Why are joints deformed?
Traumatic injuries
Short-term deformity due to soft tissue swelling occurs with all joint injuries. More significant reasons for changing the configuration are:
- Dislocations.
The articular ends of the bone are displaced relative to each other, as a result the joint takes on an unnatural appearance, the limb is lengthened or shortened. There is sharp pain and springy resistance when trying to move. - Fractures.
The deformity is provoked by the displacement of bone fragments and is aggravated by the accumulation of blood in the joint. Intense pain and severe impairment of support and movement are observed. Pathological mobility and crepitus are possible, but not required. - Ligament ruptures.
With complete or almost complete damage, the ligament ceases to fix the joint, the distal segment deviates to the side, and the joint is bent. External changes are more noticeable with knee and ankle injuries.
Inflammatory and degenerative diseases
Deformations are formed against the background of acute and chronic inflammatory diseases of the joints. In acute processes, changes increase over several weeks or months. In patients with chronic pathologies, years may pass from the onset of the disease to noticeable joint deformities. The reasons for the development of the symptom are:
- Aseptic arthritis
: rheumatoid, juvenile, gouty, psoriatic, with SLE, Reiter's syndrome, Behçet's disease, ankylosing spondylitis, polychondritis dissecans. - Infectious arthritis:
provoked by nonspecific microflora (including when inflammation passes from the bone against the background of osteomyelitis), with tuberculosis, gonorrhea, and some other diseases. - Secondary arthritis
: with sarcoidosis, malignant tumors, osteomyelitis, diseases of the blood, digestive system, respiratory organs.
Infectious arthritis affects one joint; with gonorrhea, polyarthritis is possible. In other cases, mono-, oligo-, or polyarthritis may be observed, but multiple symmetrical or asymmetrical involvement of joints is more common.
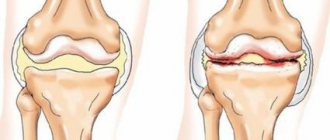
Another common cause of deformity is osteoarthritis. Post-traumatic arthrosis occurs at any age, affecting one joint. For arthritis of non-traumatic etiology, late manifestation (middle and old age) is typical. Often there is damage to several joints with an uneven course of degenerative processes. The patient may be bothered by one joint or paired joints against the background of minor symptoms or the asymptomatic course of other arthrosis.
Joint deformation
Congenital anomalies
The most noticeable visual deformation is detected in pathologies of the knee joint - congenital dislocation of the tibia or patella. Dislocation of the lower leg is often bilateral, accompanied by a violation of the joint configuration, limitation of movements, and muscle atrophy. The nature and severity of the deformity varies significantly depending on the characteristics of the displacement of the shin bones.
When the patella dislocates, the appearance of the front of the knee changes. The patella is often displaced outward. Due to the concomitant underdevelopment of the lateral condyle of the tibia, instability of the limb, and repeated injuries, patients develop early severe deforming arthrosis and form contractures, which aggravates the deformity.
Hip dysplasia and congenital hip dislocation are the most common congenital anomalies, but external deformation in these pathologies is not so noticeable, since the hip joint is deep, hidden by a significant amount of soft tissue. First of all, attention is drawn to the asymmetry of the joints and changes in the length of the limb. Over time, deformities progress due to arthrosis and contractures.
Bowed legs
O-shaped legs can be a congenital anomaly (for example, in patients with fibrocystic dysplasia), formed against the background of rickets, Blount's disease, or osteitis deformans. With this disorder, the knee joints bend at an angle that is open inward. The pathology proceeds relatively favorably, but when it occurs early and there is significant curvature, it is complicated by arthrosis, which increases the deformity.
X-shaped legs are often acquired in nature, formed due to rickets, premature onset of standing and walking, excessive load on the joints at an early age due to obesity or weak ligaments, after injuries and tumors. Sometimes there is a hereditary predisposition. The knee forms an angle that is open outward. Patients develop gonarthrosis early, which entails a further change in the appearance of the limbs.
Consequences of injuries and illnesses
In the long-term period, in patients with intra-articular fractures, the configuration of the damaged joint changes due to improper fusion of fragments or the formation of excess callus. Concomitant ligament injuries with subsequent development of instability play a certain role. Fibrous processes in the periarticular soft tissues are important.
Contractures and ankylosis are almost always accompanied by external deformation. Along with injuries to solid structures (dislocations, fractures), their formation is caused by arthritis, arthrosis, and congenital pathologies. In addition, the cause of joint deformation with the development of contracture can be:
- deep scars after severe burns, abscesses, phlegmon, extensive wounds of the periarticular area (especially infected);
- prolonged immobilization with subsequent shortening of muscles, development of fibrosis of the soft tissue structures of the joint;
- severe ischemia of the limb due to compression of the arteries by bone fragments during injury (Volkmann ischemic contracture);
- paresis and paralysis of neurogenic origin after spinal cord injury, spinal cord and brain tumors, stroke, head injury, encephalitis, cerebral palsy, with injuries to peripheral nerves, severe neuropathies.
