An orthopedic or neurosurgeon may recommend cervical spine surgery to relieve neck pain, numbness, tingling and weakness, restore nerve function, and stop or prevent neck instability.
Cervical spine surgery may involve removing a disc or bone tissue and fusing the vertebrae with a bone graft either in front or behind the spinal column. A bone graft can be one of two types: an autograft (from the patient's own bone) or an allograft (donor bone). Sometimes metal plates and screws are also used to further stabilize the spine. These devices are called tools. When the vertebrae are stabilized through surgery, excess mobility disappears and the function of the nerve roots is restored.
An alternative to spinal fusion (fusion) is to replace the intervertebral disc in the cervical spine with an artificial disc, which restores movement in the neck and stabilizes the spine.
Degenerative diseases
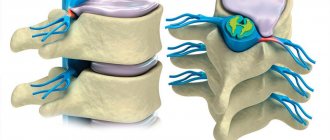
In degenerative disc disease, the distance between the vertebrae shortens, causing the discs to wear down, which can lead to the formation of a herniated disc.
Degenerative processes can also develop in the joints of the spine (facet joints) or bone tissues with the development of spondyloarthrosis (spondylosis). Degenerative processes in the spine can lead to compression of nerve structures (spinal stenosis or root compression) with the development of symptoms such as pain, numbness, muscle weakness or dysfunction of the pelvic organs.
Nucleoplasty
Nucleoplasty is one of the latest medical achievements in the field of intervertebral hernia surgery. It not only rightfully belongs to the group of minimally invasive operations, but is a representative of the direction of percutaneous surgery, since all manipulations to remove a hernia are carried out through a puncture with a diameter of about 3-4 mm.
Nucleoplasty is considered the most gentle method of surgical treatment of spinal hernia, since it:
- allows you to avoid blood loss;
- makes it possible to activate the patient within 2-3 hours after completion;
- does not require hospitalization (discharge occurs on the same day);
- characterized by an easy and quick recovery period with an almost complete absence of restrictions;
- does not involve risks of nerve damage or complications characteristic of general anesthesia;
- ensures the preservation of the natural biomechanics of the spine;
- leads to complete recovery in 80% of cases;
- does not lead to the formation of postoperative scars.
The essence of the method is to introduce a special guide needle and then an electrode into the center of the nucleus pulposus of the intervertebral disc and partially destroy it under the constant control of an image intensifier. Depending on what is used to destroy part of the nucleus pulposus, the following types of nucleoplasty are distinguished:
- laser;
- cold plasma;
- radiofrequency;
- hydroplastics.
During the operation, the surgeon makes several back-and-forth movements with the electrode without removing it from the disc. As a result, so-called passages are formed in the nucleus pulposus, diverging from one point in different directions. Such actions do not lead to a change in the qualitative composition of the core, but due to the evaporation of a certain volume of it, negative pressure is created inside the disc, which contributes to the retraction of the hernial protrusion and ultimately the restoration of the normal size and shape of the disc.
The surgeon constantly monitors the amount of destroyed internal disc contents using an image intensifier monitor, which eliminates the possibility of removing too much material.
But the hernia cannot retract instantly; this requires some time. Therefore, the first results can be assessed immediately after the completion of minimally invasive surgery, but the final effect occurs after 2-4 weeks.
The operation is performed under local anesthesia. If the patient is very worried, he may be given an injection of a sedative. This will help improve your psycho-emotional state and reduce the level of anxiety before the upcoming minimally invasive intervention. The total duration of the procedure is about 15-30 minutes. After it is completed and the instruments are removed from the body, not a single stitch is placed on the remaining puncture wound. It is enough to cover it with a sterile bandage to prevent infection.
During one operation, the neurosurgeon can remove only one hernia. If a patient is diagnosed with multiple disc bulges, they will require the same number of interventions.
