Osteochondrosis is the most severe form of degenerative-dystrophic damage to the spine, which is based on damage to the nucleus pulposus of the intervertebral disc, with subsequent deformations of the bodies of adjacent vertebrae, intervertebral joints, disorders of the ligamentous apparatus, and involvement of the nervous system and blood vessels in the pathological process.
One of the most common forms of osteochondrosis is lumbar osteochondrosis , or, more precisely, the lumbosacral spine. Many people - both men and women - are familiar with back pain in the lumbar region, sacrum, and lower extremities, caused by various types of lumbar osteochondrosis and its complications. Among the causes of temporary loss of ability to work and disability, this disease occupies one of the first places.
The course of the disease is chronic, usually with periods of exacerbations. Most often, exacerbations of lumbar osteochondrosis are provoked by lifting and carrying heavy objects, hypothermia, stress, and injury.
Osteochondrosis of the lumbar spine - causes, mechanism of occurrence and development
No clear cause of osteochondrosis has been identified; the disease is considered multifactorial. The most popular theory is that the cause of spinal osteochondrosis is considered to be constant muscle overstrain or muscle hypotension, non-physiological muscle tension, which leads to overload of the vertebral segments, deterioration of their blood supply and, ultimately, to degeneration of the intervertebral discs and joints, which results in osteochondrosis.
The cause of premature aging of intervertebral discs can also be endocrine and metabolic disorders, hereditary predisposition to the development of osteochondrosis, autoimmune disorders, and microtraumas. The negative role of visceral, that is, associated with internal organs, pathologies in the development of spinal osteochondrosis has also been proven. Unfavorable heredity plays a significant role in the development of the disease. The contribution of hereditary factors to the appearance of lumbar osteochondrosis is about 60%, the rest is attributed to factors of adverse external influences on the spine.
Factors contributing to the development of osteochondrosis in both the lumbar and other parts of the spine are very numerous. The main ones are: incorrect posture, physical inactivity, muscle strain in the lumbar region as a result of constant carrying of heavy objects or sudden excessive load, hormonal changes, endocrine and somatic diseases, disruption of the normal blood supply to spinal tissues, emotional stress, age-related changes, poor nutrition. Under the influence of these factors, the processes of dehydration and circulatory disorders, arthrosis and subluxations in small joints, bone growths, prolapsed discs - hernias, gradually increase in the structures of the spine.
The most obvious causes of lumbar osteochondrosis are most often considered to be a sedentary lifestyle and back injuries. Therefore, the risk group primarily includes those people whose profession is directly related to stress on the back. This is a very wide range of professions - salespeople and waiters, surgeons and teachers - everyone who is forced to spend most of their working time standing. The risk group includes builders and loaders, as well as athletes whose occupation places heavy stress on the spine. In addition, drivers, various office workers, programmers suffer from osteochondrosis of the lumbar region - that is, those who have a mostly sedentary job and who suffer from physical inactivity.
Diagnosis of the disease
The doctor makes a preliminary diagnosis based on characteristic complaints and examination data. Pain in certain points, muscle tone, sensitivity, range of motion, and posture are assessed. Instrumental research methods help clarify the stage of osteochondrosis and confirm the diagnosis. Most often, at the initial stage, an x-ray of the spine of interest is prescribed. The pictures clearly demonstrate whether there is a reduction in the distance between the vertebrae, that is, whether there is thinning of the cartilage, and how far the process has progressed. If, based on the results of the X-ray, the doctor suspects the presence of intervertebral hernias, he will prescribe a more informative research method - magnetic resonance imaging (MRI). Layer-by-layer scanning and good visualization of soft tissues make it possible to confirm or refute the diagnosis of intervertebral disc herniation with absolute accuracy.
Symptoms of osteochondrosis of the lumbar spine
With lumbar osteochondrosis, pain of a different nature is possible. This can be either aching pain that occurs during prolonged sitting or after sleep, or sharp shooting pain that catches you in the most uncomfortable position and does not allow you to straighten up. Pain is caused by pinched nerve roots, irritation of the spinal column's own nerves, swelling and irritation of the muscles and ligaments located in the innervation zone of the lumbar spine.
