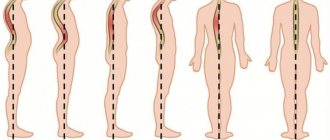
Lumbar kyphosis is one of the types of kyphosis, which is expressed by an atypical curvature of the spine in the lumbar region. This pathology is characterized by damage to the eleventh to twelfth thoracic vertebrae, along with the first and second lumbar vertebrae.
Kyphosis of the lumbar spine is diagnosed in approximately 8% of patients. In adults, this pathology often appears due to spinal injuries and herniated intervertebral discs. Lumbar kyphosis in a child most often appears at the age of 13 years, when the spine grows rapidly and the muscular corset does not keep up with it and does not provide support for the axis of the spinal column in the correct position.
In this article you can see a photo of lumbar kyphosis, as well as learn about the causes of this pathology and methods of its treatment in the multidisciplinary CELT clinic.
What it is
Healthy people have physiologically determined curvatures of the spine - lordosis in the cervical and lumbar regions and kyphosis in the thoracic and sacral regions. Physiological curvature in the thoracic region may increase due to a number of pathological reasons. Progression of the deformity leads to squeezing back of the lumbar vertebrae - inversion .
Brief history of the disease
The most famous hunchbacks are Richard III and the literary Quasimodo. In the old days, hunchbacked people immediately attracted the attention of others. Few individuals survived to adulthood because the pathological processes causing kyphosis were incompatible with life in those days.
They saw something sinister in the hunchbacks, attributing to them a bad character and friendship with mystical forces.
Kyphotic posture has become characteristic of certain segments of the population. It was also called "journeyman's kyphosis." Children forced to “hunch over” their master from an early age - shoemakers, tailors - acquired a characteristic curvature of the spine, affecting the thoracic and lumbar regions.
Peasant children, herders, princes and nobles had straight backs and relatively good health. And the apprentices had neither the time nor the means to take care of themselves.
It was only at the beginning of the 20th century that serious research began to be carried out on the prevention and treatment of kyphosis.
Classification, degrees or what it happens
The term kyphosis is used to refer to the type of curvature of the spine in the longitudinal (sagittal) plane with the apex of the curve dorsal.
Lumbar spinal inversion is assessed by determining the sum of the magnitude of kyphosis and physiological lordosis.
The size of the pathological arc is the basis for the classification of kyphosis according to CJ Kaplan (1952):
| Degree | Complications of kyphosis | Angle of curvature |
| I degree | easy | up to 30° |
| II degree | moderate | 31 — 60° |
| III degree | heavy | more than 60° |
The degree of kyphosis is determined based on measurements of the angle of curvature
Classification of kyphosis based on the etiology of deformities was given by RB Winter in 1995:
- Postural or positional;
- Kyphosis in Scheuermann's disease;
- Congenital with defects in the formation of vertebrae, segmentation;
- Mixed etiology;
- Neuromuscular;
- For spina bifida - late paralytic, detected at birth;
- Traumatic with damage to bone-ligamentous structures without and with damage to the spinal cord;
- Post-surgical;
- Post-radiation;
- For metabolic disorders (osteoporosis, osteomalacia, osteogenesis imperfecta, etc.);
- For skeletal dysplasia (achondroplasia, mucopolysaccharidosis, neurofibromatosis);
- For connective tissue disease (Marie-Strumpel disease);
- Tumor;
- Inflammatory.
Prevalence, significance
The true incidence of pathological kyphosis is unknown. Depending on the diagnostic criteria, it is about 3–8% of the population. Most cases are thoracic kyphosis, which has little clinical significance.
Severe deformation is observed quite rarely. Nowadays, this is a sign of congenital pathology or advanced disease, due to the inaccessibility of medical care for various reasons.
The most common manifestation of spinal deformities is poor posture.
