A meniscus cyst is a formation filled with synovial fluid, which normally nourishes the joint cavities. These formations can be located in the thickness of the cartilage, and in advanced stages they extend beyond its limits, forming parameniscal cysts.
As in the case of a Baker's cyst or hygroma, increased stress or injury to the knee leads to cystic degeneration, in this case of the cartilaginous plates.
Menisci are triangular cartilaginous plates bent at the edges with thickened peripheral edges. Their shape compensates for the discrepancy between the articular surfaces of the bones. They act as shock absorbers, reducing trauma from shocks when walking. They also stabilize the knee joint, eliminating excessive movements.
In simple terms, it is a fibrocartilaginous disc, a cushion that helps the bones of the joint fit together, helping to stabilize the joint.
Main reasons
Meniscal cysts occur under long-term stress due to exposure to prolonged tangential and compressive forces. Mucoid synovial fluid accumulates, stretches the meniscus tissue, and then transforms into a fluid cavity. A number of reasons for the appearance of meniscal cysts:
- hereditary predisposition;
- congenital pathologies and dysplasia;
- excessive physical activity;
- sports and household knee injuries;
- joint diseases - arthritis, arthrosis;
- lymphatic pathologies.
The risk group includes working people whose profession involves stress on their knees, as well as professional athletes (football players, dancers, hockey).
Menisci of the knee joint
are cartilage pads that act as shock absorbers in the joint, as well as stabilize the knee joint and increase the congruence of the articular surfaces in the knee joint. When moving in the knee joint, the menisci are compressed and their shape changes. There are two menisci in the knee joint - external (lateral) and internal (medial). In front of the joint they are connected by a transverse ligament. The external meniscus is more mobile than the internal one, so traumatic injuries occur less frequently. The internal meniscus is less mobile and is connected to the internal collateral ligament of the knee joint, so the injury is often combined with damage to this ligament. Lateral to the joint, the menisci are fused to the joint capsule and have a blood supply from the arteries of the capsule. The internal parts are located deep in the joint and do not have their own blood supply, and their tissues are nourished by the circulation of intra-articular fluid. Therefore, damage to the meniscus near the joint capsule heals well, but tears in the inner part, deep in the knee joint, do not heal at all. Prevalence of meniscus injuries Among internal injuries of the knee joint, meniscus injuries occupy the first place. According to the CITO Sports and Ballet Injury Clinic, where mainly athletes, in whom this injury occurs most often, are treated, meniscal injuries account for 60.4% of 3019 people, of which 75% are patients with injuries to the internal meniscus, 21% with injuries and diseases of the external meniscus and 4% - with damage to both menisci. The proportion of meniscus damage is correspondingly 4:1. This is due to the patient population and improved diagnostics (arthroscopy and other methods). Thus, the menisci are most often damaged in athletes and physical workers aged 18 to 40 years. In children under 14 years of age, meniscus rupture occurs relatively rarely due to anatomical and physiological characteristics. Damage to the menisci is more common in men than in women - in a ratio of 3:2, the right and left are affected equally.
Causes of meniscus injuries
The cause of a meniscus tear is an indirect or combined injury, accompanied by rotation of the tibia outward (for the medial meniscus), inward (for the external meniscus). In addition, damage to the menisci is possible with sudden excessive extension of the joint from a bent position, abduction and adduction of the lower leg, and less often when exposed to direct trauma (hitting the joint on the edge of a step or being hit by some moving object). Repeated direct trauma (bruises) can lead to chronic trauma to the menisci (meniscopathy) and subsequently to its rupture (after squatting or a sharp turn). Degenerative changes in the meniscus can develop as a result of chronic microtrauma, after rheumatism, gout, chronic intoxication, especially if the latter are present in people who have to walk a lot or work while standing. With a combined mechanism of injury, in addition to the menisci, the capsule, ligamentous apparatus, fat body, cartilage and other internal components of the joint are usually damaged.