Pain syndrome can be caused by compression of the radicular structures (radiculopathy), compression of the spinal cord (compressive myelopathy), damage to the spinal cord due to impaired blood supply due to compression, narrowing (stenosis) of the supply arteries and veins (compression-vascular myelischemia).
The cause of compression may be: protrusion and herniation of intervertebral discs, spondylolisthesis (sliding of the vertebra forward in relation to the underlying one), proliferation of osteophytes and cartilage tissue in the spinal segment. As a result, osteochondrosis of the lumbar spine leads to a narrowing of the canal through which spinal nerves or vascular structures pass, and under certain conditions (awkward movement, physical activity, unsuccessful rotation of the body, etc.) compression (squeezing) may occur. Compression of nerve structures leads to various pain syndromes and muscle spasms. Compression of blood vessels causes disruption of blood supply - ischemia of the organ that is supplied by this vessel or artery begins.
Clinical syndromes of osteochondrosis of the lumbar spine
The clinical picture of lumbar osteochondrosis is determined by a complex of vertebral symptoms (changes in the statics and dynamics of the lumbar spine) and extravertebral symptoms, which mean dysfunction of neurological and vascular structures in the lumbosacral region of the spine.
Vertebral syndromes of lumbar osteochondrosis
In lumbar osteochondrosis, vertebral syndrome is characterized by the following set of symptoms:
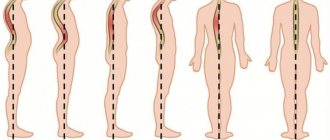
- violation of the configuration of the vertebral functional-anatomical segment: flattening or (less often) increased lordosis, scoliosis or lordoscoliosis is observed;
- impaired mobility in the lumbar region, decreased range of motion, muscle-tonic imbalance caused by tension in both deep and superficial multi-joint muscles.
- local pain and tenderness during active and passive movements, which causes reflex tonic muscle tension
- violation of the spring-motor functions of both the intervertebral disc and the vertebral-motor segment as a whole.
- local pain (increased sensitivity) of the osteoligamentous structures of the spine in the affected area (pain on palpation, local (regional) vertebral and/or vertebral pain syndrome).
It is important to note that with osteochondrosis of the lumbar region, vertebral pathologies are always observed. The presence of signs of myelopathy, radiculopathy and myeloradiculopathy without obvious clinical and morphological signs of vertebral syndrome requires, as a rule, a more in-depth examination of the patient for primary (“non-vertebrogenic”) damage to the nervous system.
Extravertebral (reflex and compression) syndromes in osteochondrosis of the lumbar spine
Extravertebral syndromes are divided into two large groups: reflex and compression.
Reflex syndromes precede compression syndromes and are caused by irritation of the receptors of the nerve roots emerging from the spinal canal through the intervertebral foramina. Irritation can be caused by intervertebral hernia, bone growths, as well as vascular disorders (swelling, poor circulation), inflammation. In some cases, this leads to intense pain, which occurs not only locally, but also along the nerve at a distance from the site of irritation - the so-called “referred pain.” Referred pain can be short and sharp (“lumbago”) or dull and prolonged. In the area of innervation of the damaged nerve, autonomic disturbances (burning, goosebumps, impaired sensitivity) are possible. Possible myofascial pain - muscle spasm, which leads to limitation of movements.
Reflex syndromes include lumbago (“lumbago”) in the acute development of the disease and lumbodynia in the subacute or chronic course.
Compression syndromes are syndromes that occur as a result of compression, pinching of nerves, blood vessels, and the spinal cord in the area of the lumbar spinal motion segments. Compression syndromes in osteochondrosis of the lumbosacral region are divided into radicular and vascular-radicular. A special case of compression syndrome is myelopathy—infringement of the spinal cord.
Radicular syndromes (radiculopathy) are usually caused by disc protrusions, causing pinching of the spinal roots. The radicular symptoms that arise correspond to the level of the affected spinal segment. The L4-S1 roots are most often affected.
