How to treat?
Orthopedic doctor, candidate of medical sciences Litvinenko Andrey Sergeevich:
The treatment program for epicondylitis is drawn up depending on the form, stage, and the presence of concomitant pathologies. The set of measures includes: protective regime, drug therapy, physiotherapeutic procedures, blockades, and the use of special fixatives. An integrated approach allows you to restore joint function, avoid surgery and return to a full life.
Which doctor should I contact?
- Epicondylitis is treated and diagnosed by:
- An orthopedic traumatologist is the main specialist: makes a diagnosis, prescribes an examination, gives recommendations, performs injections and surgical operations.
- A sports medicine doctor will help you choose the right training regimen and give advice on the nature of permissible loads.
- Physiotherapist - helps select and conducts the necessary physiotherapeutic procedures.
- Specialist in physical therapy - necessary during the recovery period to strengthen muscles and develop movements in the joint.
At first glance, the clinical picture of epicondylitis seems harmless, since it does not cause excruciating pain or clear signs of inflammation. As the disease progresses, it becomes chronic, and it becomes difficult for the patient to lift and hold even light objects in his hands. Over time, atrophy of the forearm muscles and limited mobility in the elbow joint develop.
First aid
Epicondylitis is characterized by a gradual development of symptoms, however, if severe pain appears after exercise or injury to the elbow, a number of measures should be taken:
- If pain occurs, it is recommended to stop the load and create rest for the elbow and shoulder joints, immobilize the arm; for this purpose, you can use, for example, a scarf bandage.
- In the first 24 hours, apply cold for 15-20 minutes every hour to reduce swelling and pain.
- If the pain is unbearable, you can take a painkiller or use topical ointments.
- If symptoms persist, you should consult a doctor.
Conservative treatment
Conservative therapy is effective in 80-90% of cases, and if all doctor’s recommendations are followed, it usually gives good results, aimed at eliminating pain, restoring blood circulation in tissues, movements and muscle strength. In case of epicondylitis, first of all, it is necessary to eliminate the provoking factors, rebuild the training regimen, eliminate physical activity, and change the work and rest schedule.
Video description text
Drug therapy
Includes drugs that are used in the form of ointments and gels, compresses, tablets and injections:
- Anti-inflammatory ointments - they relieve local inflammation well, relieve symptoms, help relieve muscle tension after exercise, are effective at the initial stage, use: Voltaren-gel, Diclak, Fastum-gel, Traumeel, for a course of up to 2 weeks.
- Compresses with dimexide are used to reduce inflammation, pain, and tissue swelling. The compress is applied for 1-1.5 hours, novocaine and voltaren-emulgel are added along with dimexide.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) - have an analgesic effect, reduce inflammation, tissue swelling, and act on the symptoms of the disease. NSAIDs are considered the first step in the treatment of epicondylitis; movalis, nimesil, nise, arcoxia are prescribed. The course of admission is from 7 to 14 days.
- Chondroprotectors and collagen-containing preparations strengthen tendons and muscles, help restore articular cartilage, and increase tissue elasticity.
- Vitamin complexes - contain the necessary macro- and microelements, improve metabolism, speed up the healing process.
Injection techniques
- Corticosteroids, hormonal drugs (diprospan, kenalog, dexamethasone, hydrocortisone, betamethasone) have a pronounced anti-inflammatory, anti-edematous and analgesic effect, providing a “tip of a needle” effect. They are used in a solution with novocaine or lidocaine (the composition of the blockades can be single- or multi-component). They require use strictly according to the instructions and prescription of a doctor, as they have side effects and a number of contraindications, they are used in the form of medicinal blockades, the injection is made directly into the area of the inflamed epicondyle and tendon. Prescribed for severe pain and ineffectiveness of other methods, treatment is symptomatic.
- A number of authors recommend adding a lidase solution to the classic blockade to soften scar tissue. Others additionally add homeopathic preparations Traumeel-S, goal-T, it is believed that this reduces the severity of the side effects of hormones.
- Injections of hyaluronic acid, according to some authors, improve tendon gliding and tissue swelling. However, they have not been used in widespread practice due to low efficiency, questionable results and the high cost of the drugs.
Drug blockade for inflamed epicondyle
Orthobiology methods
- Injections of the patient’s own blood plasma (PRP therapy) are widely used in the treatment of epicondylitis, the effect is based on the introduction of autoplasma enriched with platelets with a high content of biologically active substances (cell growth factors) into the inflammatory focus, which creates a powerful anti-inflammatory effect in tissues, stimulates regeneration and blood supply, angiogenesis (sprouting of new microcapillaries).