Types of meniscus damage
The following types of meniscal injury are distinguished: 1 separation of the meniscus from its attachment sites in the area of the posterior and anterior horns and the body of the meniscus in the paracapsular zone; 2 ruptures of the posterior and anterior horns and the body of the meniscus in the transchondral zone; 3 different combinations of the listed damages; 4 excessive mobility of the menisci (rupture of the intermeniscal ligaments, meniscal degeneration); 5 chronic trauma and degeneration of the menisci (meniscopathy of a post-traumatic and static nature - varus or valgus knee [see varus and valgus]); cystic degeneration of the menisci (mainly external).
Nature of meniscus damage
Meniscal tears can be complete, incomplete, longitudinal (“watering can handle”), transverse, flap-like, or fragmented. More often, the body of the meniscus is damaged with the transition of the damage to the posterior or anterior horn (“handle of the watering can”), isolated damage to the posterior horn is less common (25-30%), and even less often the anterior horn is injured (9%). Tears can be with or without displacement of the torn part. Tears of the medial meniscus are often combined with damage to the lateral capsuloligamentous apparatus. With repeated blockades with displacement of the torn part of the meniscus, the anterior cruciate ligament and the cartilage of the internal femoral condyle are injured (chondromalacia).
Symptoms of meniscal damage In the clinical picture of meniscus damage, acute and chronic periods are distinguished. Diagnosis of meniscus injuries in the acute period is difficult due to the presence of symptoms of reactive nonspecific inflammation, which also occur with other internal injuries of the joint. Characterized by local pain along the joint space corresponding to the area of damage (body, anterior, posterior horn), severe limitation of movements, especially extension, the presence of hemarthrosis or effusion. With a single injury, bruises, tears, pinching, and even crushing of the meniscus often occur without tearing it off or separating it from the capsule. Predisposing factors for complete rupture of a previously undamaged meniscus are degenerative phenomena and inflammatory processes in it. With proper conservative treatment of such damage, complete recovery can be achieved. After the reactive phenomena subside (after 2-3 weeks - the subacute period), the true picture of the damage is revealed, which is characterized by a number of typical clinical symptoms in the presence of an appropriate history and mechanism of injury: local pain and infiltration of the capsule at the level of the joint space, often effusion and joint blockade. Various characteristic pain tests confirm the damage. The number of these tests is large. The most informative of them are the following: extension symptoms (Roche, Baykova, Landau, etc.); rotational (Shteiman - Bragarda); compression symptoms and mediolateral test.
Diagnosis of meniscus injuries
The so-called voiced tests, i.e., symptoms of sliding and movement of the menisci and clicking during passive movements, are also of great importance in the diagnosis of meniscal injuries. The most typical and easiest to recognize a medial meniscus tear is a true joint block (a “watering can handle” meniscus tear). In this case, the joint is fixed at an angle of 150-170°, depending on the size of the displaced part of the meniscus. True blockade of the meniscus must be differentiated from reflex muscle contracture, which often occurs with bruises, damage to the capsular-ligamentous apparatus and entrapment of intra-articular bodies (chondromalacia, chondromatosis, Koenig's disease, Hoffa's disease, etc.). We must not forget about the possibility of pinching the hypertrophied pterygoid fold. Unlike blockade of the joint by the meniscus, these infringements are short-term, easily eliminated, harmless, but are often accompanied by effusions. In case of damage to the outer meniscus, joint blockades occur much less frequently, since the meniscus, due to its mobility, is more often subject to compression than to tearing. In this case, the meniscus is crushed by the articular condyles, which with repeated injuries leads to degeneration and often cystic degeneration. Discoid menisci are especially often cystic. The most characteristic symptoms of damage to the external meniscus are local pain in the outer part of the joint space, aggravated by internal rotation of the leg, swelling and infiltration in this area; a symptom of a click or roll and, less often, a symptom of blockade. Many of the listed symptoms of meniscal damage also occur with other injuries and diseases of the knee joint, so timely recognition of a meniscal tear in some cases presents significant difficulties. A carefully collected anamnesis is the main diagnostic criterion. Pain tests, as a rule, are not detected, there is no irritation of the synovium. There is only a positive Chaklin's symptom (tailor's test), sometimes a sound phenomenon (clicking, rolling, friction). A survey radiograph reveals a narrowing of the corresponding parts of the joint space with symptoms of deforming arthrosis. In such cases, paraclinical methods help. Great difficulties are encountered with atypical forms of the meniscus (discoid or continuous meniscus), with chronic trauma (meniscopathy), rupture of the ligamentous apparatus of the meniscus (hypermobile meniscus), and damage to both menisci. A discoid, predominantly external, meniscus is characterized by a rolling symptom (clicking knee). Due to its massiveness, it is more often subject to crushing by articular surfaces, which leads to degeneration or cystic degeneration. There are three degrees of cystic degeneration of the external meniscus (according to I. R. Voronovich). Grade I is characterized by cystic degeneration of meniscus tissue (cysts are detected only histologically). Clinically, moderate pain and infiltration of the capsule are determined. In grade II, cystic changes spread to the meniscus tissue and the pericapsular zone. Clinically, in addition to the indicated symptoms, a small painless protrusion is detected in the anteromedial part of the external joint space, which decreases or disappears when the knee joint is extended (due to movement of the meniscus deep into the joint). In grade III, the cyst involves parameniscal tissue; mucous degeneration occurs with the formation of cystic cavities not only in the meniscus tissue, but also in the surrounding capsule and ligaments. The tumor-like formation reaches a significant size and does not disappear when the joint is extended. Diagnosis of degrees II and III is not difficult. Chronic microtrauma of the menisci is characterized by poor anamnestic and clinical data. With meniscopathy, there is usually no significant history of trauma; pain along the joint space, synovitis, and atrophy of the inner head of the quadriceps femoris muscle periodically appear. Meniscopathy also develops when there is a static disorder (valgus, varus knee, flat feet, etc.). Arthroscopy makes it possible to detect degenerative changes: the meniscus, as a rule, is thinned, lacks shine, has a yellow tint with the presence of cracks and tissue disintegration in the area of the free edge; easily torn, excessively mobile. Histological examination using electron microscopy with a scanning device reveals significant cracks and erosions of the surface layer, and in some places, areas of destruction in deep layers. Symptomatology for damage to both menisci consists of the sum of the symptoms inherent in each of them. Simultaneous damage to both menisci is rare. A predisposing factor is rupture of the intermeniscal ligament, which leads to pathological mobility of the menisci and contributes to their damage. Diagnosis of a rupture of both menisci is difficult, since the clinical picture of damage to the internal meniscus usually predominates. Errors in recognizing meniscal injuries are 10-21%.
Treatment of meniscus injuries
depends on the severity of the condition. At one extreme, small tears or degenerative changes in the meniscus should be initially treated conservatively. At the opposite extreme, a large, painful watering can-handle tear causes blockage of the knee joint and requires immediate arthroscopic surgery. Most actual meniscus injuries fall somewhere between these two extremes and the resulting treatment decisions. Therefore, the decision for immediate surgery should be made based on the severity of symptoms and signs, while taking into account the athletic level and workload of the athlete.
Patients whose condition does not improve with conservative treatment require surgery. The purpose of the operation is to preserve the body of the meniscus as much as possible. Some meniscal lesions are suitable for fusion by surgical suture, which can be performed arthroscopy. The decision as to whether to attempt repair of a tear is based on several factors, including the recency of the injury, the age of the patient, the stability of the knee, the location of the tear, and its orientation. The outer third of the meniscus rim has a blood supply, and a tear in this area can heal. A tear with an increased chance of successful healing is a fresh longitudinal tear in the peripheral third of the meniscus in a young patient with simultaneous anterior cruciate ligament reconstruction. Degenerative processes, displaced tears, horizontal dissections, and complex lesions are poor candidates for healing. Young patients have a greater likelihood of success. Displaced tears may require removal of the torn portion of the meniscus (meniscectomy). Meniscus surgery in modern clinics is done by arthroscopy, which is performed through several small surgical holes and takes approximately 1-2 hours. Through these holes, the surgeon inserts surgical instruments into the joint cavity, including a small video camera that allows you to see the joint from the inside.