Lumbar kyphosis inversion is most pronounced in the following types of postural disorders:
- Round back with total flat kyphosis , with a caudally displaced apex against the background of the absence of lumbar lordosis;
- Flat-arched back with the absence of physiological thoracic kyphosis against the background of pathological kyphosis of the lumbar region.
Poor posture is the earliest manifestation of spinal diseases that occur with degenerative and dystrophic changes. A flat-arched back disorder is difficult to correct. If such deformities persist for a long time, irreversible changes in the spine may develop.
Severe kyphosis has a negative impact on the functioning of the internal systems of the body and disfigures a person’s appearance.
Video: “What is kyphosis and how to get rid of it?”
Types of disease
Pathological kyphosis is varied. Its type depends on the causes of the disease:
- functional kyphosis or incorrect posture: the cause of the appearance is a weak muscle corset or an unnatural position of the back during prolonged sitting. In some cases, this type of kyphosis is associated with psychology: for example, very tall teenagers try to hide their height and slouch, just as insecure people raise their shoulders to appear more inconspicuous. Trying to compensate for the excessive backward curvature of the spine, the body begins to protrude the lumbar region inward, forward, which causes a concomitant disease - lumbar hyperlordosis.
- dorsal juvenile kyphosis (Scheuermann-Mau disease): presumably, Scheuermann-Mau disease appears as a consequence of necrosis of cartilage tissue (avascular necrosis), excessive growth of bone tissue in the vertebral bodies and multiple vertebral fractures due to osteoporosis. The causes of this type of kyphosis have been little studied, but one thing is certain - genetic predisposition plays a special role here. Scheuermann-Mau disease distorts the shape of the vertebrae, complicating the form of kyphosis. The bending angle can reach up to 75 degrees.
- congenital kyphosis: a disorder appears at the stage of development of the vertebrae in the embryo. The deformation appears as irregularly shaped segments. The curvature can develop in any direction with the apex located in any part of the spine. A disease of this form often progresses, combined with other pathologies and neurotic disorders.
- paralytic kyphosis: appears against the background of diseases associated with weakened or paralyzed back muscles. For example, with cerebral palsy, thoracic kyphosis progresses and increases its length to the lower back, acquiring scoliosis as a concomitant disease.
- post-traumatic kyphosis: fractures of the thoracic or lumbar vertebrae often cause the development of post-traumatic kyphosis. The appearance of the disease is associated with the severity of the injury, the accuracy of following the instructions of the attending physician for the rehabilitation period, and the presence of other diseases associated with disorders of bone or muscle tissue.
- degenerative kyphosis: such kyphosis is a consequence of degenerative changes in the spinal column. Degenerative changes can be either a natural process of aging of the body or a consequence of a slowly developing pathology. Therefore, older people are more likely to be affected by this type of kyphosis.
Risk factors, causes and consequences
There are four physiological arches of the spine. In a newborn child, the spine is an arch with its convexity facing backwards.
Total kyphosis is physiological for newborns and children up to 3 months.
Physiological curvatures of the spine appear as the child develops : in the process of holding the head, cervical lordosis is formed; with the beginning of standing and walking - lumbar and thoracic curvature.
Posture is fully formed only with the onset of puberty.
Pathological changes in the musculoskeletal system during this period can cause changes in the structure of the spine.
Against the background of changes caused by internal causes - genetic, metabolic, infectious, risk factors :
- Underdeveloped muscular system;
- Injuries;
- Lack of physical fitness;
- Uncomfortable furniture;
- Visual defects.
| Causes of acquired kyphosis localized in the lumbar region: | Congenital causes of lumbar kyphosis: |
|
|
Increased thoracic kyphosis results from increased lumbar lordosis. Most often, kyphosis affects the thoracic spine. But in the presence of only lower lumbar lordosis, compensatory kyphosis of the upper lumbar region is observed.
Consequences of kyphotic deformities:
- Psychological problems due to external unattractiveness;
- Development of a stable pain syndrome;
- Spastic paralysis.