- Plasmolifting is a domestic method of using platelet-rich plasma (PRP), which is not inferior in effectiveness to PRP therapy. It should be noted that after plasma injections, the pain may intensify somewhat, this is a normal reaction and goes away after 3-5 days. During this period, cold is applied to the injection site and stress is eliminated.
- SVF+PRP therapy is a technology of using stromal fraction cells obtained from one’s own adipose tissue and plasma, used when conservative methods are ineffective, with the aim of regenerating damaged tendons and stopping the inflammatory process. A number of authors consider the method as a last resort before surgical treatment.
Tests and diagnostics
The diagnosis is made on the basis of a survey, examination of the patient and a number of studies. The disease is not characterized by changes in laboratory tests.
Initially, the doctor collects anamnesis, asking the patient a series of questions.
Next, an examination is carried out, during which the specialist examines the affected area, determining whether there is swelling, redness, discomfort, or pain. A number of functional tests are also carried out - for example, the patient is asked to shake hands, raise a glass of water, etc.
In addition, the doctor may prescribe additional research methods: manual muscle testing, radiography, MRI, ultrasound, etc.
Physiotherapy
Physiotherapeutic procedures are indicated for all forms of the disease; the orthopedist and physiotherapist select each patient individually. For a speedy recovery, it is recommended to combine several techniques. In this case, the course of the disease, the presence of contraindications, and the characteristics of the body are taken into account. physiotherapy is always carried out in courses of 3 to 15 sessions, with varying intervals between procedures.
Shock wave therapy session
- Phonophoresis with hydrocortisone. The medicine is delivered to the inflammatory focus using ultrasound. By stimulating blood flow and metabolism in tissues, hydrocortisone helps relieve swelling and has an anti-inflammatory effect. The result is visible after 3-5 procedures. The course of treatment includes 5,7 or 10 sessions.
- Electrophoresis. Electric current is applied to the inflamed area, and novocaine is additionally used to reduce pain. Under the influence of electrophoresis, blood microcirculation improves, inflammation and swelling of the tendons decreases, and drugs penetrate deeper into the tissue. 7-10 procedures are prescribed, with an interval of 1-2 days.
- Magnetotherapy. The magnetic field stimulates blood circulation and metabolic processes, reduces swelling. After just a few sessions, movements in the elbow joint become less painful and discomfort decreases. Up to 10-15 sessions are recommended.
- Interstitial electrical stimulation (ITES). The technique is based on the ability of electric current to have an analgesic effect. One of the electrodes, in the form of a needle, is placed in the area of the inflamed epicondyle and tendons, the rest are placed cutaneously, in the area of the muscles of the forearm. Duration up to 20-30 minutes, course treatment 5-7 sessions, with an interval of 3-5 or 7 days.
- Laser therapy, laser beams are able to penetrate deep into tissue and have a thermal effect. This helps increase blood circulation and relieve the inflammatory reaction.
- Myostimulation. The effect of pulsed current on muscle fibers. Improves blood supply and tone of muscles and tendons, helps avoid atrophy.
- Darsonval. The elbow is exposed to low-intensity electric currents and high voltage. Capillary blood circulation accelerates, lymph outflow improves, tissues are restored faster. The technique has not found widespread use.
- UHF. Method of exposure to high-frequency electromagnetic fields. The thermal effect promotes blood flow and activation of metabolic processes.
- Shock wave therapy for epicondylitis acts on the causes of the disease, is based on the effects of acoustic waves, has an effect on pathological tissues - softens areas of fibrosis and salt deposits in the tendons, increases local blood flow, accelerates recovery processes, stimulates the synthesis of collagen and elastin. It has been proven to be up to 96% effective, helps to cure the disease, and combines well with other methods. The course requires 5-7 sessions.
- Cryotherapy, treatment using cold, helps reduce local swelling and pain in the acute period, due to short-term spasm and subsequent expansion of microcapillaries, improves blood supply.
The technique of interstitial electrical stimulation according to Gerasimov for epicondylitis helps relieve pain in several sessions
Orthopedist, candidate of medical sciences Timur Vyacheslavovich Kholikov recommends:
Good results are obtained by combining shock wave therapy with the use of platelet-rich plasma from the patient's blood (PRP therapy). The technique allows not only to relieve pain and inflammation, but also to strengthen tissue damaged by epicondylitis by stimulating regeneration in tendons and muscles.
