Osteoarthritis of the hip joint is a degenerative disease of the musculoskeletal system. It is characterized by limited mobility, severe pain, and difficulty moving. The disease is accompanied by the destruction of cartilage tissue, as a result of which mobility deteriorates, friction occurs between joints, and osteophytes form. This disease is most often diagnosed in people over 45 years of age. It is very important to carry out treatment on time. Arthrosis in its advanced form becomes a cause of disability. You can undergo complex treatment for arthrosis of the hip joint at ArthroMedCenter.
Why you shouldn’t delay treatment for joint pain
Coxitis occurs due to infectious diseases, due to hereditary predisposition, injuries and increased stress on the joint, diseases of the endocrine and immune systems. Inflammation can spread throughout the body, so do not delay seeing a doctor and treating your hip joints. In addition to arthritis, there is arthrosis (coxarthrosis) - inflammation localized in the tissues of the joint. Both diseases significantly impair the quality of life. Competent and timely treatment of the hip joints will help eliminate this problem.
Cell and tissue engineering
These areas of medicine study the problems of cartilage tissue regeneration. Articular cartilage is being restored using cell- and tissue-engineered structures (CEC and TEC). These two approaches have the same goal - to replace destroyed cartilage fragments with normal, complete tissue.
- KIC . The essence of the method is the intra-articular injection of a mixture containing a biostimulating matrix, multipotent mesenchymal stromal cells (MMSC) and bioactive molecules (growth factors, cytokines). The introduced substances stimulate the regeneration of cartilage tissue, thereby restoring the functions of the joint. Note that the biopolymer matrix is responsible for delivering the components of the mixture to the cartilage, and the cells contained in the CIC have a regenerating effect.
- TEAK. Tissue-engineered structures are “grown” from CICs in special bioretractors that provide the necessary conditions for the proliferation and differentiation of cellular elements. Artificially synthesized cartilage tissue is implanted into the joint cavity, where it partially or completely replaces damaged cartilage.
Note that different types of biological material can be used for intra-articular injection or implantation. In particular, to stimulate the restoration of cartilage tissue, cell mixtures obtained from the human body or synthesized artificially are used. And for implantation, cartilage tissue that is own or “grown” in a bioretractor can be used.
Don't confuse engineering with transplantation. These are two completely different concepts. Remember that autotransplantation of your own tissues or fluids is not a method of cell or tissue engineering. These methods are discussed only in the case of the use of artificially synthesized or cultivated biomaterials.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Minimally invasive endoprosthetics in the Czech Republic: doctors, rehabilitation, terms and prices.
Find out more
Treatment of joint arthritis
The most effective treatment for hip arthritis is comprehensive. At our medical center it includes:
- drug therapy - stops the inflammatory process, eliminates the causative agent of infection, relieves pain and other unpleasant manifestations of the disease;
- physical therapy – restores mobility, increases tissue elasticity;
- physiotherapy - helps the body recover faster;
- manual therapy and massage - improve blood supply to tissues and relieve pain.
How to treat arthrosis of the hip joint?
Conservative therapy is used to treat arthrosis of the hip joint. If the desired result after treatment is not available, surgery is prescribed.
Tactics of drug treatment
To treat coxarthrosis, doctors prescribe medications. Their task is:
- reduction or complete relief of pain;
- regeneration or inhibition of destruction of cartilage fibers;
- restoration of blood microcirculation;
- getting rid of existing pathological processes.
Painkillers are prescribed in the form of tablets, intramuscular or intra-articular injections, and external preparations. At the initial stages of treatment, non-steroidal anti-inflammatory drugs will be effective. If the pain is intense, injections of hormonal drugs are used. If muscle spasms are present, muscle relaxants are prescribed.
Auxiliary drugs are chondroprotectors. They help restore cartilage structures. They have a cumulative effect, so they will need to be taken over an extended period of time.
Additionally, medications that improve blood microcirculation may be prescribed. The use of medications will be effective only in the initial stages of the disease.
Doctors can also prescribe the following procedures to a patient:
- UHF;
- magnetic therapy;
- electrophoresis;
- ultrasound;
- ozokerite;
- massage;
- acupuncture;
- therapeutic exercises;
- balneotherapy;
- mud therapy;
- cryotherapy;
- kinesiotherapy;
- mineral and radon baths.