But nucleoplasty by any of the methods can be performed only for uncomplicated hernias less than 6 mm . For larger formations it will be ineffective. The only drawback of the method is the possibility of developing a recurrent hernia in the same disc. But this in most cases is caused not by the shortcomings of the operation as such, but by the lack of changes in the patient’s lifestyle. If he continues to lead a sedentary lifestyle and gain excess weight, there is a high probability that the disease will not only recur, but will also affect other intervertebral discs.
This minimally invasive operation cannot be performed if:
- sequestered hernias;
- spinal canal stenosis with osteophytes;
- acute infectious disease;
- paralysis or paresis;
- severe disruption of the pelvic organs against the background of the development of radicular syndrome.
Laser hernia removal
Laser nucleoplasty began to be used earlier than cold plasma, but today it is inferior to it in popularity. The method involves using thermal energy created by a quartz LED as an agent that destroys the molecules of the nucleus pulposus. The pulses emitted by it lead to heating of tissues to 60-67 ° C, which leads to the “evaporation” of the molecules of the internal contents of the disk. The resulting steam is discharged outside through a special hole in the working probe.
The procedure leads to a reduction in the size of the disc and retraction of the hernia by reducing the pressure in it to 30%. Thanks to this, the pressure of the pathological protrusion on the nerve roots is eliminated and the pain syndrome is progressively reduced.
Cold plasma nucleoplasty
It is the destruction of part of the nucleus pulposus of the disc with cold plasma that is considered the safest method of removing an intervertebral hernia, since in addition to all the general advantages of nucleoplasty, this method is also distinguished by the absence of the risk of overheating of surrounding tissues, which can be observed when using a laser or radio waves. Therefore, cold plasma nucleoplastics enjoys well-deserved popularity, and only hydroplastics can compete with it.
Cold plasma nucleoplasty was first tested in 1995 and has since earned the recognition of neurosurgeons around the world. It is based on the use of cold plasma generated by a special apparatus to destroy part of the nucleus pulposus. Its temperature does not exceed 45-50 °C, which eliminates the possibility of burns to the fibrous ring, vessels or other anatomical structures.
Cold plasma is formed between the ends of the device’s electrodes, which are immersed in a cannula pre-installed in the center of the disk. As a result, energy is released, which instantly breaks down the macromolecules of cartilage tissue into low molecular weight substances. As a result, there is a decrease in disk volume.
Unlike other methods of nucleoplasty, cold plasma can be reused to destroy part of the nucleus pulposus in the event of a recurrent hernia.
Radiofrequency nucleoplasty
Radiofrequency nucleoplasty involves the destruction of the required volume of the nucleus pulposus by a high-frequency electric field. The action of UHF currents leads to heating of molecules to 60°C and the formation of the same “passages” inside the nucleus pulposus, the closure of which with the remaining cartilage tissue leads to a reduction in the size of the hernia and an improvement in the patient’s condition.
Hydroplastics
Hydroplasty is based on a completely different method of destroying part of the nucleus pulposus. It does not involve the slightest thermal effect, which completely eliminates the risk of developing undesirable consequences. The method is based on the use of powerful pressure of a sterile saline solution in which an antibiotic is pre-dissolved.
The minimally invasive operation also involves inserting a conductive needle into the nucleus pulposus disc under the control of an image intensifier, through which a special hydroresector connected to the console of the SpineJet device is then immersed. It has two channels: a narrow one is intended for supplying liquid, and a wide one is for suctioning it back.
Under the influence of a flow of solution, the speed of which can reach 900 km/h, the required volume of the nucleus pulposus is destroyed into tiny fragments. They, along with the waste fluid, are immediately aspirated and removed from the intervertebral disc. As a result, the pressure inside it decreases, and the hernia is pulled back.
Even in comparison with other nucleoplasty techniques, hydroplasty has even greater advantages, since it allows you to insert a hydroresector not only into the center of the disc, but also directly to the fibrous ring at the site of protrusion formation. This significantly increases the effectiveness of the procedure. It eliminates the possibility of accidental injury to the peripheral parts of the disc and, if necessary, can be repeated.
