Wedge-shaped deformation of the vertebral bodies is expressed in the fact that bone tissue degenerates and the shape changes. Wedge-shaped deformity of the vertebrae can be congenital (due to a violation of osteogenesis at the intrauterine stage of development) or acquired (for example, due to an osteogenic inflammatory process, compression fracture, etc.). In children, the sphenoid vertebra may be single. In adults, several vertebrae located in the thoracic or lumbar region are often subject to destruction and deformation at once.
It is very difficult to recognize this pathology. At the initial stage, it practically does not give any clinical symptoms. Gradual deformation of the spinal column creates the preconditions for rapid destruction of the intervertebral discs. Signs of osteochondrosis often become manifest (primary) symptoms of the sphenoid vertebra in both adults and children.
In the process of its development, this orthopedic disease leads to a person experiencing constant nagging, dull pain in the back and lower back. They intensify significantly with prolonged static tension in the muscular frame of the back. Therefore, patients often do not control their posture - they begin the process of curvature and formation of a “round back” against the background of constant stooping. In some cases, scoliosis develops, combined with excessive thoracic kyphosis.
After spinal curvature, clinical signs of dysfunction of the autonomic and central nervous systems begin to dominate. Later, a clinical picture of insufficient blood supply to the structures of the brain and myocardium appears. Vital lung capacity may be significantly reduced.
Such conditions should not be allowed to develop. A wedge-shaped vertebra is a condition in which it is possible to correct the performance of the muscular frame of the back in such a way that negative consequences will not develop. Therefore, make an appointment with a chiropractor in our clinic and receive a comprehensive consultation. The first appointment for each patient is provided completely free of charge.
About the disease
Picture of the course of the disease
A sphenoid vertebra is an anomaly of skeletal development, manifested in underdevelopment of the body and vertebral arch. Usually the disease is congenital, but sometimes it is a consequence of acquired pathologies of the skeletal system.
A normal vertebra consists of a body, an arch, and a spinal canal. The body is located in front, the arc is located behind. The spinous and articular processes extend from the arch. The processes connect the spine and muscles.
The formation of the spine begins from conception. First, membranous vertebrae are formed, then they are replaced by cartilage tissue. Ossification of cartilage occurs at 8 weeks of intrauterine development. Sometimes a malfunction occurs and the embryo’s vessels grow in incorrectly. Thus, the arch or body of the vertebra only develops halfway, and it itself becomes wedge-shaped.
Degrees and classification
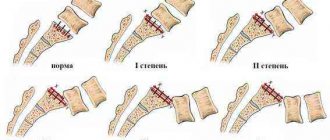
From a developmental point of view, wedge-shaped vertebrae are inactive and active .
Inactive ones remain unchanged throughout life and can be fused with neighboring vertebrae. This phenomenon is called blocking. The active ones continue to grow and develop. This is an unfavorable course of the disease, as it leads to severe deformation of the spine.
Wedge-shaped deformity of the vertebrae can be active or inactive
The focus of localization can be in any department, but most often the anomaly occurs in the lower thoracic or upper lumbar region. The vertebra may be curved in the front, back or side. Also, the deformation can be single, double or multiple.
Sometimes two wedge-shaped vertebrae are located between two normal ones in a mirror position. Thus, they neutralize each other. This is called "alternating" vertebrae. This scenario is considered the most favorable, since the curvature is local.
ICD code
According to ICD 10 it has code Q76.4.
Prevalence
The most severe anomaly is several vertebrae deformed on one side, located next to each other. Fortunately, this phenomenon is very rare. .
Causes of wedge-shaped vertebrae
The wedge-shaped shape of the vertebrae can occur for many reasons; we will consider only the main ones. It’s worth starting with a description of the vertebra itself. This is a complex bone in its structure. Its composition is determined by a rectangular cuboid base. The lateral arches and spinous processes extend from it. These structures form an oval ring, which subsequently becomes part of the walls of the spinal canal.