Vascular-radicular neurological disorders are caused by compression of the hernia on the root and the radicular artery passing along with it. In this case, “paralytic sciatica” can develop catastrophically quickly, characterized by peripheral paresis or paralysis of the extensor muscles of the foot. In such cases, the appearance of motor disorders is accompanied by the disappearance of pain.
Even more severe neurological manifestations are caused by disruption of the blood supply to the spinal cord due to damage to the radicular arteries. In this case, chronic discirculatory myelopathy develops, usually at the level of the lumbar enlargement of the spinal cord.
The most unfavorable variant of lumbar vertebrogenic radicular syndromes is compression of the cauda equina - the so-called caudal syndrome. Most often it is caused by a prolapsed median disc herniation, which compresses all the roots at the level of the affected segment.
Stages of spinal osteochondrosis
Osteochondrosis is a progressive disease, but the transition to each subsequent stage occurs gradually. One of the stages of development of osteochondrosis is the so-called disc herniation. The discs are composed of a hard shell called the annulus fibrosus and a semi-liquid core. Disc herniations occur when the fibrous ring of the disc becomes thinner and ruptures, the nucleus protrudes through the gap, and the nerve roots are compressed, which is accompanied by increased pain and an even greater decrease in the shock-absorbing properties of the disc. The rate at which symptoms develop depends on lifestyle, treatment, and individual characteristics of the body.
Stage 1
Characteristic complaints appear, constant or periodic. They are often provoked by physical activity or forced body position. The x-ray shows minimal narrowing of the intervertebral spaces or normal.
Stage 2
Symptoms intensify as the disc loses stability (the cartilage tissue bulges into the surrounding annulus fibrosus), which compresses the nerve roots. An x-ray shows a noticeable reduction in the intervertebral distance or displacement of the vertebrae; bone tissue growths may appear.
Stage 3
Herniated intervertebral discs, also called protrusion or disc prolapse, appear; the disc extends more and more into the surrounding tissues, which leads to damage to blood vessels and nerves, so the pain intensifies, limiting movement in the limbs and causing numbness.
Stage 4
Stage of disc fibrosis. The disc hardens, it is replaced by scar tissue, bony protrusions grow along the edge, and the intervertebral distance noticeably decreases. The mobility of the spine is significantly reduced - it literally becomes ossified.
Clinical classification of lumbar osteochondrosis. Degrees of osteochondrosis
Classification of lumbar osteochondrosis by degree is used to systematically characterize the clinical manifestations of the disease. This classification systemically describes the symptoms of the disease and begins from the moment the patient experiences pain.
1st degree of osteochondrosis
Occurs when an intervertebral disc ruptures, caused by sudden movement or overexertion. It manifests itself as sudden pain, a feeling of electric current passing in the spine, and the muscles are reflexively tense.
2nd degree osteochondrosis
The second degree can manifest itself in the form of symptoms of intervertebral protrusion and spinal instability. Chronic pain that worsens with exercise. Intervals of remission and exacerbation alternate. The cervical spine is characterized by neck pain that worsens after a long stay in one position, headaches, arm pain, shoulder pain, periodic discomfort or numbness in the fingers. For the lumbar region - pain in the lower back, pain in the gluteal region, periodic pain in the sacrum, frequent fatigue in the legs.
3rd degree osteochondrosis
Manifests itself in the form of symptoms of a herniated disc (pain along the affected nerve, numbness in the arms or legs, changes in gait, headaches) or long-term symptoms of a herniated disc (in the cervical region: frequent headaches, tinnitus, dizziness, decreased vision, hearing , muscle strength in the arms; in the thoracic region: irregular heart rhythm, difficulty breathing; in the lumbar region: kidney disease, gastrointestinal tract, sexual dysfunction, numbness or weakness in the legs).
4 degree osteochondrosis
It is generally accepted that the fourth degree of osteochondrosis begins from the moment when the hernia no longer manifests itself, the manifestations of the disease may decrease, but the symptoms of spinal instability, slipping or twisting of the vertebrae, or their complete fixation relative to each other still remain. They may be joined by manifestations of proliferation of the vertebral bodies (osteophytes), which can also compress the spinal nerves or block the spinal canal (secondary spinal canal stenosis) and compress the spinal cord (spinal cord ischemia). In addition, the fourth degree includes the consequences of surgical intervention if the hernia was removed promptly (various types of innervation disorders, paresis, inflammation).
