The meniscus is a formation consisting of cartilage tissue. It is located between the lower leg and thigh and is designed to perform one of the main functions - to protect the articular cartilage. In addition, it supports all parts of the joint that come into contact with each other, and also significantly reduces their friction during movement. Traumatization of the meniscus leads to joint blockade, which is always accompanied by severe pain. Sometimes a “false recovery” occurs, after which a relapse always occurs, so it is impossible to do without competent treatment.
Meniscus injury
As a rule, people who are actively involved in sports or heavy physical labor are susceptible to these injuries. Mostly, meniscus injuries can be found in men aged 18 to 45 years. In children, such injuries practically do not occur, since during this period the anatomical structure of the boy’s body is significantly different from that of an adult man. But in women, this type of injury occurs rarely. There are cases when, under the influence of certain diseases, a meniscus rupture occurs, and this is not due to playing sports. As a rule, this damage can occur due to degenerative changes or inflammatory processes occurring in the knee joint, that is, arthrosis or arthritis.
Anatomy
The knee joint consists of three bones:
- femoral;
- tibial, it is considered the largest;
- patella
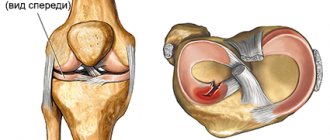
In addition to the above bones, the joint contains menisci - small cartilaginous plastics resembling multifaceted plates in shape. The menisci are located inside the joint, namely between the femur and tibia. They divide the joint into two compartments, which provide motor function of the lower limb.
Anatomy of the knee
There are two menisci in the knee:
- Outer. It is characterized by excessive mobility, therefore, when exposed to external force, the outer meniscus is less susceptible to injury due to its weak connection with the articular capsule, which ensures its excessive mobility.
- Interior. Its injuries are quite common. On the one hand, it is connected to the tibia, and on the other, to the outer edge of the joint capsule.
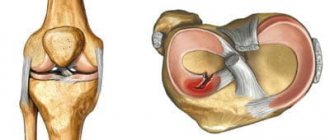
In medical practice, the following types of injuries occur: separation of the meniscus from the place where it should be attached, meniscal rupture, excessive mobility of the meniscus, which is typical for ligament damage.
Causes
The most common cause of meniscal damage is injury to the knee. Damage to the meniscus can be combined with other injuries or be isolated from them. Almost every second patient who suffers a knee injury is diagnosed with a fracture of the tibia along with damage to the meniscus. In addition, people with a history of cruciate ligament ruptures are at risk, since with the slightest external impact on the joint, a meniscus rupture occurs. In medical practice, two types of bruises are distinguished; let’s look at them in more detail.
Physical
It occurs due to the influence of external force on the joint. Injuries occur in these situations:
- rotational movements are made in the area of the knee joint;
- the patient leans excessively on his knee;
- the knee joint is excessively bent;
- accelerated knee extension.
Professional athletes experience constant knee injuries, and this leads to chronic inflammation of the meniscus. As a result, any injury, even a small one, can lead to a meniscus tear.
Degenerative
Degenerative damage often occurs in people who have passed the age of forty and suffer from certain diseases. Rheumatism. It causes not only damage to the heart muscle, but also leads to damage to large joints. Rheumatism causes swelling of the tissues located near the joint, and they, in turn, disrupt the blood supply to the meniscus. The meniscus fibers become less strong, they lose elasticity and resilience, which makes them prone to various damages.
Degenerative meniscus tear
Gout. This disease refers to metabolic disorders. Excess uric acid remains in the body and settles in the muscle tissue and joints. Crystalline substances of uric acid, entering the joint, begin an inflammatory process, accompanied by severe pain. Sometimes uric acid can cause a decrease in the strength of the meniscus, which ultimately leads to injury.
Risk factors
The main risk factors for developing Osgood-Schlatter disease are age, gender and participation in sports.
Age
Osgood-Schlatter disease occurs during puberty and growth of the body. The age range is different for boys and girls because maturation begins earlier in girls. Osgood-Schlatter disease usually develops in boys aged 13-14 years and in girls aged 11-12 years. Age ranges differ by sex because girls experience puberty earlier than boys.
Floor
Osgood-Schlatter disease is more common in boys, but the gender gap is closing as more girls gradually take up sports.
Sports activities
Osgood-Schlatter disease occurs in nearly 20 percent of adolescents who participate in sports, while it occurs in only 5 percent of adolescents who do not participate in sports. The disease occurs mainly when playing sports that require a lot of jumping and changing the trajectory of movement. This is for example:
- Football
- Basketball
- Volleyball
- Gymnastics
- Figure skating
- Ballet
Symptoms
At the initial stage of meniscal injury, the following symptoms may appear:
- unpleasant discomfort in the knee area;
- pain of moderate or low intensity;
- inflammation in the knee area.
After receiving an injury, the patient immediately experiences pain, and swelling becomes noticeable in the knee area. Pain can be observed at the site of the meniscal injury or throughout the joint opening. Damaged parts of the meniscus can cause discomfort when the victim moves. With a minor injury to the meniscus, there may be no pain, but when the joint moves, strong clicks or crunching sounds will be heard, but with severe damage, complete dysfunction of the joint is possible.
Severity of meniscus injury
Before prescribing a course of treatment, the doctor must determine the severity of the injury. This is due to the fact that minor injuries do not require hospitalization or surgery. There are three degrees of severity of rupture:
- The pain is moderate, swelling is not obvious.
- The pain is severe, but its severity dulls over time, swelling is pronounced, and a hematoma is present.
- Acute pain, extensive swelling, hematoma, impossible to step on the affected leg.
Regardless of the extent of the rupture, the affected joint must be shown to a doctor. This is because improper healing of cartilage tissue can reduce the functionality of the knee joint and lead to lameness.