Conservative treatment
usually prescribed for small tears of the posterior horn of the meniscus. Stable vertical tears, which are most often observed along the periphery of the menisci, also respond well to conservative treatment. These tears may be accompanied by pain, but do not impinge on the meniscus between the articular surfaces and do not cause any clicking or rolling sensations. Conservative treatment is effective when the knee joint is stable and symptoms are mild. Small (less than 10 mm) stable longitudinal tears, tears of the upper or lower surface that do not penetrate the entire thickness of the meniscus, as well as small (less than 3 mm) transverse tears may heal on their own or do not appear at all. However, it is necessary to exclude activities in sports that require a quick jerk from the defender and movements in which one leg remains in place - they can worsen the condition. If a minor tear is suspected, conservative treatment may include exercises to restore normal additional types of knee motion and the use of orthoses for 2-3 weeks. Shortly after injury to the meniscus of the knee, atrophy of the quadriceps femoris muscle often develops. Therefore, during this period, the affected athlete should perform isometric exercises, stretching and strengthening of the quadriceps and hamstrings. Standard measures of conservative treatment: To reduce swelling that occurs in a horizontal position of the body, it is necessary to raise the leg above the level of the heart. To prevent swelling and hemorrhage into the joint cavity, it is necessary to wear an elastic compression bandage. It is necessary to apply a cold compress (crushed ice in a plastic bag) to the injured area several times a day. Do not apply ice directly to the skin. Avoid physical activity that caused the meniscus injury. Your doctor may recommend the use of crutches, which will reduce the stress on the injured limb. Nonsteroidal anti-inflammatory drugs, such as ibuprofen and aspirin tablets or ointments, can help relieve pain and swelling. After this initial phase, more complex types of conservative therapy are prescribed. Young athletes can initially only be treated conservatively. Among the adult population, surgical treatment of meniscal tears is more common. Indications for arthroscopic surgery include pain and effusion that cannot be treated conservatively, as well as friction during movement or joint blockage. If there is a suspicion of damage to the cruciate and collateral ligaments of the knee joint, then you should not immediately refer the patient for surgery. It is recommended that special attention be given to reducing the severity of swelling to ensure that the knee joint can be tested for a more accurate diagnosis. We must always keep in mind that a decrease in the severity of symptoms of meniscus damage does not indicate the therapeutic effect of conservative treatment and does not guarantee the prevention of new damage to articular cartilage in the future. The choice of treatment for meniscus tears will depend on the athlete's response to the conservative treatment performed.
Surgery
The volume and technique of surgical intervention are determined by the severity and location of the injury. In athletes (and in young people in general), it is not recommended to use arthrotomy - an open operation with opening of the joint cavity - due to the high risk of complications and the long duration of the recovery period. Preference should be given to a minimally invasive operation - arthroscopy - with the introduction of an arthroscope through a small puncture and the implementation of all manipulations through it. In addition, with arthroscopy it is possible to assess in detail the nature of the damage. The disadvantage of arthroscopy is its higher cost, as well as the need for equipment and surgeons with appropriate qualifications. Displacement or infringement of the meniscus If the meniscus is displaced or infringed, a puncture of the knee joint is performed to remove blood, and the meniscus itself is straightened during a closed operation by performing sequential bending of the leg at the knee at a right angle and traction of the shin with simultaneous rotation and abduction to the healthy side. As a result, the articular surfaces diverge slightly and the meniscus snaps back into place. Then the limb is immobilized with a plaster splint for 1–2 weeks, after which rehabilitation measures begin. In case of “blockade” of the knee joint (feeling of elastic resistance when trying to bend or straighten the leg at the knee), “closed” methods of reduction are not used, since turning the leg and flexion-extension in the joint during closed reduction against the background of the blockade can lead to additional injury pinched meniscus and cartilaginous surface of the joint. However, true blockade of the meniscus must be distinguished from reflex muscle tension, which often occurs with bruises, damage to the capsular-ligamentous apparatus and pinching of intra-articular bodies (chondromalacia, chondromatosis, Koenig's disease, Hoffa's disease, etc.). We must not forget about the possibility of pinching the hypertrophied pterygoid fold. Unlike blockade of the joint by the meniscus, these infringements are short-term, easily eliminated, harmless, but are often accompanied by effusions.