External immobilization
In order to immobilize and create rest, various methods of fixing the joint are used. So, in case of severe pain, in the acute stage, the elbow is fixed with a plaster or plastic splint in a functionally advantageous position (flexion at an angle of 80-90 degrees), for a period of 5-10 days, the arm itself is placed on a scarf. A longer period is not recommended, as this can lead to the development of contracture; as a rule, this period is sufficient for the pain to subside. During the immobilization period, it is recommended to perform exercises for adjacent joints to improve blood circulation. If necessary, the splint is converted into a removable one or replaced with an elastic bandage.
Taping
Special elastic adhesive tapes are used - tapes, which are placed cutaneously along the muscle groups of the forearm and imitate the ligamentous apparatus of the joint. Kinesio taping provides functional rest to the elbow, reduces stress on muscles and tendons, relieves pain, improves blood circulation and lymph flow in the tissues. The technique has found wide application in sports, since in case of some types of epicondylitis, it allows you to continue training.
Bandages and fixators
Special orthopedic products are used for both treatment and prevention of epicondylitis. In the acute period and with severe pain, orthoses with a locking hinge are used to create rest. The joint receives additional fixation, which reduces the load and the risk of injury. Bandages are recommended when performing similar movements and physical activity. A bandage with a pneumatic cushion is widely used, which exerts gentle pressure on the tendons, thereby helping to relieve the area of the inflamed epicondyle and change the degree of muscle tension during loads.
Soft elbow bandage
Classification
According to the characteristics of the course of the disease, the following forms are distinguished:
- Acute - in this case, first there are complaints of muscle tension and slight soreness, after which constant severe pain appears.
- Subacute – pain is felt during exercise, and disappears at rest.
- Chronic – pain manifests itself for three or more months, with remission followed by relapse.
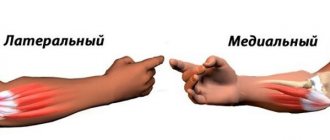
According to the location of the disease, the following are distinguished:
- Lateral epicondylitis (external) - an inflammatory process develops in the tendons that attach to the epicondyle on the outside of the bone. External epicondylitis is diagnosed more often than internal epicondylitis. Often treatment for such a disease is required for those who play tennis.
- Medial epicondylitis of the elbow joint - inflammation develops in the area of attachment to the internal epicondyle. The medial type of the disease can occur as a result of playing golf, shot throwing, javelin, etc. However, this type of disease develops not only in athletes, but also in tailors, typists, surgeons, etc. Due to the connection of this type of disease with certain activities, it develops more often in women .
Therapeutic exercise (physical therapy)
It is recommended to perform special physical exercises only after the inflammatory process has stopped. The complex of therapeutic exercises helps restore muscle tone, tendon elasticity, and improves blood supply to tissues. Even in severe cases, exercise therapy should not be excluded. It is necessary to devote at least 20-30 minutes a day, and for people whose work involves monotonous workload, such exercises should be performed regularly, even in the absence of pain.
Postisometric muscle relaxation (PIR) is carried out by a physical therapy specialist, or a chiropractor, and consists of smooth stretching of the tendons and muscle groups of the forearm, alternating periods of resistance and rest, as well as performing special resistive exercises.
Before performing exercises, you should consult your doctor. Exercising during an exacerbation or premature training leads to muscle overstrain and worsening of the condition.
| Hand exercises | Hand exercises |
Pathogenesis
During the development of the disease, periosteal inflammation occurs, subsequently leading to the appearance of microtraumas in the area of muscle attachment. Local inflammation of the nerves innervating the epicondyles may also develop. Factors that provoke the development of these processes are microtrauma or muscle failure. In addition, local disorders in the tendons, collagen degeneration of cartilage tissue, degeneration of fibrils and fibrocytes can be provoking phenomena.
The pathophysiology of the disease is associated with professional activities and activities that require constant forceful supination and pronation of the forearm. During the development of the process, the development of subperiosteal hemorrhages, calcification , and degenerative changes in tendon tissue may be noted.
Security mode
Relevant for all types of disease, both during exacerbation and in remission. It consists of dosing loads and eliminating provoking factors:
- Change in the nature of activity or working conditions. Systematic muscle overstrain during work provokes the development of the disease; transfer to light work is recommended. For example, when working at a computer, it is desirable that the elbow joint is on the table, and the mouse pad is equipped with a special anatomical cushion that relieves the hand.
- The use of mechanized tools and process automation, alternating periods of work and rest.