Hereditary diseases
Due to its low prevalence, hereditary pathologies are considered a fairly rare cause of joint deformity. Joint pathology can be part of complex changes in the skeleton, combined with metabolic disorders, disturbances in the functioning of internal organs, and facial deformities. The symptom occurs in the following diseases:
- mucopolysaccharidoses;
- pseudoachondroplasia;
- Ollier's disease;
- Cornelia de Lange syndrome;
- Thiemann's disease;
- Klippel-Trenaunay syndrome;
- Shereshevsky-Turner syndrome;
- Lery-Weil dyschondrostosis.
Intervertebral osteochondrosis
Intervertebral osteochondrosis also goes by names such as discosis or discitis. The pathology is caused by an increase in the intensity of degenerative processes in the intervertebral discs, as a result of which their shock absorption and elastic properties deteriorate, and the mobility of the spine decreases.
The progression of the pathological process is determined by a combination of endo- and exogenous factors, which include metabolic and endocrine disorders, as well as macro- and microtrauma. The development of intervertebral osteochondrosis is manifested by changes in the gelatinous nucleus: its turgor decreases, the disc loses its ability to fully absorb shock.
Due to the pressure of the vertebral bodies, the height of the disc decreases, and the fibrous ring protrudes beyond the intervertebral space. As a result, it can put pressure on the spinal cord structures.
Pathogenesis of osteochondrosis
Sometimes the annulus fibrosus becomes covered with cracks, through which fragments of the gelatinous nucleus extend beyond the disc. In this way, a Schmorl's hernia, or cartilaginous hernia, is formed.
The symptoms of the pathological process are determined by the location of the hernia. If it is localized in the front, then no clinical manifestations are observed, but in the case when the hernia is located posteriorly, it penetrates the spinal canal and provokes symptoms of cervical radiculitis.
The clinic here is determined not by the pressure of the hernia, but by the inflammatory reaction in the nerve roots and epidural tissue, and the symptoms also make themselves felt due to venous stasis.
The symptoms of secondary radiculitis are explained either by protrusion of the fibrous ring beyond the intervertebral space, or by a true hernia with a posterior location. Clarification of this circumstance is important for choosing the method of surgical treatment in a particular case.
Intervertebral osteochondrosis is most often localized in the lower back, somewhat less frequently in the cervical spine, and even less so in the thoracic spine. It is possible to identify pathology only with a thorough orthopedic-neurological examination of the patient.
The leading symptom of the pathological process is local pain syndrome. With lumbar localization of the lesion, pain is observed in the lower back, radiating to the buttocks and lower limb.
During the examination, the following is determined:
- smoothness of lumbar lordosis;
- symptom of “reins”, that is, a sharp tension in the paravertebral muscles of the lower back;
- antalgic scoliosis;
- pain on palpation of the spinous processes adjacent to the disc involved in the pathological process;
- Osna-Shkolnikov symptom, that is, sharp pain in the spine upon palpation of the abdominal wall in the projection of the 4th lumbar vertebra.
The identification of neurological symptoms is determined by the location and characteristics of the lesion of the intervertebral disc. When the nerve roots are compressed, the patient complains of pain in the area of their innervation, paresthesia, weakness in the limbs, decreased severity or complete loss of tendon reflexes. If the symptoms are expressed bilaterally, then this confirms massive disc prolapse.
To make a diagnosis of intervertebral osteochondrosis, a study of cerebrospinal fluid is used, as well as a number of instrumental techniques, which include discography and venospondylography.
Diagnostics
The cause of non-traumatic deformities is determined by rheumatologists. Diagnosis of traumatic injuries and their consequences is the responsibility of orthopedic traumatologists. According to indications, consultations with a geneticist, oncologist, and other specialists are prescribed. The initial stage of the examination includes a conversation with the patient, a general physical examination, a detailed examination of the joints with an assessment of their configuration, size, and range of motion. Based on the data obtained, a diagnostic action plan is drawn up, within the framework of which the following can be carried out:
- Radiography.
A standard study is performed in two projections. If necessary, targeted photographs and radiographs of symmetrical joints are prescribed. The technique allows you to visualize fractures, dislocations, areas of destruction and osteolysis, changes in the joint space, and bone growths. - Ultrasound of the joint.