Diagnostics
To confirm the initial diagnosis, the specialist conducts a number of additional tests. Baykov's symptom. The knee bends at an angle of 90 degrees. Then the specialist performs the following manipulation: palpates the joint gap and extends the lower limb. If during the diagnostic process the patient experiences sharp pain, it means that there is trauma to the meniscus.
Baikov's symptom test
Shteiman's sign. The joint is bent at an angle of 90 degrees, and then circular movements are made with the knee. If the patient feels severe pain when rotating inward, it means that the internal meniscus has been injured, and when rotating outward, the external meniscus has been injured. Laidau's symptom. With this type of diagnostic examination, the patient is asked to sit in a “Turkish” position if he feels acute pain in the knee - the meniscus is damaged. Chaklin's symptom. This type of diagnosis helps to identify tears of the internal meniscus. The essence of the test is to perform flexion and extension movements; the appearance of a crunch means the presence of damage; Polyakov's symptom. The test is performed while lying on your back. The patient lifts up the limb that has not been injured, lifts himself onto his shoulder blades and rests on the heel of the sore leg. The presence of severe pain indicates a meniscal injury. McMurray's sign. The victim is placed on his back, he bends his legs and makes circular movements with the limb; the presence of pain in the joint will allow a diagnosis of a meniscal injury to be made.
General
The initial diagnosis is made based on the patient's complaints, as well as tests performed. However, to determine the severity of the meniscus lesion, an instrumental examination is prescribed.
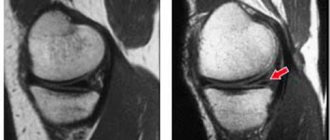
Crack in the meniscus
Conventional radiography is considered irrelevant today, since it is almost impossible to see the meniscus in the images, so more modern research techniques are used.
- Ultrasound. For proper visualization of the damaged area, the patient is placed in a supine position with knees bent. Before an ultrasound examination, the patient should not receive intra-articular injections for several days.
- A CT scan is prescribed when it is necessary to determine the nature of injury not only to the meniscus, but also to the entire knee. Otherwise, this diagnosis is considered meaningless, since with this device it is problematic to determine the degree of damage to the meniscus, as well as ligaments and muscle tissue.
- MRI is an excellent determinant of meniscal lesions.
Which specialist treats a meniscus injury?
A traumatologist treats problems of the musculoskeletal system. But due to the fact that unpleasant symptoms can develop several days after the fall that led to the rupture, not everyone thinks to visit the emergency room. As a last resort, it would not be a mistake to contact a therapist - after an examination, he will determine the problem and give the necessary direction. If there is no clinic with specialized specialists in the city, you will need to visit a surgeon. He will conduct an examination and, if necessary, provide treatment.
Treatment
If you suspect a meniscus lesion, you should immediately immobilize the patient, apply a cold compress to the injury site, and then call an ambulance. Treatment is prescribed by a specialist based on a diagnostic study.
Conservative
As a conservative technique, the following are prescribed:
- Non-steroidal painkillers: Ibuprofen, Voltaren, Indomethacin, Diclofenac.
- Chondroprotectors are aimed at the regeneration of cartilage tissue.
- Ointments that relieve inflammation and severe pain.
Meniscectomy
If the patient has a crushed or displaced meniscus, blood in the periarticular cavity, or there is no successful response to another treatment method, a meniscectomy is prescribed.
Meniscectomy
Meniscopathy is amputation of the meniscus; it is used for the decomposition of cartilage tissue or for acute inflammatory processes that cannot be eliminated. However, this extreme measure is resorted to only in the most difficult situations; in other cases, doctors try to save the meniscus.
Regeneration
Surgeons can restore the meniscus in several cases:
- the meniscus has torn away from the joint capsule;
- the meniscus tear has a perpendicular direction;
- no degeneration is observed in the cartilage;
- the patient is at a young age.
Arthroscopy
Today, arthroscopy is considered the most effective treatment method. Using a special arthroscope, the location of the meniscal lesion is determined, and then the damage is repaired. This technique is used for rupture of the meniscus, as well as its anterior horn.
Transfer
Transplant operations are performed in cases of absolute fragmentation of the meniscus, leading to limb dysfunction and persistent acute pain in the patient. However, this technique has contraindications:
- joint instability;
- changes in the knee area;
- elderly age of the patient;
- diabetes;
- diseases of the gastrointestinal tract.
Prevention
As a preventative measure, it is recommended to wear a knee pad on the lower limb while playing sports.
Also, do not neglect warming up the muscles before performing physical exercises; you should strengthen muscle tissue more thoroughly, and also take medications that affect peripheral blood supply. An injury such as a torn meniscus is quite common. If measures aimed at treatment are not taken in a timely manner, they can ruin the life of any person, and sometimes lead to disability, therefore, at the slightest injury, you should seek qualified help. Share:
Rehabilitation
The period of rehabilitation after injury is of no small importance. It includes :
- Performing special exercises to develop the knee joint.
- The use of chondoprotectors and non-steroidal anti-inflammatory drugs.
- Massage, physiotherapy.
- No loads throughout the year.
Rehabilitation after such an injury includes five stages:
- Stage 1 – its duration is 4-8 weeks. At this stage, you need to try to maximize the range of motion in the injured joint and reduce swelling.
- Stage 2 – lasts about 2.5 months. It is necessary to completely restore motor activity, eliminate swelling, and begin to train weakened muscles.
- Stage 3 – it is necessary to completely restore motor activity when playing sports, to restore muscle strength. At this stage, they actively engage in physical therapy and return to normal life.
- Stage 4 – it is necessary to achieve the ability to actively engage in sports without pain, as well as to increase the strength of the muscles of the injured leg.
- Stage 5 – all functions of the joint should be restored.