Cervical spine deformity
For patients with cervical spine deformities such as hyperlordosis, spinal straightening and stabilization surgery can significantly reduce symptoms and improve quality of life. Congenital deformities or so-called anomalies of the craniocervical or craniovertebral junctions can affect the cervical spine and be a reason for surgical treatment.
Injuries.
Since the cervical spine is very flexible, it is susceptible to injury. Some injuries can cause fracture and/or dislocation of the cervical vertebrae. In severe neck injuries, the spinal cord may also be damaged. Patients with a fracture, especially those with spinal cord injury, undergo surgery to relieve pressure on the spinal cord and stabilize the spine.
Instability of the motor segments of the cervical spine due to various pathological processes can lead to abnormal mobility of the vertebrae and effects on the nerve structures.
Treatment
When prescribing treatment, the doctor is based on the degree of displacement of the vertebrae. If there is a slight displacement, the doctor suggests observation - taking control radiographs of the spine 1-2 times a year to monitor the displacement of the vertebrae. The first degree is treated conservatively. In some cases, spinal traction in the hospital and wearing a corset are prescribed. With traction, the movement of blood and lymph accelerates, which prevents tissue destruction, and medications are better absorbed. If the vertebrae are displaced at the initial stage, it is recommended to fix the spine in a rigid corset.
Avoid any physical stress on the spine. If pain bothers you, take painkillers, muscle relaxants, and NSAIDs. Anti-inflammatory therapy is prescribed. The second, third, fourth and fifth degrees with active complaints require surgical treatment - transpedicular spinal fusion. Surgery for vertebral displacement consists of stabilizing the vertebrae using a special titanium structure.
During the operation, the vertebral arch and the resulting scars are removed, as a result of which the nerve roots are relieved of pressure. The displaced vertebrae are attached to the metal structure with screws.
Revision surgery
Revision surgery is often required to correct the deformity. The type of revision depends on the specific pathology. The operation can be done with either anterior or posterior access.
The complication rate from revision surgery of the cervical spine is higher than with other surgical techniques. After revision surgery, it is also more difficult to relieve pain and restore nerve function. Patients should also be aware that the chance of long-term neck pain increases with revision surgery.
Contraindications for surgery
Even if there are strong indications for surgery, it cannot be performed if:
- acute local or general infectious and inflammatory processes;
- autoimmune diseases at the stage of decompensation, including diabetes mellitus and thyroiditis;
- severe blood clotting disorders;
- recent stroke or heart attack;
- uncompensated chronic diseases of the kidneys, lungs, liver and heart;
- severe thrombosis of the deep veins of the lower extremities.
In such situations, surgery is possible only after correcting the patient’s condition with a specific course of treatment.
Cervical spine surgery: objectives and techniques
If degenerative changes in the cervical spine lead to the development of myelopathy (spinal cord dysfunction), radiculopathy (nerve root dysfunction), neck pain or abnormal mobility, then surgery may be required. The goal of surgery is to relieve pain and restore stability to the spine.
Surgeons use 2 main surgical methods to solve problems in the cervical spine:
- Decompression: removal of tissue that puts pressure on the nerve structure
- Stabilization: restricting movement between vertebrae.
These 2 techniques may be used in combination, or the patient may simply undergo decompression surgery or simply undergo stabilization surgery.
Indications for surgical treatment of osteochondrosis
Surgical intervention for osteochondrosis is indicated in 10–15% of cases. The help of a neurosurgeon, as a vital measure, is required when there is a pronounced threat of causing critical damage to the structures of the central nervous system, especially the spinal cord, nerve plexuses and large blood vessels.
In such cases, the likelihood of disability increases several times, so surgical intervention is recommended to be carried out as soon as possible. The main reason is the onset of paresis and paralysis, more often of the upper or lower extremities, less often of the entire half of the body or the area below the affected SMS.
Osteochondrosis of the cervical spine increases the risk of stroke.
The severity of these complications is underestimated by patients. They are often irreversible. Therefore, in some situations, the need for surgery is not even discussed, especially when conservative therapy is completely ineffective.