Postoperative rehabilitation
Rehabilitation begins in the hospital, with physiotherapy and exercise therapy. On days 2–3 after surgery (provided there is no hemarthrosis or other complications), isometric exercises begin. For a week after surgery, walking is allowed only with a cane or crutches. If a torn meniscus has been repaired, crutches must be used for much longer (4-6 weeks) and no stress must be placed on the injured knee to allow the meniscus to heal completely. In the future, the list of exercises is expanded, gradually increasing their complexity and the degree of load on the joint: from 7–10 days, exercises in the pool and exercises in the knee joint without load on the leg (from a sitting or lying position) are recommended. From 15–20 days, walking is allowed with support on the operated leg; half squats and special exercises on a bicycle ergometer and exercise machines are required to prevent the formation of contractures. After 4-6 weeks, and maybe even earlier, the patient will be able to return to normal physical activity. After restoration of joint function, they move on to sports rehabilitation - gradual implementation of preparatory exercises and return to sports. With partial meniscectomy, as well as after complete meniscectomy with subsequent installation of a modern implant, the rehabilitation time is significantly reduced - full load on the joint (walking) is possible from 5-7 days.
How does a parameniscal cyst form?
Formations lying closer to the median plane are medial , medialis, and those located further are lateral , lateralis.
What a parameniscal cyst is is a membrane with mucoid fluid located not in the thickness of the meniscus, but on its periphery (that is, on the outside). This is due to the fact that it is easier for the mucoid substance to spread in the peripheral direction, along a vector from an area of high pressure to an area of low pressure (outward). This pathology has variable dimensions, does not visually disappear when the knee is extended, and does not change its shape or size.
The prefix para means being nearby, characterizes its location near the ligaments, near the joint capsule.
Synovial cyst of the knee joint
A synovial cyst is a disease characterized by hernia or hypertrophy (enlargement) of the synovial membrane of a joint. Today, medicine is not able to name the exact cause of this disease, but there are several risk factors, such as osteoarthritis, rheumatoid arthritis, and traumatic joint injuries. Treatment of this knee cyst in most cases is surgical, since conservative treatment methods are not highly effective. The operation consists of complete removal of the synovial cyst and subsequent suturing of the weak point of the capsule with a special suture, which helps to strengthen it. Today, a popular method is endoscopic removal of the knee cyst, because this method is less traumatic and the recovery period is faster and more effective. But in any case, you should not delay your visit to the doctor, since the synovial cyst may rupture and this, in turn, will greatly complicate the entire process of treatment and recovery.
Types of meniscal cysts
Based on location, intrameniscal and parameniscal cysts are distinguished. Intrameniscal – located in the thickness of the cartilage, and even minor physical activity can increase the likelihood of a meniscus tear. Parameniscal cyst - develops from an intrameniscal cyst. And when connective tissue grows around a liquid formation, its apparent size may increase.
There are other cystic lesions of the knee that do not affect the structure of the menisci:
- synovial cyst - a cystic change in the membrane of the synovium;
- Baker's cyst - diagnosed in the popliteal fossa, characterized by inflammation of the synovial bursae between the tendons of the leg and thigh muscles: the medial head of the gastrocnemius muscle and the distal part of the semimembranosus;
- a subchondral cyst occurs when there is a cyst in the hip joint, is small in size and occurs in people aged 60-75 years;
- ganglion cyst - is rare, also appears in vertebral cysts, filled with viscous, colorless liquid contents, develops due to a defect in the joint capsule, tendon sheath and outward protrusion of tissue.
In addition, lateral and medial meniscal cysts are distinguished, and formations in the medial meniscus are diagnosed 3 times less often due to the deeper location of the cartilage, while the lateral one is more susceptible to stress.
Other types of cystic formations of the knee
On the back surface of the knee joint, when the joint capsule is weak and the synovial bursa is damaged, a Baker's cyst is formed. The subchondral cyst consists of fibrous tissue and is filled with myxoid contents. This formation most often does not cause symptoms. Another type of neoplasm is a ganglion cyst of the knee joint. It is a compaction in which synovial fluid accumulates. The ganglion often forms in the tissues of the cruciate ligament; the formation can be multilocular.