The shock-absorbing and physical load is placed on the rectangular cuboid part of the vertebra. It is protected from destruction by intervertebral cartilaginous discs. They are filled inside with the gelatinous fluid of the nucleus pulposus - it evenly distributes all the loads.
At the intrauterine stage of fetal development, a pointed wedge-shaped shape of the vertebrae occurs in cases where the formation of the epiphyseal plate is disrupted. In the later stages of pregnancy, the development of blood vessels can have a negative impact. If they are insufficient, the base of the vertebrae is deformed.
Risk factors for the development of pathology in the fetus are:
- incorrectly composed diet of the expectant mother;
- smoking and drinking alcohol by parents during the period of conception;
- arterial hypertension, especially combined with nephropathy and eclampsia in pregnant women;
- diseases of the endocrine system in women (diabetes mellitus, pituitary insufficiency, increased production of adrenal and thyroid hormones);
- work in conditions of environmental pollution with harmful gases and salts of heavy metals;
- radiation exposure to a growing fetus;
- use of antibiotics and a number of other pharmacological drugs.
Acquired forms of wedge-shaped vertebral deformity can develop at any age. Often the disease manifests itself at the age of 6–7 years or at the onset of puberty at 12–14 years. Then orthopedic pathology develops extremely slowly. Severe clinical symptoms can occur in a person aged 25–30 years.
Rapid deformation of the vertebral bodies can be caused by the following reasons:
- metastases of tumors to the base of the vertebra;
- purulent melting of bone tissue due to osteomyelitis, tuberculosis or syphilis;
- dystrophic degenerative processes in the tissues of the spinal column;
- traumatic effects causing compression fractures, cracks, etc.;
- spinal tumors;
- thoracic and lumbar osteochondrosis in the stage of pronounced protrusion of the fibrous ring of the intervertebral disc.
During menopause, wedge-shaped deformation of the vertebral bodies in women may be associated with the development of osteoporosis. Therefore, when pathology is detected, densitometry is necessarily performed to determine bone density. Corrective therapy, including hormonal replacement therapy, is prescribed as necessary.
Causes
The main reason for the formation of wedge-shaped vertebrae is a failure in the development of the embryo.
The spine can become deformed due to heredity. Provoking factors are :
- Hereditary pathology. Usually this is Scheuermann-Mau disease, which is transmitted through generations.
- Endocrine disorders in the mother.
- Poor nutrition during pregnancy.
- Infections, especially those suffered in the first trimester.
- Unfavorable environmental conditions.
- Hard work during pregnancy.
- Severe stress.
As for the acquired disease, it can be provoked by the following factors:
- Back injuries.
- Neoplasms in the spine.
- Inflammatory process in the spine.
- Osteoporosis.
- Systemic diseases associated with metabolic disorders.
- Granulomatosis (inflammation of the vascular walls).
Video: “Kyphosis: how to straighten the hump on your back?”
Diagnostic methods ↑
Since in order to prescribe effective treatment it is extremely important for the doctor to have a clear understanding of the condition of each vertebra and the nature of the existing wedge-shaped deformities, various methods can be used for diagnosis.
They can have varying degrees of information content depending on the type of wedge-shaped deformity and the location of the hemivertebra.
Magnetic resonance imaging
Read also…. How to treat spondylolisthesis?
MRI or magnetic resonance imaging, according to many experts, is the method of first choice in the differential diagnosis of wedge-shaped deformity of the vertebrae.
Unlike other methods of radiation diagnostics, MRI provides a more complete picture, allowing you to study the condition of the vertebrae, spinal cord, epidural space, discs, and dural sac.
Wedge-shaped deformation of the vertebrae often occurs as a result of damage to the spinal cord.
Therefore, this research method is advisable to use when examining patients with symptoms indicating the possibility of wedge-shaped displacement of the vertebrae or their deformation.
Radionuclide method
The radionuclide method, or osteoscintigraphy, is used in the differential diagnosis of wedge-shaped deformities of the vertebrae, especially in cases where it is caused by metastatic lesions.
The radionuclide method is used in combination with magnetic resonance imaging, since it has more limited capabilities in diagnosing local vertebral lesions.