Diagnosis of kyphosis
To prevent complications that can lead to disability, it is important to consult a doctor in a timely manner. Particular attention should be paid to the health of children and adolescents, because the sooner treatment begins, the fewer consequences the disease will cause for the body.
To diagnose lumbar kyphosis, the doctor needs to conduct a comprehensive examination. It will include not only a visual examination, but also magnetic resonance imaging, radiography and computed tomography. These measures are necessary in order to determine concomitant pathologies of the spine.
Symptoms and diagnostic methods
Diagnosis includes anamnesis, physical and instrumental examination. Vertebrologists use spondylometry to determine the condition of the spine.
The mobility of the lumbar spine in the sagittal plane is measured in a standing position by measuring the distance between the spinous processes of the TXII – LV vertebrae. This distance increases by 6–8 cm (Schober test) when tilted. According to X-ray data, the mobility of the lumbar spine in the anteroposterior direction is 40°.
At the apex of the deformity, spinal torsion is assessed. The patient stands on straight legs with the torso tilted forward (Adams test). The height of the hump and the angle of torsion are determined at the level of the greatest asymmetry of the paravertebral muscles or ribs (Schultes method).
X-ray examination of the spine is carried out in two projections : lying on the back and on the side.
To assess kyphotic deformity on a radiograph, three indicators are used::
- Cobb angle . The lines forming the angle are drawn along the discs adjacent to the neutral vertebrae (in children) or along the endplates of the neutral vertebrae closest to the apex of kyphosis.
- The ventral angle is formed at the intersection of lines tangent to the anterior surface of the vertebral bodies, drawn along the cranial and caudal knees of kyphosis;
- The dorsal angle is formed at the intersection of tangents drawn along the apices of the spinous processes of the upper and lower knees of the kyphosis.
When researching, age-related features of the structure of the spine are taken into account.
The most common pathologies, the manifestation of which may be lumbar kyphosis, are rare in the population.
Pott's disease
Tuberculous spondylitis can cause kyphosis in the lumbar spine
Tuberculous spondylitis (Pott's disease) is characterized by local soreness, dull pain in the back. Kyphosis of the spine manifests itself in the form of an acute-angled hump against the background of deformation of the ribs at its level. This contributes to respiratory and cardiac dysfunction.
When kyphosis appears, the primary focus of tuberculosis is usually detected in acute or latent form . There is no history of tuberculosis. An interesting connection mentioned in the medical literature is the connection between pathology and the abuse of intravenous drugs.
Pott's disease is characterized by the "reins" symptom, or Kornev's symptom. This is the contouring of muscle cords, tension of the longitudinal muscles in response to flexion of the spine, to tapping along the spinous processes. The symptom is an early sign of damage to the vertebrae.
Another Angelescu symptom characteristic of this pathology is fixation of the spine in the area of the lesion . The patient rests on the bed with the back of his head and heels. Due to pain in the spine, he cannot bend or bend.
A spondylogram of the body is indicative - the vertebrae are flattened anteriorly, destructured, and their density is significantly reduced. The ligamentous apparatus of the spine may undergo ossification.
Brucellous spondylitis
Spondylitis caused by brucellosis is very similar to Pott's disease . X-ray examination allows to identify the regional focus of destruction. It is most often located in front and on the side of the vertebra. Diffuse osteosclerosis forms around the destructive focus. The affected vertebrae are connected to neighboring vertebrae by coracoid bony projections.
Spondylolisthesis
Kyphosis causes the lumbar vertebra Lv to slip forward and move away from the sacrum. Kyphotic protrusion of the Lј vertebra is accompanied by constant moderate pain – Chirkin’s symptom.
With spondylolisthesis, the vertebra protrudes forward
Causes of spondylolisthesis:
- Spinal malformation;
- “fatigue” and fracture of the arch of the interarticular part;
- Spinal instability syndrome;
- Fracture of articular processes;
- Diseases of the musculoskeletal system - arthrogryposis, Paget's disease.