Surgical intervention
In the final stages of the disease, medications and physiotherapy can only slightly alleviate the symptoms. But it is almost impossible to restore full motor function at these stages with the help of medications. In the last stages, surgical treatment is indicated:
- corrective osteotomy, which preserves the joint;
- arthrodesis, in which the hip joint is closed;
- endoprosthetics, in which the hip joint is replaced using an implant.
Symptoms of the disease
The presence of coxarthrosis of the hip joint can be suspected if characteristic signs and pronounced localization are present. The intensity of discomfort depends on the stage of the disease.
At first, the pathology is asymptomatic or has mild symptoms such as barely noticeable pain and slight restrictions in movement. Symptoms appear after significant physical activity, prolonged walking or prolonged standing. Localization of pain is noted in the hip joint, sometimes moving from the thigh to the knee. Unpleasant sensations disappear after rest. Occasionally there is stiffness in the joint in the morning, but in general the range of motion is completely preserved. There is no muscle atrophy or changes in gait.
Lack of treatment for a disease such as coxarthrosis of the hip joint threatens to move into the second stage. Symptoms at this stage become more pronounced: the intensity of pain increases, discomfort is disturbing even in complete rest. After physical activity, lameness may occur. In addition to the joint, pain is felt in the groin and thigh. The range of motion decreases, the person experiences discomfort during abduction and internal rotation of the hip. As a result of displacement of the head of the bone and a forced decrease in motor activity, atrophy of the muscles responsible for adduction/abduction of the hip, as well as extension/flexion, is observed. On the part of the affected joint, a decrease in the volume of the femoral and gluteal muscles becomes noticeable.
The third degree of coxarthrosis is characterized by constant severe pain that does not go away day or night. It becomes more and more difficult to move; a person is forced to use a cane or walker for support while walking. There is a sharp limitation in the range of motion, drying out of the muscles of the lower leg, thigh and buttock. Due to the weakness of the femoral abductor muscles, there is a shortening of the leg and a skew of the body towards the affected limb. A shift in the center of gravity leads to an increase in the load on the affected joint.
When extending or flexing the hip joint, while walking, you can hear crackling, crunching, or clicking sounds in it. This happens due to friction between bone growths and surfaces. Normally, this also happens, but in the case of coxarthrosis, such sounds are combined with painful sensations.
Creation of artificial cartilage
Not so long ago, scientists were confident that articular cartilage would be one of the first artificial tissues. However, in the process of its creation, the developers encountered a number of difficulties. As it turned out, copying the structure and biomechanical properties of cartilage tissue is extremely difficult, almost impossible.
To “grow” full-fledged cartilage that would be suitable for implantation, not only the presence of a matrix and growth factors is required, but also mechanical stimulation.
Nowadays, work is still ongoing on the creation of artificial cartilage that would exactly replicate the structure of natural ones. So far, this direction of engineering is considered the most promising. It is quite possible that the creation of high-quality TECs will soon become a real breakthrough in the treatment of deforming arthrosis.
Methods of cell and tissue engineering are still at the stages of development and implementation in clinical practice. They look quite promising, but so far they cannot completely replace endoprosthetics. However, there is a high probability that in just a few decades it will be possible to get rid of arthrosis with a few injections.
Biomedical cell products for cartilage tissue regeneration
Nowadays, biomedical cell products containing autologous (that is, belonging to the person himself) chondrocytes are gradually being introduced into clinical practice. Some drugs are a pure substrate of these cells, others also contain a biodegradable carrier (matrix, scaffold).
Fact! Scientists believe that it is best to use cartilage cells from the nasal septum for cultivation. They have a fairly high potential for differentiation, and they are not difficult to obtain.
Table 1. Means for restoring cartilage tissue.
