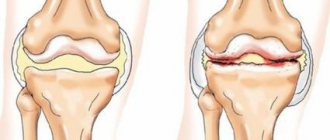
When the first symptoms appear, immediately visit a doctor; do not delay the development of the disease. Osteoarthritis is a degenerative disease consisting of the destruction of cartilage tissue and inflammation in the joints. Osteoarthritis of the metatarsophalangeal joint leads to long-term deterioration of health and decreased performance of the patient. Osteoarthritis of the toes is an irreversible change in the cartilage tissue of the joints, hyaline cartilage begins to thin and collapse, mobility and shock absorption decrease, and bone structures are damaged due to the lack of cartilage. According to statistics, the disease occurs in seven out of ten people in varying degrees of severity.
Reasons for the development of the disease
In a rheumatology journal, scientists described differences between normally aging cartilage and joint osteoarthritis, indicating that osteoarthritis is truly a disease and not just a natural consequence of aging. The main enzymes responsible for cartilage destruction are matrix metalloproteinases and anti-inflammatory cytokines (for example, IL-1). These enzymes were found in joints undergoing osteoarthritis, but not in cartilage undergoing normal aging.
A person's age is the most identified risk factor for osteoarthritis of the metatarsophalangeal joints of the feet. Prevalence rates for both radiographic and, to a lesser extent, symptomatic osteoarthritis increase sharply after age 40 in women and age 50 in men. Degenerative pathology is rare in people under 35 years of age. Secondary causes and other types of degenerative joint diseases should be considered in this population. Causes of osteoarthritis of the metatarsophalangeal joints:
- genetic predisposition;
- obesity;
- heavy load on the leg joints;
- repeated damage;
- injury;
- hypothermia;
- salt deposits;
- engaging in hazardous sports;
- wearing high-heeled shoes with improper soles.
These factors impair blood circulation in the metatarsophalangeal joints. Impaired blood circulation leads to the formation of osteoarthritis. Also, chronic arthritis and congenital abnormalities of the joints lead to the occurrence of osteoarthritis of the metatarsophalangeal joints of the foot.
Treatment of arthrosis of the metatarsophalangeal joint
Conservative treatment of the metatarsophalangeal joint is possible only at the 1st and 2nd stages of pathology development. Treatment of arthrosis of the metatarsophalangeal joint of the 3rd and 4th degree is carried out exclusively by surgical methods. During the operation, partial or complete reconstruction of the damaged joint using plastic surgery is possible.
In our manual therapy clinic, treatment of the metatarsophalangeal joints of the foot is carried out conservatively, using the following techniques:
- correction of lifestyle and diet, which allows you to eliminate the impact of negative causes and start the processes of restoration of damaged tissues;
- massage and osteopathy are used to restore tissue trophism, enhance microcirculation of blood and lymphatic fluid;
- Therapeutic gymnastics allows you to speed up the process of diffuse nutrition, restore lost elasticity of ligaments, tendons and muscles;
- laser exposure and reflexology allow you to start the regeneration process;
- physiotherapy allows you to relieve pain and improve the condition of all tissues.
If you need to undergo treatment for arthrosis of the metatarsophalangeal joints of the feet, then you can make an initial free appointment with an orthopedist at our clinic. During the consultation, the doctor will conduct an examination, make a preliminary diagnosis, and, if necessary, recommend additional examinations. An individual course of therapy will then be developed.
Clinical picture of a degenerative disease
Take care of your feet, do not let the disease develop.
Due to the physiological characteristics of the lower part of the foot, most of the load falls on the first metatarsophalangeal joint. The development of degenerative pathology begins in the thumb. As the pathological condition progresses, destruction of cartilage tissue in the second and third metatarsophalangeal joint is possible. Symptoms of the disease depending on the stage of development:
- The initial stage of osteoarthritis is characterized by transient pain in the front of the lower leg. The first metatarsophalangeal joint begins to thicken, causing slight restriction of movement. The pain is localized and worsens after prolonged physical activity. The first degree is characterized by micro-tears of the ligaments and a weak inflammatory process in them.