Video: “What is spondylolisthesis?”
Dreyfus syndrome
Did you know that...
Next fact
Generalized platyspondyly is enchondral dysostosis, which manifests itself in a child when he begins to walk. Kyphosis develops due to weakness of the ligamentous apparatus. He is unable to fix the spine. Accompanied by back pain.
Signs of Dreyfus syndrome:
- Shortened neck and torso with long limbs;
- Muscle wasting;
- Loose joints;
- Muscle extensibility;
A spondylogram shows : an increase in the transverse dimensions of the vertebral bodies; decrease in the height of the vertebral bodies; growth of space between the vertebral bodies; reduction in the size of the pelvic and sacral bones; hip dislocation.
Calvet disease
Osteopathy of the vertebral body, called vertebra plana syndrome (Calvet's disease), occurs in children . Most often in boys 7–14 years old. The lumbar spine is affected in 27.7% of cases.
The spondylogram shows:
- osteoporosis of the central part of the vertebra,
- compaction of the endplates with progression of flattening.
The deformed vertebra is separated from neighboring vertebrae by widened intervertebral discs. Flattening is caused by aseptic necrosis of the spongy substance of the vertebral body, Gaucher disease, lymphogranulomatosis, eosinophilic granuloma.
Symptoms of the disease:
- pain in the spine that occurs sharply during somersaults or jumping;
- fatigue in the back;
- fracture of the spinal body (accompanied by short-term weakness in the legs);
- soreness, protrusion of the spinous process;
- difficulty bending the body and straightening;
- increased ESR;
- eosinophilia.
Achondroplasia
Thoracolumbar kyphosis is a characteristic feature of the most studied form of hereditary dwarfism - achondroplasia. Children with this pathology can be born with a normal body length.
Typical clinical picture:
- large head with hypertrophied brain part and fontanelles,
- prominent forehead,
- flattened bridge of the nose,
- shortened limbs,
- deep skin folds,
- isodactyly,
- laxity of the knee joints,
- short, wide feet,
Kyphosis is fixed and cannot be corrected . It intensifies when the child is dropped off.
Rickets
Rickets is another disease that contributes to the development of kyphosis
Kyphotic changes in the spine are detected at the end of the first year of life . Lumbar invasion is characteristic of a severe stage of the disease. It becomes especially noticeable when the child sits and stands. The spine is aligned in the lying position. The “softened” vertebral body narrows the joint spaces - a rachitic hump is formed (if left untreated).
Rachitic kyphosis develops very quickly when the child gets up early and sits for a long time.
The diagnostic process should be aimed, first of all, at identifying the initial agent leading to the pathology in order to prescribe the correct treatment tactics.
Symptoms of pathology
Patients who experience this disease may experience pain, motor and sensory symptoms. In addition to them, dysfunction in the pelvic area is possible. The specificity of kyphosis is not only the main symptoms, but also periodic pinching of the nerve trunk.
Some of the most common symptoms of lumbar kyphosis include:
- pain in the lower back, which can radiate to the buttocks or legs;
- during compression of the roots, numbness of the limbs and lack of sensitivity may be observed;
- increase or decrease in blood pressure;
- stiffness in movements;
- lack of knee or tendon reflex;
- muscle weakness;
- impaired potency in men due to problems in blood circulation;
- regular urge to urinate, fecal incontinence, which are provoked by high pressure on the internal organs of the pelvis;
- the appearance of a small hump above the lower back;
- intercostal neuralgia.
Due to the presence of pain, the patient takes a forced position: leans forward, lowers his shoulders and brings them together. If you do not treat the disease, then in the future your internal organs will begin to suffer from it.
Treatment
Lumbar invasion is not an independent disease . This is a symptomatic manifestation of the underlying disease.
The optimal approach to therapy requires the interaction of doctors of several specialties - orthopedists, neurologists, geneticists, infectious disease specialists, pulmonologists, ophthalmologists, cardiologists, pediatricians.