Photo: image obtained by osteocintigraphy
X-ray computed tomography
X-ray computed tomography allows:
- it is enough to objectively assess the condition of the affected vertebra, paravertebral soft tissues, and disc;
- accurately determine the pathomorphological substrate of the lesion.
- thanks to contrast enhancement, confirm or exclude the oncological nature of pathological processes.
Photo: wedge-shaped vertebral deformity
However, the method has a number of significant disadvantages:
- allows you to see the extent of the spread of pathological processes only at the level of several vertebral segments;
- RCT reconstruction is performed exclusively in the axial plane, which does not always make it possible to obtain a good quality image;
- data on the contents of the spinal canal are also uninformative.
Consequences
If the disease was not diagnosed at an early age (2-4 years) and treatment was not started, it will lead to serious consequences. The disease will progress, and correction will become impossible, since from 6 to 20 years of age the final ossification of the spine occurs.
The most severe consequences of the pathology:
- Scoliosis, kyphosis, lordosis.
- Hump.
- Disruption of internal organs.
- Decreased oxygen supply to the brain.
All this leads to external deformities, disability, and death.
Symptoms
If the vertebral deformity is severe, the clinical picture will be clear. However, the symptoms are uncharacteristic, so patients often take them lightly or associate them with other diseases.
The most typical manifestations of wedge-shaped vertebrae:
- Severe pain, intensifying after physical activity or prolonged stay in one position. The pain is localized in the area of the spine where the deformity occurred.
- Difficulty breathing and shortness of breath. Occurs with wedge-shaped vertebrae of the thoracic region. This is due to a decrease in lung volume.
- Migraines (with an abnormality in the cervical spine).
- Increased fatigue.
- Malfunctions of the gastrointestinal tract.
- Displacement of internal organs.
- Slouch.
- Chest deformity.
- Unilateral divergence of ribs.
Diagnostics
Did you know that...
Next fact
To diagnose wedge-shaped vertebrae, it is necessary to undergo examination by several specialists: a neurologist, a vertebrologist, and an orthopedist. To assess the condition of internal organs, additional consultations with a pulmonologist, cardiologist, or gastroenterologist may be necessary.
It is possible to detect deformation using an X-ray of the spine , but this method is not sufficiently informative. For example, altenating vertebrae are very difficult to detect using radiography. It is also difficult to understand the condition of the intervertebral discs, blood flow and other important points necessary for choosing therapy.
The most informative study is MRI . With its help, the presence of pathology in the discs and epidural space is accurately determined. If there is a suspicion of a tumor or metastases in the spine, a CT scan . This method examines a specific part of the spinal column.
You can learn more about the initial stages of spinal curvature in the following articles:
- Scoliosis 1st degree
- Scoliosis 2 degrees
- Kyphosis 1st and 2nd degree
Publications in the media
Most often in adults, less durable vertebrae break at the points of transition from one physiological curvature to another: lower cervical, upper thoracic, lower thoracic and upper lumbar. Causes: axial load on the spine, sudden or excessive flexion or extension of the spine. Classification of fractures by stability. Stability is determined by the integrity of the posterior ligamentous apparatus and intervertebral joints • Stable injuries •• Angle avulsion •• Wedge-shaped compression of less than 50% of the height of the vertebral body •• “Blast” fractures that occur under axial load without flexion and extension of the spine; in this case, the vertebral end plates break, the central sections of the intervertebral disc are embedded in the vertebral body and tear it from the inside into several fragments according to the principle of water hammer • Unstable injuries •• Dislocation and fracture dislocation of the vertebra •• Fracture with wedge-shaped compression of more than 50% of the height of the vertebral body in the anterior section •• Flexion-rotation fracture.