Surgery is recommended if at least one of the following is present:
- Symptoms of acute compression of the roots of the cauda equina of the lumbar spine: impaired sensitivity of the feet;
- weakness of the thigh muscles;
- numbness in the perineum;
- loss of Achilles and/or knee reflexes;
- severe pain in the lumbosacral region;
- bright pain radiating to the limbs;
- dysfunction of the pelvic organs, manifested by involuntary leakage of urine or feces, decreased or complete loss of potency.
- severe constant or paroxysmal throbbing headache, covering the back of the head, temples and forehead;
- frequent attacks of dizziness, which can lead to loss of consciousness;
- nausea or vomiting that occurs due to a headache or when changing body position;
- high blood pressure, presence of signs of angina pectoris;
- noise or ringing in the ears;
- visual disturbances, manifested by decreased visual acuity, pain in the eyeballs, and the appearance of a “veil before the eyes”;
- speech disorders;
- vestibular disorders.
The occurrence of such signs is regarded as a good reason for immediately contacting a neurosurgeon and conducting a comprehensive examination, including MRI, neurological tests and other diagnostic procedures. Based on the research results and the patient’s medical history, the spinal surgeon decides on the need for surgery for osteochondrosis or the possibility of conservative treatment.
Understanding Decompression Surgery
Surgical decompression techniques can be performed using an anterior or posterior approach to the spine, depending on how and where the nerve tissue compression has occurred.
In decompression, the tissue pressing on the nerve root or spinal cord is surgically removed or more space is created so that the nerve tissue is not impacted in any way. The main types of surgical decompression procedures are:
- Foraminotomy:
If the intervertebral disc material or osteophyte puts pressure on the root at the exit from the foraminal opening, then a foraminotomy may be performed. Foraminotomy is used to enlarge the intervertebral foramen and thus relieve compression. - Laminotomy:
Similar to a foraminotomy, but involves creating a hole in the plate to create more space for the spinal cord. - Laminectomy
: An ectomy is the medical term for removal. A laminectomy removes part or all of the plate to relieve pressure on the spinal cord. - Facetectomy:
involves removing the facet joint to relieve pressure on the nerve root exiting the spine. - Laminoplasty:
Laminoplasty means shaping an anatomical structure to restore form or function. In the case of the cervical spine, laminoplasty is the surgical shaping of a plate to create more space for the spinal cord. - Each of the above decompression techniques is performed from the back (back) of the spine.
- However, sometimes the surgeon needs to perform decompression from the front of the spine. For example, if an intervertebral disc bulges into the spinal canal, it sometimes cannot be removed from behind because the spinal cord interferes with access. In such cases, decompression is usually performed from an anterior approach to the neck.
Anterior decompression techniques:
- Discectomy:
surgical removal of part or all of a herniated disc. - Corpectomy:
Sometimes disc material becomes interposed between the vertebral body and the spinal cord and cannot be removed by discectomy alone. In other cases, bone spurs (osteophytes) form between the vertebral body and the spinal cord. In these situations, access to the disc may require removal of the entire vertebral body. This procedure is called corpectomy (corpus means and ectomy means removal). - Transcorporeal microdecompression
(TCMD): TCMD is a minimally invasive procedure that is performed in the cervical spine from an anterior approach. The procedure is performed through a small channel made in the vertebral body to access and decompress the spinal cord and nerve. TCMD can be performed as a stand-alone procedure or in combination with anterior discectomy and fusion (ACDF) and/or total disc replacement. - Spinal stabilization
- Discectomy and corpectomy usually result in instability in the cervical spine. Instability means abnormal movement of the vertebrae, increasing the likelihood of serious neurological damage. In these situations, it is often necessary to surgically restore spinal stability.
Basic surgical methods of stabilization:
- Fusion (fusion)
is the fusion of bones, usually with the help of a bone graft or biological substance. Spinal fusion stops excess motion between two vertebrae and provides long-term stabilization. The procedure is somewhat similar to the consolidation of bone tissue after a fracture. - With fusion in the cervical spine, both adjacent vertebral bodies and facet joints or laminae can be connected.