Differences between a lateral cyst and a medial one
If the internal meniscus is damaged, a medial meniscal cyst is determined, if the external meniscus is damaged, a lateral one is determined. With cystic damage to the lateral meniscus, walking is difficult due to pain, as is the case when putting a load on the knee. Local swelling is noted along the anterolateral surface of the knee, anterior to the lateral collateral ligament.
When the joint is flexed by 140-150 degrees, it appears visually; upon palpation examination, a dense, painful formation is revealed. The pathology of the medial meniscus is less pronounced due to its resistance to trauma, and therefore manifests itself as swelling at the level of the joint space, posterior to the medial collateral ligament. It is distinctive that it is more difficult to visually determine a cystic lesion of the internal meniscus due to its deep location.
Features and functions of the lateral meniscus
Menisci are cartilage pads that are located between the articular surfaces of the thigh and lower leg. They are divided into external (lateral) and internal (medial). The main functions are to maintain the normal interaction of all components of the joint, to act as shock absorbers, that is, to soften shocks during movement (walking, running, jumping). They are responsible for uniform load distribution, distribute joint fluid, and limit the range of motion within the physiological norm.
In contrast to rupture of the medial cartilaginous plate, damage or rupture of the lateral one is much less common. As a rule, this is not the only problem of the knee joint. Damage to these cartilage plates usually accompanies a more severe knee injury that impairs its functionality. Both the external and internal are cartilaginous formations, which have an anterior, posterior horn and a central part.
The lateral meniscus is not so tightly attached to the joint capsule, unlike the medial meniscus, which explains its greater ability to withstand non-physiological loads. This explains its rarer isolated lesion. The lateral plate is more rounded, functionally it is as important as the medial one - to increase the area of contact of the articular surfaces of the femur and tibia, to stabilize the joint.
Its peculiarity is that it has an incomplete attachment - the tendon of the popliteus muscle passes through the body. In some people, the meniscus does not have the usual round shape, and looks like a fibrocartilaginous plate that completely or partially covers the lateral condyle of the tibia. In this case it is called discoid. This is not considered a pathology, but simply one of the normal variants. This form does not have a negative impact on the functionality of the joint. As a rule, a person learns about a discoid meniscus by chance when examining the joint for any problems in the knee.
Symptoms and stages of pathology
Cystic processes in the menisci are accompanied by pain in the area of the joint space (between the articular surfaces of the tibia and femur, inside the knee). When walking, doing physical exercises and any movements, it intensifies, and in an immobilized state it subsides. There may be loss of sensation around the knee and swelling in the knee joint. Upon examination, the traumatologist reveals a dense swelling on the lateral side of the joint; pressure is accompanied by increased pain.
With the development of cystic changes in the menisci, 3 degrees are distinguished:
- First degree - pathology cannot be detected by visual examination and palpation. The diagnosis can be made after histological examination of the punctate.
- Second degree - cystic formation is determined by a protrusion area on the lateral surface of the knee, because the cystic cavity is located outside the cartilage, in the perivascular area.
- The third degree is a cystic degeneration of the meniscal tissue and its adjacent capsule with the ligamentous apparatus, which is also called a parameniscal cyst.
What to do with a meniscal cyst: - If discomfort occurs in the knee while walking, you need to eliminate unnecessary trauma to it and minimize the load exerted, and then contact a traumatologist to establish an accurate diagnosis.
Treatment begins, as expected, with the elimination of pain. When choosing treatment tactics, the doctor is guided by the nature of the injury, its severity and location.
Cyst under the knee joint
A cyst under the knee joint (Baker's cyst) is a benign neoplasm that has a dense elastic structure and is characterized by stretching of the articular capsule and synovial membrane of the knee joint. Clinically manifests itself as an oval-shaped bulge in the popliteal area. A Baker's cyst is similar in structure to a hernia, since its body does not consist of individual cells, but is connected to the articular capsule. The popliteal cyst protrudes most strongly when the knee is extended, when the knee is bent - it is less dense and less convex. When a popliteal cyst grows large, it can limit movement in the knee, clog veins (leading to varicose veins), or can put pressure on nearby nerves and thereby cause numbness in the foot. When a cyst ruptures, pain occurs under the knee, fluid comes out of its cavity and spreads to the lower leg, causing it to swell. Surgical removal of Baker's cyst is by far the most effective treatment method and, accordingly, has positive results.