There is no etiopathogenetic treatment for physeal dysplasia . Symptomatic therapy aimed at improving the patient’s quality of life is the only possible option.
Orthopedic treatment of children with rickets should be carried out comprehensively. Drug antirachitic therapy should begin as early as possible.
With spondylolisthesis with severe inversion of the lumbosacral region, patients require careful dynamic monitoring. Conservative complex therapy is carried out using spinal traction, corsets, physical therapy, massage, physiotherapy, and immobilization.
The pain syndrome is blocked by analgesics . Plaster casts were replaced by functional corsets: fabric corsets with longitudinal metal spikes, polyethylene or polyvik, leather belts. Fixing corsets are used for a long time - for several years. Surgical treatment is prescribed based on the clinical condition of the patient and the prognosis for further treatment of the disease.
In patients with Pott's disease, even antibiotic therapy alone produces good results . It is performed on an outpatient basis and does not require bed rest. If there is significant deformation of the spine and signs of compression of the spinal cord, surgical intervention is indicated. Additionally, long-term rehabilitation treatment is used using a plaster corset.
Drugs
For rickets, vitamin D3 is prescribed in large doses - from 1000 to 5000 IU per day for 3 months.
Artificial vitamin D analogues:
- Oksidevit,
- Calcitriol,
- 1 – alphacholecalciferol,
- Rockartrol.
Daily doses of metabolites are determined individually, depending on the severity and severity of the process. The complex treatment of rickets includes drugs rich in vitamins and microelements in age-specific dosages.
With spondylolisthesis, acute pain is relieved by blockade of 0.25 - 0.5% novocaine solution . Solutions of B vitamins eliminate and reduce the phenomena of secondary radicular syndrome. Reopirin or Pirabutamol relieves pain and inflammation.
Medicines used to treat tuberculous spondylitis:
- Isoniazid,
- Rifampicin,
- Ethambutamol,
- Streptomycin.
Surgery
Surgery for lumbar kyphosis is dangerous due to the intersection of spinal nerves . This can lead to disruption of the innervation of the lower extremities. Resection of the vertebral bodies is performed using curved Luer-type cutters with an elongated beak. Isolation of wedge-shaped vertebrae and their removal is accompanied by intense bleeding.
They try to postpone surgical intervention for children until they reach 11–12 years of age . The absolute indications for surgery are: confusion of the lumbar vertebrae with severe spinal instability, muscle paresis, severe pain, spinal injury, spinal canal stenosis.
The pathological position of the lumbar spine is reconstructed. Resection of the affected vertebral bodies along with the intervertebral disc is performed. Fusion of the remaining vertebrae is done with a bone autograft. It is prepared from the tibia.
One of the surgical methods for treating kyphosis is spinal resection.
Correction of the pathological position of the torso is carried out intraoperatively or after surgery by sharply bending the limbs together with the pelvis and lifting the upper half of the torso.
After the operation, the patient is placed in a previously prepared plaster bed or on a bed with a shield on the stomach. Typically, on the 15th day after surgery, the patient is placed on his back on a loop - a belt. It is fixed to Balkan frames. Kyphosis reclination and functional treatment are carried out for 4 months.
Exercises, massage
The main goals of using physical therapy methods for all clinical forms of kyphosis:
- Correct or reduce existing deformity (kyphosis reclination);
- Prevent the progression of kyphosis;
- Strengthen the muscles of the back and abdominal wall.
Physical therapy methods include:
- Physiotherapy;
- Massage;
- Passive correction;
- Backstroke.
To avoid stress on the spine, therapeutic exercises for kyphosis of any etiology should be performed lying down or on all fours. Exercises in a standing position are possible when the pain subsides.
It is necessary to strengthen the back muscles - this will help maintain the spine in the desired position. With a round back, the muscles of the back and shoulder girdle are especially strengthened, and the muscles of the chest are relaxed and stretched. The mobility of the thoracic spine is increased with extreme caution.