Clinical picture • Pain in the damaged part of the spine • Bruising and abrasions at the point of application of force • Changes in physiological curvature: smoothing of the lumbar lordosis, increased thoracic kyphosis, scoliosis • Symptom of the reins - tension of the long back muscles in the form of rollers on both sides of the spinous processes of the damaged vertebrae • Pain upon palpation of the spinous processes of damaged vertebrae • Protrusion of the spinous process posteriorly and an increase in the interspinous spaces at the level of injury • With a fracture of the lumbar vertebrae - abdominal pain, tension in the muscles of the anterior abdominal wall, pseudo-abdominal syndrome - clinical picture of an acute abdomen, developing with irritation or damage to the solar plexus and border sympathetic trunk retroperitoneal hematoma • Silin's symptom - increased pain on palpation of the spinous processes while raising straight legs in a supine position. Diagnostics . An X-ray examination is carried out in two projections, and, if necessary, targeted radiography, tomography of the spine, radiography in lateral projections, CT, MRI. Radiographs reveal a wedge-shaped deformity of the vertebral body in the lateral projection.
Treatment • Fracture of the lower thoracic and lumbar vertebrae •• The patient is transported on a special stretcher with a shield that prevents flexion of the spine •• Simultaneous reposition followed by application of a corset is indicated for wedge-shaped compression of more than 50% of the vertebral body ••• Anesthesia: 20 are injected into the interspinous space above the broken vertebra ml of 0.5% procaine solution (Behler's method), an analgesic is administered subcutaneously ••• Reposition is carried out according to the Watson-Jones-Behler method (extension of the spine on tables of different heights) or Davis (pulling up by the legs of a patient lying down face) ••• An extension plaster corset is applied, leaving the back open for 4–6 months ••• Physiotherapy, massage, exercise therapy are prescribed •• The Dreving-Gorinevskaya functional method is indicated for compression of less than 1/3 of the height of the vertebral body ••• Bed rest is prescribed and longitudinal traction for the axillary fossae on an inclined board for 1.5–2 months ••• Exercise therapy is prescribed from the first days of bed rest to create a muscle corset •• Method of gradual reposition ••• Reposition is carried out by gradually increasing the extension of the spine by placing wide rollers under lumbar region for 7–10 days ••• Exercise therapy, massage, physiotherapy are performed ••• On 15–20 days an extension corset is applied for 4–6 months •• Open posterior fixation of the spine is used for uncomplicated flexion fractures ••• A broken vertebra is straightened before surgery, simultaneously or gradually ••• Fixation of the spinous processes, arches, transverse processes of the damaged part of the spine is used ••• After the operation, exercise therapy and massage are prescribed to strengthen the back muscles •• In case of “burst” fractures, bone fragments are removed, the vertebral body is replaced with a bone graft • Fracture of the midthoracic and upper thoracic vertebrae. For fractures of the upper thoracic vertebrae up to TV, traction is applied not to the axillary fossae, but to the head with a Glisson loop.
M KB-10. T08 Spinal fracture at unspecified level
Treatment
The choice of treatment tactics depends on the initial data. The following factors are taken into account: the stage of the pathology, the activity of the wedge-shaped vertebrae, the presence of concomitant diseases. Conservative treatment and surgical intervention are used.
Conservative treatment
Conservative treatment is prescribed for minor curvatures and Scheuermann-Mau disease. The operation is not advisable, since it is traumatic and requires long-term rehabilitation .
Conservative treatment is used if the curvatures are minor, such as in Scheuermann-Mau disease
The following methods are used to correct pathology::
- Physiotherapy.
- Massage.
- Manual therapy.
- Swimming.
- Wearing orthopedic products.
- Spa treatment.
Physical therapy involves performing a special complex developed by a doctor. Every day you need to do gymnastics to strengthen the muscle corset and restore back flexibility.
The massage is performed by a therapeutic massage specialist. The patient's blood circulation and metabolism are normalized, and muscles are strengthened. It is recommended to take 2 courses per year, 10 sessions each.
Manual therapy is based on gentle techniques. The qualifications of the specialist are of decisive importance. You cannot interrupt the course of treatment, even if the pain increases. Swimming is the most optimal and beneficial type of activity for back problems. In water, muscles relax, on the other hand, individual muscle groups develop and strengthen.
