cervical osteochondrosis?
Vegetovascular dystonia is a syndrome in which the functioning of the autonomic nervous system is disrupted. VSD is a functional disorder in which there are no structural changes either in the spinal column or in the nuclei of the intervertebral discs.
Vegetative-vascular dystonia has a mental origin - it is a neurosis that is associated with intrapersonal conflicts or childhood traumas. Externally, VSD and osteochondrosis can be similar to each other: headaches, dizziness, pain in the anterior chest wall.
To distinguish diseases, it is necessary to carry out instrumental diagnostics - x-rays of the cervical spine and other parts, computed tomography and magnetic resonance imaging. As a result of diagnosis, there will be no organic changes in VSD, unlike osteochondrosis.
Why do headaches occur?
As we have already found out above, cervical-cephalic osteochondrosis is a non-existent diagnosis. Osteochondrosis of the head and neck is a condition in which the following pathological changes occur in the human body:
- the cartilage tissue of the intervertebral discs, under conditions of constant tension of the cervical and collar muscles, suffers from a lack of fluid and nutrients;
- dehydration of the fibrous ring occurs and it begins to take fluid from the nucleus pulposus located inside it;
- this leads to a decrease in the height of the intervertebral disc;
- there is pressure on the radicular nerves, which provokes stiffness and overstrain of the surrounding muscles;
- there is a change in the patency of the cerebral blood vessels - less blood begins to flow through them to the structures of the brain;
- against the background of oxygen starvation, headaches, dizziness, drowsiness begin to develop, decreased concentration and concentration, and decreased performance;
- with a long-term process of tension in the neck muscles, degeneration of the vascular wall is observed, the course of the artery becomes tortuous and difficult;
- foci of ischemic deformation of the substance are formed in the structures of the brain;
- this provokes the appearance of clinical symptoms of depression, decreased mental activity, etc.
In severe cases, patients suffer from panic attacks, disruption of the autonomic nervous system, depression with suicidal thoughts.
Osteochondrosis of the cervical and head is a potentially dangerous condition that disrupts the functioning of some vital internal organs. In particular, if the vagus nerve, which leaves the brain through the foramen ovale, is damaged, the heart rhythm may be disrupted. When the nerves that control the functioning of the coronary circulatory network are damaged, the blood supply to the heart muscle deteriorates. Coronary heart disease and angina pectoris develop. These diseases can provoke acute heart attack and myocardial infarction. Patients with cervical osteochondrosis are at risk of developing hypertension or becoming paralyzed when spinal canal stenosis develops. Do not delay visiting a doctor if signs of cervical osteochondrosis develop. The sooner you start treatment, the shorter the course of therapy will be.
Treatment of vegetative-vascular dystonia
Vegetative-vascular dystonia is treated with medications, psychotherapy and lifestyle correction. Patients are prescribed symptomatic treatment: sedatives, anti-anxiety drugs, sleeping pills, restoratives, and vitamins. The goal of psychotherapy for VSD is to teach the patient to regulate negative emotions and increase stress resistance. The lifestyle is also adjusted: you need to balance work and rest, exercise and adhere to a balanced diet.
How to treat osteochondrosis at home?
It is not recommended to treat osteochondrosis at home. There are several reasons for this:
- at home it is impossible to accurately diagnose “osteochondrosis”, since back pain has different origins: neurogenic, vascular, viscerogenic (due to diseases of the internal organs) and psychogenic. That is, a person is treating osteochondrosis, but in fact, back pain arose, for example, due to kidney diseases;
- it is impossible to objectively assess the effectiveness of treatment without control diagnostics;
- the patient cannot adequately select treatment for himself, and folk remedies do not have an evidence base, and therefore, most likely, they are ineffective and may have side effects.
In one case, you can be treated at home - only after consulting a doctor who will correctly diagnose, prescribe adequate treatment and periodically monitor the effectiveness of therapy using X-rays, CT or MRI.
How to determine that the pathology is caused by osteochondrosis
The following symptoms are typical for panic attacks and depression:
• spontaneity. Anxiety may appear for no apparent reason;
• changes in character: increased aggressiveness or “tearfulness” in a balanced patient, apathy in an active patient, reluctance in sexual intimacy in a loving one;
• feeling of lack of air. Thus, the brain sends a signal about a lack of oxygen to the respiratory organs.
• sleep and appetite disturbances. Anxiety symptoms affect the nervous system. The desire to eat normally disappears, night rest becomes restless, and dreams become chaotic, often nightmarish.
If such symptoms are caused by osteochondrosis, then usually a person can also feel the following “bonuses”: dizziness, sudden changes in pressure (dystonia), headache, periodic numbness of the limbs and facial muscles, hearing and vision impairment.
If at least 2 of the above symptoms coincide, you will not be able to cope with depression and panic attacks on your own. A doctor's help is needed.
Treatment of spinal osteochondrosis
Treatment of osteochondrosis can be conservative or surgical. Which method will be the main one depends on the stage of the disease and the neglect of the musculoskeletal system.
Conservative treatment includes medications, physical therapy and lifestyle adjustments. Medications are mainly prescribed anti-inflammatory drugs and muscle relaxants to relieve pain and normalize muscle tone. In physical therapy, one of the main conditions for recovery is early activation, that is, 1-3 days after pain is eliminated, you need to walk, run, exercise in the pool or ride a bike. It is also important to change your lifestyle to an active one, since sedentary behavior is one of the factors in the development of back pain and destruction of the nuclei of the intervertebral discs.
Surgical treatment is used in cases where conservative therapy has proven ineffective within 2–4 weeks, and in cases where there are pronounced structural changes in the spine. What kind of operation is needed will be determined by the surgeon after consultation with a neurologist and studying research data. For example, in the treatment of osteochondrosis of the cervical spine, methods are used that relieve the spinal cord from pressure from the vertebrae or hernia (discectomy and decompression).
If you experience back pain, which is accompanied by lumbago in the spine or neck, aching pain in the chest, weakened muscles in the arm or leg, unpleasant tactile sensations on the skin and numbness, consult a neurologist for advice.
0
0
0
Article rating:
5 out of 5 based on 1 rating
Author: Makeeva Marina Anatolyevna
Neuropathologist, reflexologist. Highest category. Candidate of Medical Sciences. Work experience 26 years.