[20], [21], [22], [23]
Treatment without surgery
Conservative treatment without surgery is characterized by reducing the load on the knee joint and prescribing anti-inflammatory and painkillers. Pharmacological agents have a positive effect on cartilage tissue, promoting its rapid regeneration. In the acute period of pathology, narcotic analgesics can be used, they relieve pain, as well as non-steroidal anti-inflammatory drugs, the latter relieve pain and eliminate the inflammatory process. In addition to the above, the knee joint is fixed with a plaster cast or knee brace for no more than two weeks.
Surgical treatment
Indications for surgical treatment of meniscal cysts:
- large formations;
- unbearable pain in the knee joint;
- rapid progression of the disease.
Radical treatment involves complete excision of the parameniscal cyst along with degeneratively affected cartilage, but this treatment tactic is accompanied by a violation of the biomechanics of the joint along with progressive osteoarthritis. Because of this, in our time, arthroscopic resection is performed only on the parts of the cartilaginous plates affected by the cystic process.
Knee arthroscopy is a minimally invasive surgical procedure to diagnose and/or treat injuries to the inside of the joint.
The parameniscal cyst is removed through a small separate incision, or internal fenestration of the pathological formation is performed with drainage into the joint cavity.
Traditional methods of treatment
In traumatology, traditional medicine has a positive effect only in the early stages of pathology and is appropriate for small amounts of trauma. Folk remedies are mainly used by patients for conservative treatment in order to improve the effectiveness of medications. They are also used in the postoperative period, during recovery, strictly after consultation with the attending physician. But in reality, traditional methods of treatment play a role as a placebo effect - evidence-based medicine has not confirmed their effectiveness in traumatology.
Diagnosis of rupture
At the initial appointment, the doctor collects an anamnesis of the disease and examines the affected limb. To confirm the diagnosis, clarify the nature, severity and localization of the lesion, the patient is prescribed instrumental diagnostic methods:
- Radiography is a highly informative method for studying bone structures. It does not provide information about the presence of ruptures, but research is required to identify or exclude intra-articular fractures and the presence of loose bodies. X-rays are performed in frontal and lateral projections to obtain more accurate information.
- Ultrasound is based on ultrasonic waves that are reflected from tissues of different densities. This is a simple and safe research method that helps to quickly identify meniscal tears, cystic cavities, and degenerative processes.
- Computed tomography - like radiography, is based on x-rays, but unlike conventional research, it provides a three-dimensional image, from which even the smallest damage in bone structures can be seen. It is mainly prescribed for suspected fractures.
- Magnetic resonance imaging is the most informative method for diagnosing knee joint injuries. It provides clear images of soft tissues, three-dimensional images of the joint, which can reveal any damage to tendons, ligaments, cartilage, and also changes in bone tissue.
When making a diagnosis, differential diagnosis is carried out with diseases that may manifest with similar symptoms, for example, Goffre's disease, Koening's disease, reflex contracture.
Possible complications
Long-term cystic changes in the meniscus can cause degenerative changes in bone tissue, which results in the occurrence of deforming arthrosis. Postponing treatment until later is dangerous because the pathology can progress from the first degree to the third. And this will require much more time and money to restore the damaged knee. In addition, the wall of the cystic formation can rupture due to high fluid pressure in its cavity. The rupture is accompanied by sharp and severe pain, erythema, swelling and local fever.
Let's summarize: - timely attention to discomfort in the knee when walking will ensure a less difficult recovery process. People at risk should listen more carefully to their body's signals. If painful sensations appear, it is highly not recommended to self-medicate and let the injury take its course. On the contrary, you need to exclude additional stress on the knee and immediately contact a traumatologist.
Be healthy! Read the article: Baker's cyst of the knee
What happens if a meniscus injury is not treated?