Treatment of osteochondrosis of the lumbar spine
If you experience acute lower back pain for the first time, you should definitely consult a doctor to establish a diagnosis in order to rule out an attack of renal colic, appendicitis, or any other disease that requires emergency medical care.
If the cause of back pain is known, and this is an exacerbation of osteochondrosis of the lumbar spine, first of all it is necessary to reduce the load on the spine as much as possible. You need to stay in bed for 3-7 days - sometimes this is the only way to significantly reduce pain. But to speed up recovery, proper, that is, effective, treatment is necessary. It should stimulate the human body’s own protective and healing processes. Treatment should take into account the localization of the lesion, the stage of the disease, the functional state of the body and its individual systems. Surgical treatment of this disease is indicated only in very severe cases. Most often, various methods of conservative treatment of osteochondrosis are used.
Conservative treatment of lumbar osteochondrosis
Conservative treatment methods are primarily drug treatment. In order to reduce pain, as well as to reduce inflammation, which is often the cause of vertebral syndrome, nonsteroidal anti-inflammatory drugs (NSAIDs) are prescribed in the form of tablets or, in acute cases, in the form of injections. Sometimes after an injection of an analgesic, the pain subsides and does not return even when the drug expires. This means that the vicious circle in which pain leads to muscle spasm, and muscle tension, in turn, increases pain, has been broken. However, if the pain continues for a long time, it is important to remember that NSAIDs usually have various side effects and, when taken for a long time, can cause unwanted complications - a decrease in the number of leukocytes in the blood, complications from the gastrointestinal tract.
Often, to improve the general condition of patients, sedatives (calming) drugs are prescribed for 1-3 weeks, as well as small doses of antidepressants. For osteochondrosis of the lumbar spine, novocaine blockades are performed if necessary. Recently, anticonvulsant drugs have been successfully used to relieve pain.
To reduce compression syndromes, manual therapy, traction treatment (spinal traction) and, in special cases, surgery are used.
When the fixation properties of the ligamentous-articular apparatus of the spine are weakened, it is recommended to use fixation devices - corsets, collars, bandages, etc. However, fixation devices can only be used for a limited time, since muscle weakening is observed when using them. And for patients with spinal osteochondrosis, it is extremely important to strengthen their own muscle corset in the future.
After relieving acute symptoms, the task of creating muscle fixation comes first, and then stimulating the processes of regeneration of damaged structures. For this purpose, therapeutic exercises, reflexology, and massage are used. For this purpose, chondroprotectors are used (drugs for restoring cartilage tissue). As well as drugs that improve the condition of blood vessels (angioprotectors), vitamins, primarily group B, calcium preparations that improve the condition of bone tissue.
Physiotherapeutic procedures are widely used to treat spinal osteochondrosis. They reduce pain and swelling of tissues, improve blood circulation, and stimulate muscle fixation. Procedures can be combined and alternated. Physiotherapeutic treatment methods that can be used include:
- darsonvalization of the affected area of the back and affected limbs;
- electrophoresis;
- low-energy laser radiation;
- ultrasound;
- exposure to a magnetic field;
- thermal procedures
In sanatorium conditions, mud, ozokerite, paraffin baths, radon, sulfide, hydrogen sulfide, turpentine and other baths are successfully used;
It must be remembered that the development of full regeneration requires a fairly long period of time; under favorable circumstances, it occurs in the sixth month. Therefore, treatment must be long-term. It should be carried out in combination, that is, combine medications with physiotherapy and exercise therapy.
Manifestations and treatment options for thoracic osteochondrosis in women
Osteochondrosis is increasingly becoming a problem for the working population of the country. This pathology can be caused by people leading a sedentary lifestyle. I would like to dwell in more detail on the manifestations of osteochondrosis of the thoracic vertebrae specifically in the weaker sex.
What is characteristic of the disease?