- Dosing of sports loads and restructuring of the training program. Monotonous movements that require sudden movements of the hands are excluded. For example, in tennis, if symptoms of “tennis elbow” appear, it is recommended to reconsider the hitting technique, or select the optimal weight of the racket.
The protective regime should not be neglected. These simple measures will help stop the progression of epicondylitis.
Surgery
Up to 20% of epicondylitis are subject to surgical treatment. The indication is the absence of positive dynamics within 6 months of conservative treatment. Several types of operations are performed:
- Tenolysis is carried out to excise the scar tissue of the tendons and restore their free movement.
- Osteoperforation of the bone in the area of the epicondyle promotes the migration of bone marrow cells to the site of inflammation and reduces the symptoms of the disease.
- Tenoplasty - lengthening of the extensor tendons is necessary in cases of severe adhesions and the impossibility of restoring the functionality of the forearm muscles.
- Arthroscopy is a minimally invasive endoscopic operation, performed through a microincision, the task is to “clean” the tendon tissue from areas of fibrosis and adhesions.
In the postoperative period, the patient is prescribed drug therapy and rest. On days 7-14, physiotherapeutic methods and light physical therapy exercises are added. After 3-4 months, the patient returns to a full life.
Carrying out a surgical operation does not guarantee a 100% result; there are examples of unsuccessful operations and relapses.
Symptoms of epicondylitis of the elbow joint
Symptoms of the disease depend on the location of the inflammatory process.
Lateral epicondylitis (“tennis elbow”) is manifested by the following symptoms:
- Pain on the outside of the elbow that radiates to the outside of the forearm.
- Increased pain in the elbow with movement, especially with external rotation of the forearm and its extension. The pain also becomes stronger during palpation of the external epicondyle of the humerus. At rest, the unpleasant sensations subside.
- The patient cannot hold objects in his hands.
- Due to atrophy of the forearm extensor muscles, the fingers may go numb, and at the same time pain in the shoulder develops.
Medial epicondylitis is manifested by the following symptoms:
- Pain on the inside of the elbow, which radiates to the flexor muscles of the forearm.
- The pain becomes worse during movement when the forearm bends inward.
Very often, symptoms can be pronounced and significantly affect the patient’s performance. However, sometimes they are weak. In this case, the disease may go away on its own over time. As a result, the person does not seek help, and the process can become chronic.
Disease prevention
It is an integral part of treatment and is indicated even after complete recovery:
- Compliance with working conditions, periodic rest after loads of the forearm and hand;
- Dosing or complete elimination of monotonous loads;
- Warm up before playing sports;
- Preparation of a training regime program with the participation of a general physical training (GPP) trainer;
- Providing additional protection for the elbow joint using elbow pads, tapes, bandages and fixators.
We should not forget about developing a working posture and correct and safe hand position while working.
An increase in physical activity is allowed only after the complete cessation of pain after 6-8 weeks. Regular strengthening of the forearm muscles and taking vitamin and mineral complexes are also preventive measures.
Literature sources
- Arshin V.V. Orthopedic diseases of the hands from functional overstrain: abstract. dis. Dr. med. Sciences / Arshin V.V. -Samara, 1996.-39 p.
- Builova T.V. Rehabilitation for epicondylitis of the shoulder. Clinical recommendations / T.V. Builova, M.B. Tsykunov // Bulletin of Restorative Medicine / - 2021. - No. 1 (71). - With. 80-84
- Bukup, K. Clinical study of bones, joints and muscles / K. Bukup. - M., Medical literature, 2008. - 320 p.
- Vorotnikov, A.A. Extracorporeal shock wave therapy in the treatment of tendopathies of the upper and lower extremities in patients with aggravated somatic status / A.A. Vorotnikov, A.N. Cymbal.
- Zulkarneev, R.R. Shock wave therapy for injuries and diseases of the musculoskeletal system / 6. R.R. Zulkarneev, K.E. Valeev, Yu. R. Stepanov // Kazan Medical Journal/ - 2009. - No. 5 (90). — P.753-754. 6. Karateev, Yu.A. Ermakova // Modern rheumatology. - 2015.-No. 3(9). — P. 33-42.
Diet
Diet for sore joints
- Efficacy: therapeutic effect after 2-3 months
- Terms: 2-6 months
- Cost of products: 1700-1800 rubles. in Week
It is important to have enough foods containing vitamin D and calcium in your diet. It is recommended to eat more cottage cheese, dairy products, and fatty fish.
You should minimize your consumption of foods containing sugar and also reduce the amount of salt you consume.