- The second stage of osteoarthritis is characterized by the formation of a “soft” formation in the area of deformity. There is a dysfunction of the synovial membrane. The development of degeneration of the articular capsule and synovial membrane begins. Bone growths - osteophytes - cause unbearable pain. Erosion of the cartilaginous membrane of the joint appears. The thumb begins to deviate to the side. The patient tries not to step on it because of the pain, so the clubfoot is noticeable. Callus formation is possible.
- During the third stage of disease progression, patients experience pain at rest. Stiffness that occurs in the morning, after rest or inactivity, lasts more than 30 minutes. A “solid” formation is formed in the area of deformation. The third stage is characterized by severe bone deformation, disruption of the articulation axis, and ligament insufficiency, manifested by contracture and joint instability. Subchondral osteosclerosis is formed, and cysts may form.
Osteoarthritis most often affects the first metatarsophalangeal joint of the foot. However, at the second stage of development of degenerative pathology, the destruction of the cartilaginous tissues of neighboring fingers begins; most often, deformation is observed in the 2nd and 3rd metatarsophalangeal joint. To confirm the development of the disease and determine the stage, diagnostics should be performed.
Osteoarthritis (OA) of the metatarsophalangeal joint, grade 1
Deforming arthrosis of the 1st metatarsophalangeal joint of the 1st degree is a disease that can be cured without surgery. At this stage, symptoms are minimal. This is a feeling of fullness in the joint area, a slight pain after a long walk or wearing uncomfortable shoes. The appearance of a slight swelling at the base of the big toe at the end of the day.
Osteoarthritis of the 1st metatarsophalangeal joint of the foot develops gradually, but it always has a primary attack of inflammation. This may be redness of the skin with slight swelling after a long walk or as a result of traumatic exposure. After some time, all clinical signs disappear, but a periodic feeling of discomfort remains. It appears when you try to use a certain type of shoe. Some people begin to have difficulty wearing sneakers, while other patients note that a feeling of compression appears only when trying to put on classic shoes with a tight last.
DOA of the 1st metatarsophalangeal joint at an early stage can only be successfully diagnosed using MRI examination. An X-ray, even in a correctly selected position, provides scant information about the condition of the cartilage tissue, since the joint space at this bone joint is very narrow.
If you have been diagnosed with grade 1 osteoarthritis of the 1st metatarsophalangeal joint, we recommend that you contact an orthopedist as soon as possible and begin effective treatment. Chondroprotectors and anti-inflammatory ointments will not help with this pathology. It is necessary to combine methods of manual therapy and physiotherapy, massage and therapeutic exercises.
What diagnostic measures are carried out?
Symptoms, physical examination, and radiographic changes make up the diagnostic triad of osteoarthritis, which helps determine the severity of the disease. The American College of Rheumatology has outlined classification criteria that include, but do not rely solely on radiographic findings. If cases are less obvious, differential diagnoses should be considered, such as:
- Inflammatory arthritis if there is prolonged stiffness for more than 1 hour.
- Lupus, viral and rheumatoid arthritis, sepsis, malignant tumors.
- Periarticular structural disorder (eg, bursitis, tendonitis, periostitis).
- Pain can be differentiated from neuralgia or interdigital neuroma.
X-ray examination determines the degree of formation of osteophytes, narrowing of the joint space and progression of osteosclerosis. At the first stage, these signs are absent; at the second stage, small osteophytes and moderate narrowing of the joint space appear; the third stage is characterized by significant narrowing of the joint space, subchondral sclerosis. To diagnose degenerative pathology of the toe, X-rays alone are not always enough; sometimes doctors prescribe CT, MRI, blood and urine tests to rule out other diseases.
The main methods of treating the disease
For osteoarthritis of the foot, treatment begins with reducing symptoms. Goals of therapy:
- relieve pain;
- improve mobility;
- save functions;
- reduce inflammation.