- If the fusion is performed posteriorly, the surgeon will usually place strips of bone graft from one lamina or lateral (lateral) mass onto the lamina or lateral mass below. Typically, the bone graft grows into the tissue of the fixed structures over time and stabilizes the two vertebrae. The surgeon can use a similar technique to simultaneously fix the facet joints.
- Instrumentation:
Posterior cervical fusions can be supplemented with specially designed fixation devices such as staples, screws, rods and plates. These devices increase stability and facilitate fusion.
Disc replacement
The parapharyngeal microsurgical approach allows you to safely approach the disc herniation without making muscle incisions. Pirogov's triangle is a place that allows you to safely remove a protruding disc without causing harm to surrounding tissues. The tissues are very gently separated with special instruments, and the vessels of the muscles and ligaments are moved back. The prevertebral tissue is displaced to the side and the intervertebral disc is exposed, which is removed.
There are special models of prostheses that the vertebrologist selects during the operation, setting different sizes of the model between the bodies, after removing the disc. When the layout is selected according to its dimensions, an artificial disk is installed. In this way, the anatomy of the spine is restored and the body does not feel that a disc has been removed. The dimensions of the prosthesis are the same and there is no load on adjacent segments of the spine.
A separate instrument is used to insert the prosthesis. A Caspar distractor is installed, which pushes the vertebral bodies apart and at this moment the prosthesis is easily installed in the interbody space. Other advantages of the method are:
- Restoring the integrity of the intervertebral disc;
- low risk of developing postoperative complications;
- short rehabilitation period;
- no significant postoperative pain.
The operation is used when a hernia forms on the side or in the middle of the disc. It is not contraindicated in case of inflammation in the spinal canal, but cannot be performed in case of stenosis. In the latter case, the solution to the problem is possible only through posterior access or a combination of posterior and anterior access.
Decompressions and fusion
Sometimes the surgeon will perform decompression and fusion. For example, after a discectomy, space appears between the vertebral bodies. This gap is usually filled with a bone graft (from the patient's pelvic bone or from donor bone) or a spacer, which supports the spine and promotes fusion. This type of surgery is called an anterior cervical discectomy and fusion, or ACDF.
Many surgeons use fixation devices (plates with screws) in the anterior surgical approach to perform ACDF or corpectomy. These devices help improve fusion stability.
Postoperative recovery
Surgery on the cervical spine is complex and requires careful implementation of a number of measures:
- After surgery, complete regeneration will take several months. To limit neck movement and provide support, a neck brace is often recommended after surgery. Limiting neck movement promotes effective fusion of the vertebrae. It is important that the patient rests.
- Patients are advised to resume slow walking as soon as possible after surgery. It is necessary to gradually increase the duration of walking, and if the patient has difficulty walking in the first few days after surgery, then it is better to avoid walking. Before starting walking, you should consult with your doctor. It is advisable to walk 10-15 minutes a day.
- Avoid lifting heavy loads, bending, performing overhead work with arms, and sudden or forceful turns of the neck. Do not carry out any activities that put stress on the neck muscles. Driving is also not allowed after surgery. The patient needs to join exercise therapy classes 3-4 months after surgery. But physical exercise is possible only after the bones have fused properly.
- The length of time it takes for the bones to completely fuse (fuse) varies from patient to patient. It also largely depends on what method was used to surgically fuse the bones. If the surgeon used the patient's own bone or instrumentation for surgical fusion, then the bones will fuse quite quickly, in about 3-4 months. But, if a bone graft from a donor is used, then it takes a longer time for the bones to fuse (within 6-9 months). Recovery time will be further prolonged if the patient is overly physically active, performs work with the arms above the head, and holds the neck arbitrarily in any direction. Every day the patient experiences less discomfort. The time required for the patient to return to normal activities will also vary. Some may take 3-6 months, while some may take a year to fully heal.
