Medial apophysitis is sometimes considered a variant of medial epicondylitis, but in fact it is caused by excessive traction and inflammation of the apophysis of the medial epicondyle and is therefore a separate term.
The elbow is the most common site of injury in the immature skeleton of baseball players aged 9–12 years. Inflammation of the apophysis of the medial epicondyle usually occurs as a result of repeated throwing or throwing of a ball with force.
Most patients consult a doctor with vague complaints of pain in the medial aspect of the elbow. They may also complain of decreased throwing speed and control.
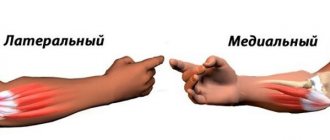
The elbow joint consists of the bones of the upper arm (humerus) and one of the bones of the forearm (ulna). The bony projections at the end of the humerus are called epicondyles. The projection that is closer to the body is called the medial epicondyle, and the projection on the outside of the elbow is called the lateral epicondyle.
The muscles that allow wrist flexion attach to the medial epicondyle, and the muscles responsible for wrist extension attach to the lateral epicondyle. Excessive flexion causes irritation of the muscles that attach to the medial epicondyle.
In a child, bones grow from areas called growth plates. The growth zone of the medial epicondyle is called the medial apophysis. With medial apophysitis, irritation or inflammation occurs in this area.
Pathogenesis
The part of the humerus that participates in the formation of the elbow joint contains small tubercles called the outer (lateral) and inner (medial) epicondyles. The tendons of the forearm muscles are attached to them. With a significant increase in the functional load on the hand flexor muscles, which are attached to the medial epicondyle, microdamage to the fibers of their tendons, as well as the bone base of the attachment area, is formed with the development of an inflammatory reaction.
Treatment of medial epicondylitis of the elbow joint
The doctor will listen to the patient’s complaints and carefully examine. You will need to answer questions about the nature of the pain, how the pain affects your normal activities, and whether you have had any injuries to your elbow.
Special tests for stretching the corresponding muscles are also used, which helps in clarifying the diagnosis.
The doctor may ask you to take an x-ray of the elbow joint to rule out bone pathology or the consequences of an injury that you may have forgotten. An x-ray can also show whether there is calcification (calcium deposits) where the tendons attach to the epicondyle, indicating a long-term inflammatory reaction in this area due to chronic injury.
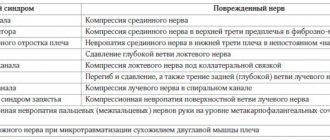
The symptoms of medial epicondylitis are very similar to a condition called cubital tunnel syndrome. This is a disease caused by compression of the ulnar nerve. In the cubital canal: between the olecranon process, medial epicondyle and ligament.
Causes
The main provoking factor leading to the formation of microdamages in the area of the internal epicondyle of the humerus is playing sports associated with a fairly high load on the muscles of the forearm. This condition is known as golfer's elbow because it often develops in professional golfers. Also, medial epicondylitis is provoked by several factors not related to sports:
- Professional human activity, in particular related to the use of hand tools.
- Age - in people over 45 years of age, degenerative-dystrophic processes develop in the medial epicondyle, leading to tissue damage and an inflammatory reaction.
- A congenital change in the properties of bone and connective tissue, caused by a change in the functional activity of certain genes responsible for their strength. In this case, the inflammatory process in the medial epicondyle can develop since childhood.
- Chronic inflammation of the structures of the elbow joint, caused by the influence of other provoking factors, in particular an infectious process, an autoimmune reaction (a pathological condition accompanied by the formation of autoantibodies that damage the body’s own tissues).
- Previous injuries to the elbow area, leading to the formation of scars with subsequent inflammation.
Reliable identification of the cause is primarily necessary for the selection of adequate therapy and subsequent prevention of medial epicondylitis.
Medial epicondylitis
Experts' opinions:
Kuzmenko Dmitry Vladimirovich
Shoulder epicondylitis
all expert opinions
Video on the topic:
all videos on the topic
What is the disease
Medial epicondylitis is a degenerative-dystrophic process that affects the area of the muscle that attaches to the epicondyle of the humerus.
Medial epicondylitis is less common than lateral epicondylitis and, unlike the latter, inflammation spreads to the inner surface of the elbow joint in the area of the connection of the hand, articular ligaments and muscle flexors of the fingers.
Types and causes of occurrence
At risk are men whose work involves increased physical activity, as well as athletes who regularly load their limbs and the main load extends to the forearm and elbow. As a result of constant repetitive movements and stress on the joint, blood circulation is disrupted, and microtraumas and microtears occur in the tendon tissue. Because of this, an inflammatory process develops, tissues degenerate, tendon tissue is replaced by scar fibers.
The cause of medial epicondylitis lies in the overload of the wrist flexors and pronator muscles during regular exercise. Less commonly, the disease can be caused by osteochondrosis of the cervical and thoracic spine, connective tissue dysplasia, weakening of ligaments, osteoporosis, impaired blood supply, and glenohumeral periarthritis.
Symptoms
Medial epicondylitis is characterized by a slow development of symptoms. Signs make themselves felt when the inflammatory process has progressed:
- there is a dull aching pain in the elbow joint,
- the tone of the arm muscles decreases,
- when pressing on the inner surface of the ligaments and muscles, the patient experiences pain,
- hand movements are limited,
- the pain intensifies when clenching the hand into a fist.