New treatments are currently being developed to reduce the activity of anti-inflammatory cytokines and stimulate cell synthesis. Treatment of first-degree degenerative pathology is based on the use of painkillers, which are non-steroidal anti-inflammatory drugs. These medications are used in the form of tablets and ointments. The following drugs have pronounced anti-inflammatory activity: Diclofenac, Piroxicam, Ketoprofen, Naproxen, Sulindac, Celecoxib. Medicines in this group should not be taken for stomach ulcers and other diseases of the gastrointestinal tract. Chondroprotectors are prescribed at the first or second stage of development, when cartilage tissue still remains on the bone structures. Medicines have a regenerating effect on joint cartilage and prevent the development of the disease. Chondroprotectors improve blood circulation in damaged metatarsophalangeal joints.
In addition to medications, physiotherapeutic procedures are required. UHF therapy, SUV irradiation, magnetic therapy, ultrasound and baths with medicinal saline solutions are successful. Physiotherapy cannot be performed in the presence of an anti-inflammatory process. These methods speed up the healing process, and the best effect is achieved when procedures are carried out in the first stages of development. At the third stage of osteoarthritis of the metatarsophalangeal joints, surgical treatment is required.
How should a sick person eat?
Patients diagnosed with osteoarthritis of the joints should follow their diet. It is important to add foods rich in antioxidants to your diet. These include:
- Vitamin E: avocado, walnuts, almonds, sunflower oil.
- Vitamin C: lemon, broccoli, parsley, bell pepper.
- Selenium: cod, shrimp, salmon, sesame.
- Beta-carotene: mango, carrots, apricot, spinach.
It is useful to eat jellied meat and jelly, as well as other products containing large amounts of gelatin. The victim's diet should not contain fatty, smoked, fried, spicy, or too salty foods. You should also avoid drinking caffeine and strong tea, baking, confectionery and sausages.
Traditional medicine will save you from the destruction of cartilage tissue
Natural restoration of cartilage does not cause as many side effects as chondroprotectors or non-steroidal anti-inflammatory drugs. Alternative treatment can reduce the drug load on the body and increase the effectiveness of the procedures. We treat osteoarthritis of the joints with home remedies:
- Melt lard and apply it warm to the damaged joint. It is recommended to use this method after a pine bath.
- Lubricate the inside of the cabbage leaf with honey, apply it to the sore finger, wrap it in cellophane and a warm scarf. Compresses should be done for 30 days.
- Burdock improves metabolic processes. Remember the leaves of the medicinal herb, apply to the joint, securing with a bandage or gauze bandage.
- 50 g of elecampane root is poured with 130 ml of vodka. The medicine is infused for 14 days, then the sore joints are rubbed.
For the treatment of osteoarthritis of the metatarsophalangeal joints of the feet, a tincture prepared from freshly picked dandelion flowers, iodine and other medicinal plants that have anti-inflammatory, regenerating and analgesic properties are suitable. Folk remedies also have contraindications; before using any herb, make sure you are not allergic to the plant.
Share this article:
Osteoarthritis of the metatarsophalangeal joints, degree 2
Also, using conservative methods of manual therapy, it is possible to successfully treat osteoarthritis of the metatarsophalangeal joints of the 2nd degree, since synovial cartilage tissue is still preserved at this stage. The most thinned hyaline cartilage in some places can even expose the heads of the bones, but with the help of laser exposure and some physical therapy methods it is possible to start the process of successful regeneration of this tissue. The most important thing for grade II osteoarthritis of the first metatarsophalangeal joint is to immediately consult a doctor for treatment.
Osteoarthritis of the metatarsophalangeal joint of the 2nd degree is much easier to recognize. With this pathology, the patient has the following symptoms:
- a feeling of rather unpleasant cutting or stabbing pain at the base of the thumb;
- difficulty walking;
- swelling around the joint and slight redness of the skin;
- visible signs of disruption of tissue trophism (skin peeling, dryness, increased sensitivity);
- crunching or clicking sounds when flexing and straightening your toes.
If such symptoms appear, immediately contact an orthopedist and undergo a full examination.