- If the patient notices any signs of infection, swelling, redness or thickening at the site of surgery or incision, then he must see his doctor. To treat severe pain after surgery, your doctor may prescribe narcotic pain medications. Gradually, as the pain decreases, the doctor moves on to conventional analgesics. Certain pain medications and nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, naproxen, ibuprofen, and COX-2 inhibitors, should be avoided for several months after surgery.
- Follow-up scheduled appointments with the attending surgeon are absolutely necessary to evaluate the recovery process and verify the reliability of the surgical implants or artificial disc. If there is persistent pain, the doctor may prescribe certain diagnostic tests, such as MSCT or MRI, EMG (ENMG). It is also important that the patient takes the medications prescribed by the doctor in a timely manner.
- Smoking is a big enemy on the road to recovery. Smoking should not be resumed after surgery because nicotine disrupts or interferes with the bone healing process, which is necessary for successful fusion. Smoking also increases the risk of complications after surgery.
- Diet is another important aspect of recovery. The patient must eat a healthy and nutritious diet to allow muscle and bone tissue to recover. It is necessary to include animal proteins in the diet, as they contain all the essential amino acids, while vegetarian sources do not contain some amino acids. A balanced diet helps in healing and recovery.
- Family members and loved ones should provide support to the patient so that he/she can get rid of emotional stress. The patient experiences a lot of stress during the surgery and hence good care and support from the family members after the surgery will be of great help in mitigating the stress.
Risks of Anterior Cervical Discectomy and Fusion (ACDF)
- The most common complication and risk of this surgery is dysphagia, which can easily be attributed to difficulty swallowing. The esophagus, which lies just in front of the spine, must be repositioned and mobilized during the surgical process to prevent a dysphagic condition. With proper treatment, dysphagia may disappear within a few days or weeks. But the main threat may be that dysphagia, once it develops, may remain permanent.
- Fusion of the bone graft may fail, with the development of pseudarthrosis
- Failure to relieve symptoms or address the cause of surgery
- Damage to the spinal cord or nerve root. However, this complication is very rare.
- Sometimes there may be bleeding. It can occur if a blood vessel in the neck is damaged.
- During surgery, damage to the trachea or esophagus is possible
- Possible damage to the vocal cords due to damage to the larynx
- Leakage of cerebrospinal fluid (CSF leak)
- The chances of infection are minimal, but cannot be completely ignored
- Hematoma
- Seroma (serum leakage from damaged lymphatic and blood vessels)
Risks of decompression surgery with a posterior approach
- Damage to the nerve root and spinal cord
- Recurrence of disc herniation
- Dural leak (a condition in which the thin covering of the spinal cord, called the dura mater, is damaged by the surgeon's instrument)
- Infection may occur during surgery as the deep internal parts of the body are exposed to air for a long time
- Some blood loss is inevitable as this is a complex surgical procedure and the surgeon must cut through various tissues
- Continued pain in the neck or surgical site
Surgery on the cervical spine is recommended by a doctor only if medications and other non-surgical procedures, such as physical therapy, exercise therapy, etc., do not relieve symptoms or restore stability of the motion segments.
As a rule, modern surgical techniques allow the patient to recover within several months. However, one must understand that any surgical intervention, especially in the cervical spine, is very stressful and does not bring the state of health to the point where surgery can no longer be avoided.
What should you pay attention to after surgery?
After surgery, the spine should be at rest. Avoid sudden movements. Within 2-3 days, a Shants collar splint is placed on the neck - a soft and elastic anatomically shaped retainer that limits head rotation to 30°. Depending on the medical indications, you will be prescribed manual therapy to eliminate functional disorders of the musculoskeletal system, which will be carried out by an experienced physiotherapist. There is no need to remove sutures, as special absorbable threads are used during the operation. Therefore, you are allowed to take a shower already on the 7th day after the intervention.
- Inpatient treatment: 4 days
- Recommended time of stay in the clinic: 10-14 days
- Possible return home: after 7 days
- Recommended return flight: after 14 days
- When is it permissible to shower: after 7 days
- When sutures are removed: not necessary (absorbable sutures)
- When can you drive again: in 2 weeks
- Outpatient physical therapy: 2 weeks