Indicated for assessing the condition of intra- and periarticular soft tissues. Confirms the presence of hemorrhages, inflammatory processes, areas of calcification. - MRI and CT of the joint.
Recommended when the results of basic methods are ambiguous. They make it possible to accurately determine the nature of the pathology, the volume and location of the pathological focus. They can be carried out at the stage of preparation for surgery in order to plan the tactics of surgical treatment. - Joint puncture.
It is carried out in the presence of liquid. For injuries, it is performed for therapeutic purposes. In case of joint diseases, after evacuation, the fluid is sent for cytological, immunological or microbiological analysis to clarify the etiology of the pathological process. - Arthroscopy.
Produced for autoimmune diseases, tuberculosis, and some other conditions. It can be diagnostic or therapeutic-diagnostic. Provides detailed visualization of joint structures, sometimes including biopsy. - Lab tests
. They confirm the presence of an inflammatory process, identify markers of autoimmune pathologies, and are used to determine the pathogen and its antibiotic sensitivity in infectious diseases.
X-ray of the hands
Classification of degenerative-dystrophic pathologies
Degenerative joint diseases can be divided into several main groups, namely:
- Primary and secondary deforming osteoarthrosis.
- Intervertebral osteochondrosis.
- Deforming spondyloarthrosis.
- Osteochondropathies (including: Osgood-Schlatter, Perthes, Kienbeck, Koenig, Keller disease).
The listed pathologies provoke degenerative changes in the joints; the clinical features of various diseases will be discussed below.
Treatment
Pre-hospital assistance
In case of injury, the arm or leg is fixed using a splint or improvised devices (for example, planks), and the limbs are ensured in an elevated position. Cold is applied to the injured area, and an analgesic is given for severe pain. For pain, swelling, and redness of non-traumatic origin, rest is recommended; short-term use of painkillers and anti-inflammatory drugs is acceptable. An increase in symptoms, an increase in general temperature, and a deterioration in general condition are reasons for urgent consultation with a specialist.
Conservative therapy
For patients with traumatic injuries, a blockade of a fracture or dislocation is performed, reduction is performed, and immobilization is performed with a plaster cast. Sometimes skeletal traction is indicated. Conservative therapy for joint deformities may include the following measures:
- Protective mode
. Includes load limitation, sometimes the use of orthopedic devices, canes, crutches, walkers. - NSAIDs
. They are an essential part of the treatment of many diseases and injuries. Reduce pain, reduce the severity of the inflammatory process. Can be used in the form of tablets, injections, creams, ointments, gels. - Antibiotics
. Necessary for infectious pathology. For nonspecific infections, they are prescribed in short courses (from one to several weeks). For STIs, they are administered according to special regimens. For tuberculosis, long-term treatment lasting several months is indicated. - Hormonal drugs
. In the form of blockades, they are used when pain and anti-inflammatory treatment is ineffective during exacerbations. Some autoimmune pathologies require the use of general medications. - Chondroprotectors
. Improves the condition of cartilage tissue. Intra-articular administration, tablets or injections are possible. - Physiotherapeutic procedures
. Taking into account the characteristics of the pathology, drug therapy is supplemented with medicinal electrophoresis, UHF, ozokerite and paraffin applications, magnetotherapy, laser therapy, shock wave therapy, massage, manual therapy, acupuncture. - Physiotherapy
. During the treatment period, exercise therapy ensures the preservation of limb function and reduces the risk of complications. At the rehabilitation stage, it allows you to improve the functions of the affected segment and restore your ability to work.
Osteochondropathies
Osteochondropathy is a degenerative-necrotic pathology that develops due to impaired trophism and progression of dystrophic processes in the subchondral parts of the epiphyses of bones.
More often, cases of pathology occur in childhood and adolescence. The disease is characterized by a chronic benign course and a favorable outcome.
The exact reasons for the development of osteochondropathy are unknown, but doctors are inclined to believe that the pathology develops under the influence of one or more factors from the list:
- injury;
- infectious process;
- genetic predisposition;
- disturbance of metabolic processes and trophism.
The pathogenesis of osteochondropathy involves a local disturbance of the trophism of bone and bone marrow in the epiphyses and apophyses.
The dystrophic-necrotic process goes through five stages in succession:
- The stage of necrotic changes, which is the result of a violation of the blood supply to areas of the apophysis or epiphysis.
- The stage of a secondary fracture of the impression type, which is possible with minimal loads.
- Fragmentation stage. Involves resorption of necrotic areas of spongy bone tissue.
- Reparation stage. During this stage, connective tissue grows.
- Consolidation stage. It involves a process of ossification, in which deformations of the pineal gland are formed or it is completely restored with correct treatment.