If you have a flat back, you need to strengthen all muscle groups except the lumbar ones. They need to be stretched. Particular attention should be paid to strengthening the muscles of the back of the thighs and abdomen.
The most complete complex of therapeutic exercises can be found in the literary publication by T. V. Lukyanenko “Healthy Spine, Recipes and Recommendations”
Massage improves tissue nutrition and helps restore muscle functionality. If the back muscles are in a pronounced contracture state, then a relaxing massage is first indicated. Strengthening massage is performed according to indications.
For the abdominal muscles , massage is always strengthening. At the same time, it is necessary to restore the functionality of the gluteal muscles and shin flexor muscles - they are important for holding the body in an upright position. Prescribe 3 courses of 20 massage sessions with a break of one month.
Underwater massage is effective.
Video: “Exercises for the lumbar spine”
Treatment at home or with folk remedies
Spinal kyphosis is a bell about severe pathological processes . It can only be dealt with under the supervision of qualified specialists. Folk remedies proposed in modern fiction are sometimes downright dangerous. Taking herbal baths can to some extent soothe the pain caused by compression of the nerve endings. And the advice in some folk medicine encyclopedias to treat kyphosis in a child due to injury by burying him in sand is simply criminal!
Home therapy must be approved by a physician. These are massages, baths, exercises .
When using treatments at home, you need to take into account the contraindications of some methods. So, for rickets, baths with salt and pine needles, massage cannot be used until the acute phase of the disease subsides. A course of ultraviolet radiation is not indicated at the same time as taking vitamin D.
For spondylolisthesis at home, baths with sea salt (1–2 kg per bath) or pine needles (1–2 tablets of 30 g or 100 ml of liquid extract) effectively relieve pain. Water temperature 36 -38°C. Course 15 – 20 baths with duration – 15 minutes.
Treatment methods for diagnosing kyphosis
They can be different, since it all depends on the degree of kyphosis (there are 4 of them), the pathology accompanying it, as well as the presence of contraindications and other individual characteristics of the patient. All methods can be classified as follows:
- drug treatment;
- physiotherapy;
- physical therapy and gymnastics;
- manual therapy;
- surgical intervention;
- orthopedic treatment.
All of the above methods are prescribed comprehensively and, which is extremely important, on an individual basis.
Prevention and diet
The occurrence of congenital pathologies leading to lumbar kyphosis is difficult to prevent . Their exact etiology is still unknown. But when identifying them in newborns, the main thing is to delay the child’s sitting, crawling, and standing up. In parallel, symptomatic treatment is carried out aimed at replacing the impaired functions of the musculoskeletal system.
Prevention of kyphosis in early childhood is based on proper nutrition with a sufficient amount of calcium in the diet. With rickets, in order to prevent the progression of the disease and the formation of persistent bone deformities, the early rise of the child in the first year of life and the early start of walking are limited.
The child’s nutrition should optimally meet his needs for proteins, fats, carbohydrates, vitamins and microelements.
For a child under 6 months of age, the best food is breast milk, and when bottle-fed, sour milk formulas.
The spine must be treated with extreme care to prevent traumatic injury. Do not lift weights, do not fall, do not make jumps that are dangerous for the entire structure of the spine.
Pathological kyphotic posture is caused by an inferior muscular skeleton. This may be due to congenital reasons or an incorrect lifestyle.
But the worsening of kyphosis can be prevented by simple hygiene measures:
- Physical exercise;
- Nutrition that meets the needs of the musculoskeletal system;
- Organization of the workplace (desk and chair of the required height, adequate lighting);
- The right place to sleep, respecting the physiological curves of the spine.
A diet for diseases of the spine should help restore musculoskeletal tissue. This requires foods rich in vitamin D, calcium, and amino acids. This is liver (poultry, fish, pork, beef), fish, egg, butter.