Osteochondrosis manifestations in the thoracic spine in women are caused by both degenerative and dystrophic lesions of the thoracic vertebrae. The vertebrae and the tissue connecting them are subject to destructive processes. Destructive phenomena are a consequence of disruption of the supply of nutrition to tissues, which in turn is provoked by low mobility both at work and at home. A sitting position of the body is not physiologically natural for the spine; when it moves little, this can cause both abrasion of the intervertebral discs and pinching of blood vessels and nerve endings. It is the pinching of the nerves that causes severe pain.
Reasons for the development of pathological processes in the female body
Before considering such manifestations, it is necessary to analyze in detail the causes of the disease. The most likely of them are heredity, age-related body changes, injuries, sudden movements of the spine, circulatory problems, fluid and calcium deficiency. Thoracic osteochondrosis can be a consequence of:
- Stressful conditions;
- Lack of movement (hypodynamia);
- Excess weight;
- Curvatures and other congenital defects of the spinal column;
- Hard work and overload.
Risk level of thoracic osteochondrosis in women
The thoracic type of osteochondrosis most often develops in women. This is due to the onset of menopause and accompanying changes in the body, hormonal imbalance and the likelihood of osteoporosis.
How does the disease manifest itself?
The development of the disease is gradual, so its manifestations are not immediately noticeable. It goes unnoticed, but when it appears, the following signs are noted:
- pain due to osteochondrosis. They are localized in the chest, ribs, probably radiating to the stomach, shoulder or neck. In order not to be confused with pain in the mammary glands, you should remember that the pain with thoracic osteochondrosis will be mild, constant and aching.
- Pressure may increase due to minor stress or for no apparent reason. It can be progressive and cause a hypertensive crisis. Such hypertension can be distinguished by the fact that medications will not give the desired effect.
- Pain in the heart area. They can be distinguished from the real ones by the fact that taking nitroglycerin or other medications that relieve heart pain will not bring visible relief.
- Interruptions in the functioning of internal organs. This especially applies to the stomach and intestines. Signs include heartburn, nausea, increased gas production, pain, and difficulty with bile secretion.
- Breathing problems. Congestion forms in the lungs, which is manifested by dizziness, weakness, pale skin, and shortness of breath.
Treatment of the disease
In order to relieve pain, drugs that relieve spasms, such as Drotaverine and Papaverine, are used. Muscle relaxants are also highly effective. If the disease is advanced, then novocoin blockade will help.
Inflammatory processes and swelling are relieved with non-steroidal drugs. These can be injections, ointments, tablets.
To slow down the destruction of cartilage tissues, chondroprotectors are used.
Treatment of the disease should be continuous and as thorough as possible. If you have any suspicions, you should consult a doctor. To prevent the disease, you need to listen to your body, do not shy away from an active lifestyle and adhere to proper nutrition. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Treatment of lumbar osteochondrosis with therapeutic anti-inflammatory patch NANOPLAST forte
The therapeutic analgesic anti-inflammatory patch NANOPLAST forte has shown high effectiveness in the treatment of many types of osteochondrosis, including lumbar osteochondrosis.
Thanks to the simultaneous influence of two physiotherapeutic factors - deep soft warming heat of infrared radiation and the influence of a magnetic field with specially selected characteristics - this innovative drug allows you to relieve pain and inflammation, improve blood circulation in the affected area, and reduce the dose of painkillers and anti-inflammatory drugs.
Therapeutic pain-relieving anti-inflammatory patch NANOPLAST forte can be used both in the complex treatment of lumbar osteochondrosis and in monotherapy. The patch is applied to the lumbar spine, to the buttocks, depending on the type of disease and location of pain.
To relieve acute symptoms in the treatment of lumbar osteochondrosis, a therapeutic patch is used for 3 to 5 days. The duration of the course of treatment is from 9 days. It is usually recommended to use the treatment patch in the morning for 12 hours, but it can also be used at night.
High efficiency, unique composition, long-term (up to 12 hours!) therapeutic effects, ease of use and affordable price make NANOPLAST forte the drug of choice in the treatment of osteochondrosis of the lumbar spine.
Read more about NANOPLAST forte