| Product | Manufacturer | Description |
| Carticel | Genzyme corp., USA | The medicine is a culture of a person’s own cartilage cells. A small amount of cartilage tissue is removed from the patient through a biopsy, which is then cultured for 3 weeks. The resulting substrate usually contains about 12 million cells. A suspension of chondrocytes is injected into the joint cavity after preliminary arthroplasty. |
| DeNovo-NT | Zimmer, Biomet, USA | To manufacture the product, juvenile allogeneic cartilage, autologous chondrocytes and fibrin glue are used. Injected into the joint cavity, DeNovo-NT “sticks” to areas of cartilage degeneration and stimulates their restoration. |
| Chondro-Gide | Genzyme Biosurgery, Denmark | It is an autologous matrix that initiates the process of biological restoration of cartilage. The material is used to cover the subchondral bone after it has been cleared by arthroscopy. Note that Chondro-Gide is suitable for eliminating cartilage defects with an area of less than 2 cm2. |
| BioSeed-C | Bio Tissue Technologies GmbH, Germany, Switzerland, Italy | The product consists of autologous chondrocytes and a biosoluble gel containing polyoxidane and polyglycolic acid. According to the manufacturer, BioSeed-C is suitable for the restoration of degenerative and post-traumatic cartilage defects. |
| Chondron | SewonCellontech, Korea | It is a mixture of autologous chondrocytes and a fibrin gel-based matrix. |
In addition to those listed in the table, there are many other cell engineering products (Chondrogen, MACI, ChondroCelect, etc.) that could theoretically be used to repair damaged cartilage. Unfortunately, they are all still in different phases of clinical trials. This means that they will begin to be used in practical medicine in at least a few years.
Causes of the disease
It is not always possible to establish the causes and identify the prerequisites for the development of premature deformation of hyaline cartilage. In this case, we are talking about primary (ideopathic) coxarthrosis, which appears and progresses on its own, without visible reasons. Destructive-degenerative joint damage, formed under the influence of various external and internal factors, is called secondary coxarthrosis.
Pathology develops due to various reasons:
• Diseases of the spine and joints. These include hip dysplasia, congenital hip dislocation, flat feet, Perthes disease, curvature of the spinal column, injury due to a fall or severe bruise.
• Genetic predisposition. Coxarthrosis is not inherited, but through kinship, a child can inherit the structural features of the musculoskeletal system and cartilage tissue, as well as the specifics of metabolism.
• Violation of metabolic processes.
• Changes in hormonal levels.
• Inflammatory processes in the joint capsule (reactive and rheumatoid arthritis, salt deposition, synovitis, bursitis, tendonitis).
• Loss of bone tissue (osteoporosis).
• Diabetes.
• Irreversible age-related changes in the osteochondral structure of the joint.
• Exhaustive physical work.
• Significant overload of the joint due to professional activities or training in heavy sports.
Too little physical activity, excess weight, bad habits, prolonged stress - all this negatively affects the condition of the bone and cartilage tissue in the hip joint.
Stages of progression of coxarthrosis
There are three stages in the development of the pathology, the common symptom of which is pain in the hip joint with gradually increasing intensity. Other signs of the disease appear as the condition worsens, so over time it becomes much easier to determine the advanced state of coxarthrosis. Stages of disease development:
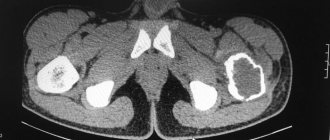
• First degree. It is characterized by an uneven narrowing of the gap between the articular surfaces and the formation of single osteophytes at the acetabulum. In this case, the neck and head of the femur are in normal condition.
• Second degree. There is a narrowing of the joint space by approximately 2 times the norm, upward displacement of the deformed and enlarged femoral head, and proliferation of osteophytes on the edges of the acetabulum outside the cartilaginous disc.
• Third degree. There is partial or complete fusion of the joint space, an enlarged femoral head, and a large number of bone growths
Sequence, timing and main features of the stages
| Postoperative stages | Intervals by period | Postoperative nature | Physical activity mode |
| Early phase | from 1 to 7 days inclusive | acute reactive inflammatory reaction | early gentle |
| from 8 to 14 days | epithelialization, contraction, wound healing | light-tonic | |
| Late stage | from 15 days for 6 weeks | beginning of remodeling: predominance of bone resorption | primary restorative |
| from 7th to 10th week. | dominance of hard tissue renewal processes | late recovery | |
| from 11 weeks until 3-4 months have passed from the date of surgery | completion of bone repair adapted to new conditions | adaptive |
Orthopedic surgeons strongly advise that you spend 3 weeks after surgery undergoing a treatment and recovery phase in the orthopedic department of a surgical hospital, then for about the same amount of time in a specialized rehabilitation center. After this, to consolidate the results obtained, take a course of health improvement in a resort-sanatorium-type institution, specializing in the profile of therapeutic and preventive treatment of the musculoskeletal system.