For scoliosis or kyphosis, special orthopedic products . For example, a Chenault corset, a Boston corset, a simple support bandage. These devices are used even with severe curvatures. They support the back in the desired position and relieve excessive muscle tension.
The use of medications is symptomatic. To relieve pain and reduce inflammation, nonsteroidal anti-inflammatory drugs, muscle relaxants, and antispasmodics are used. The choice of remedy is made by the doctor after a complete examination.
Surgery
Surgical treatment allows you to stabilize deformed vertebrae. If the pathology has reached a large extent and continues to progress, then the only option is surgery.
It is indicated in the following cases: scoliosis or kyphosis of 3-4 degrees, disruption of the functioning of internal organs, severe pain syndrome that is not relieved by conventional drugs, cerebrovascular accident.
For wedge-shaped vertebrae, the following surgical methods are used::
- Spondylodesis is the fusion of vertebrae using implants.
- Anteroposterior episiospondylodesis. A special structure is installed that blocks the growth of bone tissue in the convex area. At the same time, on the concave side the vertebrae continue to grow. This method is used to treat children whose spinal development has not yet been completed.
- Vertebral excision. The deformed vertebra is removed completely or part of it.
Video: “Technique for performing surgery to correct the spine”
All about wedge-shaped spinal deformity
It takes a lot of time to eliminate any problem with the spine. Wedge-shaped spinal deformity is no exception. The treatment process consists of many stages and depends on the degree of deformation, location of occurrence, the presence of other diseases, the age of the patient and many other factors.
Causes of pathological changes
Deformation occurs for various reasons, of which the following are distinguished:
- Congenital. Formed during intrauterine development. The development of the fetus is affected by: stress, nutrition, environmental conditions, genetics (genetic defects), medications that a woman takes during pregnancy and infectious diseases suffered during this period.
- Purchased. They occur in diseases of the spine, fractures, dislocations, hazardous working conditions, osteoporosis and cancer. When diagnosing, it is impossible to single out a separate cause; most often there are several problems that ultimately led to such a consequence.
Classification of wedge deformity
Depending on the location: side, front and rear. According to the number of affected vertebrae: single, double and multiple. Most often, such an anomaly forms in the lower part of the chest, less often in the upper parts of the spine.
Vertebrae with wedge-shaped deformity are able to further develop and grow, but this can lead to progression of the pathology. If they do not grow, they often fuse with neighboring vertebrae and impair mobility in this area. All this can provoke disruption of the functioning of internal organs, the spinal column itself, as well as muscles, nerves and blood vessels and ultimately lead to disability.
Symptoms
With a wedge-shaped deformity of the spine, the very first thing that begins to bother you is pain in the damaged area. At first it is temporary, if a person has overexerted himself or made a sudden movement, or suffered something heavy. But if you don’t see a doctor in time, you will experience constant pain.
As the deformity progresses, the pain becomes greater and begins to radiate to different places (groin, abdomen, legs, arms). Numbness, burning, weakness, fatigue appear, reflexes and sensitivity decrease. With severe curvature, discomfort and pain in the chest, increased pressure, difficulty breathing, indigestion occur, and ultimately paresis or paralysis occurs.
With the development of pathology in the cervical spine, the symptoms change slightly. Characteristic for this type of pathology are sleep disturbances, headaches and fainting. The anomaly forces a person to give up work and is a cosmetic defect that causes discomfort and can lead to depression.
Diagnosis of changes in the spinal column
This pathology can be detected during a standard external examination, but in more complex cases and for greater information, specialists can also prescribe X-rays, ultrasound, MRI and CT. A general and biochemical blood test is required, which can show abnormalities in the functioning of the body as a whole, and hormonal tests. Doctors also recommend undergoing a full range of examinations, which includes a trip to a neurologist, traumatologist, surgeon and cardiologist. .
Treatment is prescribed individually, based on many factors, patient tests and the degree of deformity. But in any case, spinal rehabilitation
takes a lot of time.
This may include:
- Conservative treatment. If there are no significant deformations and complications, then in this case they can manage by eliminating symptoms and prophylaxis to prevent further development of the disease.