It is impossible not to warn about the possible negative prospects that await the patient if he did not consider it necessary to receive medical help immediately after the traumatic incident. Walking with an incomplete element is fraught with the development of very unpleasant consequences, including:
- complete separation of a fragment of cartilage;
- severe degradation of the adjacent hyaline covers lining the surfaces of the articular bones;
- violation of the ligamentous apparatus;
- muscle atrophy of the problematic lower limb;
- the occurrence of arthrosis, arthritis, synovitis;
- intra-articular hemorrhage;
- “jamming” or instability of the knee, etc.
And this is only a small part of the serious complications that threaten a person if qualified surgical care is not provided in a timely manner. People with existing arthrosis or rheumatoid arthritis of local localization also need to be on alert, since a violation of the integrity of this organ can occur even at rest. Therefore, a systematic examination by the attending physician, diagnostic procedures, and a preventive course for such patients is a prerequisite!
Attention! The insidiousness of meniscus injuries that have not been treated is that at first severe pain can be disturbing for some time, then it may subside altogether, creating an imaginary idea of a successful recovery. And after several years, the once hidden pathogenesis manifests itself, but in a more sophisticated form - in addition with a complex of degenerative-dystrophic changes that generally cover the entire bone joint. Coping with significant degradation will already be very problematic. It is not a fact that all this will not ultimately lead to the forced need to remove the articular structure and install a total endoprosthesis.
CLASSIFICATION OF MENISCAL TEARS ON MRI
Ruptures vary in shape and location. Let's take a closer look at this. The following division is generally accepted:
The main types of meniscus tears: on the left - longitudinal, in the center - horizontal, on the right - radial.
Complex types of tears: on the left - “watering can handle”, in the center - patchwork tear, on the right - “parrot’s beak”.
If you look closely, you can see that complex ruptures are nothing more than a higher degree of each of the main types of ruptures. For example, a “watering can handle” is a complete longitudinal tear, a patchy tear is like a torn “piece” from a horizontal tear, and a “parrot’s beak” resembles a displaced radial tear.
Longitudinal tears
Three sagittal sections illustrating visualization of a longitudinal meniscal tear on MRI.
If a longitudinal tear is accompanied by displacement of a fragment of the meniscus towards the central parts of the joint, such a tear is called a complex “watering can handle” type tear.
MRI of the knee joint: irregular shape of the posterior horn. The fragment is missing. Right: displacement of the fragment into the intercondylar fossa.
The displacement of the fragment is clearly visible on coronal images. Typically, only two structures can be located in the intercondylar fossa - the anterior and posterior cruciate ligaments. Any other structure located there is most likely a displaced fragment of the damaged meniscus.
A special variation of the “watering can handle” is the inverted meniscus. This is when a torn fragment from the rear horn seems to flip onto the front horn, making it visually larger.
In the MRI image, the posterior horn is missing because it is inverted and is on top of the anterior horn.
Horizontal breaks
Horizontal ruptures are very often accompanied by the formation of cysts. Synovial fluid passing through the defect eventually accumulates and a meniscus cyst appears. This is of great practical importance for the surgeon, as it determines the scope of the operation.
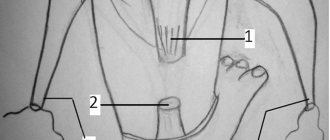
Horizontal rupture of the posterior horn of the medial meniscus with a parameniscal cyst.
Radial ruptures
The radial tear runs perpendicular to the long axis of the meniscus. Sometimes they can be difficult to recognize; this requires combining data from sagittal and coronal sections.
A broken butterfly pattern indicates a radial tear.
Radial meniscus tear on MRI
WHAT DOES THE MENISC LOOK LIKE ON MRI?
Normally, on MRI, the shape of the meniscus resembles two triangles, with their vertices facing each other. One triangle is the anterior horn of the meniscus, and the second is, respectively, the posterior horn.
As can be seen in the presented image of the medial meniscus, the posterior horn is always larger than the anterior one, and if this discrepancy is violated, then this indicates an abnormality in its shape, and may be a sign of a violation of the integrity of the meniscus. In the lateral meniscus on a sagittal section, the posterior horn is located higher than the anterior one, but their size should normally be the same.