The pain intensifies immediately after minor muscle strain. After some time, basic movements, such as shaking hands, become impossible, as the pathological process spreads to the ulnar nerve.
The acute period of the disease lasts two months, the symptoms are sharply painful. Medial epicondylitis is considered chronic if the painful syndrome lasts more than two months, while the signs of the disease become dull.
Which doctor should I contact for medial epicondylitis?
To eliminate signs of inflammation, you need to consult an orthopedist. The doctor will establish an accurate diagnosis and develop treatment tactics in accordance with the individual characteristics of the patient.
Treatment methods
First of all, if pain in the elbow increases, you need to give up physical activity, secure the limb with a bandage and apply a cold compress. It is recommended to take a non-steroidal anti-inflammatory drug to relieve inflammation and reduce pain.
When treating medial epicondylitis, the following scheme is used:
- use of local anti-inflammatory ointments and creams,
- corticosteroid blockade for intense, unremitting pain, as well as Milgamma injections,
- wearing an orthosis or a fixing bandage while performing any movements with the arm. The design relieves muscle tension, immobilizes the limb,
- Exercise therapy to relax and strengthen muscles and normalize joint functionality,
- physiotherapy for accelerated tissue regeneration. Sessions of microcurrent therapy, laser therapy, magnetic therapy, cryotherapy, acupuncture, dry heat treatment,
- massage. It is not the elbow itself that is massaged, but the forearm and the side of the neck.
Surgical treatment is indicated if conservative therapy is ineffective within six months. During the operation, the surgeon removes pathologically changed elements, sutures the tendons, and forms channels in the medial epicondyle for improved blood circulation. After the procedure, a week of immobilization is carried out, after which rehabilitation begins.
results
Within 2-3 weeks, the inflammation is stopped and the disease is eliminated. Based on practice, athletes return to their duties after a few months.
Rehabilitation and lifestyle restoration
For about three months you need to limit the load on the joint and not lift anything over two kilograms. You should massage your forearm every day and warm up during any physical exercise.
If the ulnar nerve is inflamed due to medial epicondylitis, then electrical stimulation is started. Physiotherapy sessions alternate with physical therapy to develop the joint. Under the supervision of an instructor, the patient first stretches the pronators and flexors of the arm, then moves on to isometric exercises and weight training.
Return to list
Classification
Based on the localization of the pathological inflammatory process, medial and lateral epicondylitis is distinguished. According to the main causative factor, the disease can be of pathological and traumatic origin; usually the more common form of pathology is provoked by microtrauma of the forearm muscles and their tendons.
Also, for ease of diagnosis and choice of treatment, epicondylitis is classified into types according to the severity of the inflammatory process. All criteria for the classification of the disease are displayed in the final diagnosis after an objective diagnostic study.
Manifestations
In most cases, the clinical symptoms of medial epicondylitis develop gradually over a fairly long period of time. The most characteristic symptoms of this disease are the following:
- Pain localized on the inside of the lower part of the humerus. Initially, it appears after physical activity, and then can be at rest. Pain sensations vary in severity, depending on the intensity of the inflammatory reaction.
- Weakness of the forearm muscles, which perform the function of flexing the hand and fingers. This manifestation is a reaction of the muscle fibers of the striated skeletal muscles to the inflammatory response.
- Inflammatory manifestations of the tissues of the elbow joint area - they develop in the case of a pronounced pathological reaction, are characterized by redness (hyperemia) of the skin, as well as its swelling with an increase in tissue volume.
These manifestations bring discomfort to a person’s life, reduce his ability to work, and also eliminate the possibility of a future career for professional athletes.
diagnostics
diagnosis
Clinical manifestations of medial epicondylitis may have certain similarities with other pathologies of the musculoskeletal system affecting the structures of the upper limb, therefore, an objective examination is required to make a final diagnosis. It includes instrumental diagnostic techniques with visualization of the internal structures of the elbow joint:
- ultrasound;
- X-ray;
- CT;
- MRI;
- arthroscopy.
Laboratory research techniques are used to determine the cause and severity of inflammation. After the research, the orthopedic traumatologist has the opportunity to select the most adequate treatment for this disease.
Conservative treatment
Treatment with drugs can be carried out as monotherapy or represent a preparatory stage before physiotherapeutic procedures, as well as surgery. For this purpose, non-steroidal anti-inflammatory medications are used in the form of capsules, tablets, ointments or creams.
In case of severe inflammation, glucocorticoid hormones are prescribed, which have a more pronounced anti-inflammatory effect. The duration of therapy is determined by a decrease in the intensity of the inflammatory reaction, as well as the disappearance of clinical symptoms of the disease and restoration of the functional state of the elbow.
Treatment
In the acute phase, splinting, arm elevation, rest, cold on the elbow, and nonsteroidal anti-inflammatory drugs such as ibuprofen may be prescribed. Weight-bearing movements of the elbow (such as heavy lifting) should be avoided for 4 to 6 weeks. After this period of unloading the elbow, it is necessary to involve rehabilitation (physical therapy). A full load can be given only after the symptoms have completely disappeared and the inflamed growth zone has regenerated. If a child returns to sports too quickly, changes in the growth plate may become irreversible. Recovery from medial apophysitis occurs in different ways and depends on the timeliness of the treatment started. In some cases, especially growth plate avulsions, surgical treatment may be required.