- Drug therapy. The doctor prescribes medications only if there is severe pain that does not go away. Depending on the degree of pain, medications and their form (tablets, ointments, injections) are selected.
- Physiotherapy. Physiotherapeutic procedures are prescribed as an auxiliary therapy in order to eliminate swelling or inflammation, relax, and normalize blood circulation. Massage is included in this type of treatment. But this should be a therapeutic massage performed by a professional with medical education.
- Therapeutic gymnastics and swimming. This is more of a prevention before or after problems with the spine. Regular trips to the pool and sports will strengthen the muscle corset and help get rid of pain. Therapeutic gymnastics is selected for each person individually, depending on the degree of deformation and physical condition.
- Orthopedic correction. Sometimes experts suggest wearing a special corset that is aimed at traction of the spine
. - Surgery. If the deformity progresses further and the above methods do not help, then surgery is prescribed.
Prevention
It is necessary to constantly monitor your health. Problems with the spine affect a person’s quality of life.
Prevention of congenital pathology:
- Be sure to watch your diet. It is necessary to consume enough fruits, vitamins, protein and calcium.
- Protect yourself from diseases. Avoid infections.
- If you work in a dangerous enterprise, you should stop working during pregnancy.
- Don't overexert yourself.
- More fresh air.
- It is necessary to give up bad habits (alcohol, cigarettes, etc.)
- Do not take medications (even vitamins) without your doctor's approval.
If a diagnosis has already been made, then you need to strengthen your muscle corset.
If this is a child, then diversify his leisure time, enroll him in sports clubs, limit the use of gadgets, etc. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Prognosis and prevention
The prognosis of the disease depends on several factors:
- stages of pathology;
- activity of the sphenoid vertebrae;
- patient's age;
- timeliness of diagnosis and therapy.
The most favorable prognosis will be if the wedge-shaped vertebrae do not grow and the curvature is local. An unfavorable prognosis occurs with active vertebrae. In this case, the growth of the spinal column occurs unevenly and can lead to the formation of a hump.
Prevention of the disease is:
- Healthy lifestyle.
- Avoiding back injuries and excessive physical activity.
- Timely treatment of infectious diseases.
- Physical education class.
- Regular preventive examinations by an orthopedist for patients at risk.
- Properly selected furniture for sleeping and working.
Prevention
Wedge-shaped deformity is a disease that needs to be actively combated, and not left to chance. Worsening of the anomaly can lead to serious problems with the spine and negatively affect the functioning of the heart, respiratory and nervous systems.
Expectant mothers should be especially attentive to their health.
Prevention of wedge-shaped deformity in the fetus:
- Carefully monitor your diet and lifestyle, be sure to walk in the fresh air several times a day. The diet must contain proteins, calcium, and B vitamins.
- Avoid contact with infectious patients.
- If you work in hazardous work, provide the HR department with a certificate of pregnancy, which gives you the right to switch to light work. The longer you work in hazardous conditions, the higher the risk that your child will have serious health problems. This is not just about wedge-shaped muscle deformity.
- Take care of your health - if you feel unwell, you should seek medical help. Pregnant women have a weakened immune system, so chronic and previously asymptomatic diseases can make themselves felt. This “surprise” may especially arise for women who have not been planning a pregnancy.
- Give up bad habits, otherwise wedge-shaped deformation is not the worst thing you will have to face.
- Avoid stressful situations - it’s not for nothing that women are protected in every possible way from unnecessary worries and negative emotions. Stress is one of the main causes of the development of life-threatening pathologies.
- Do not take medications without the advice of a doctor - the usual painkillers that you always took before pregnancy can negatively affect the development of the child. If it is not possible to consult with a specialist, at least read the instructions carefully.
Prevention of progression of wedge-shaped muscle deformity
If a person has already been diagnosed with a wedge-shaped muscle deformity, efforts must be made to prevent the situation from getting worse. The best way to maintain the health of your spine is to strengthen your muscular system through sports. This does not mean that it is necessary to torture a child with physical activity around the clock. Regular attendance at one or two sports sections will be enough.