Definition and functions of the meniscus Classification of injuries Possible causes of pathology Symptoms of a meniscus tear Degrees of severity of a meniscus tear Diagnosis of a meniscal tear Treatment of a meniscal tear of the knee joint Prevention of a meniscal tear of the knee joint
The knee joint is the most vulnerable part of the human body
, which is exposed to constant trauma and damage in everyday life. One such injury is a torn meniscus of the knee joint.
This closed injury is rarely accompanied by persistent pain.
, and therefore can remain unnoticed for a long time not only by the patient himself, but also by doctors. There are often cases when the victim is simply sent on sick leave with a recommendation not to put any weight on the sore leg.
But a meniscus tear is an insidious disease
, which leads to the development of intra-articular pathologies. It often provokes the appearance of erosions of the joint capsule, arthrosis and other degenerative and inflammatory diseases associated with deterioration of depreciation in the joint.
Young, physically active people between 20 and 40 years old are most susceptible to meniscus injuries, but a tear can occur at any age
. Elderly patients with problem joints are also susceptible to it. Let's figure out how to treat a meniscus tear in young and old people and what complications this condition is fraught with.
A torn meniscus is a common knee injury.
meniscus
meniscus
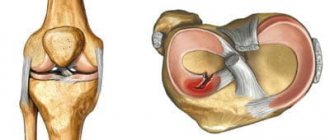
The joint space of the knee joint contains paired cartilaginous structures called menisci. The lateral (outer) and medial (internal meniscus) are distinguished. They are crescent-shaped and consist of a wider body, anterior and posterior horns. These structures perform important functions; they provide stabilization and shock absorption of the joint.
The outer meniscus is less rigidly fixed; under mechanical stress it can shift, so its damage develops less frequently. The inner meniscus is more rigidly fixed, so it is more easily and often damaged by excessive stress.
Since the horns of the menisci contain a smaller volume of cartilage tissue, a violation of the integrity usually occurs in the area of their localization. A more pronounced mechanical impact can cause damage to the meniscus in the area of the horns and body.
Signs
Since a person gets used to the aching pain in the knee, he may not notice the characteristic symptoms. Old meniscus damage is indicated by:
- frequent pain in the joint, worsening after long periods of standing and physical activity;
- relief after rest;
- restriction in movement - difficulties arise when trying to fully bend or straighten the leg;
- From time to time, reactive inflammation of the joint occurs, which is accompanied by redness and swelling. Synovitis may form.
If there is still no treatment, then the articular cartilage is gradually destroyed, which invariably leads to post-traumatic arthrosis. It is almost impossible to restore the joint in such cases. The person loses the ability to walk normally and uses a cane or wheelchair.
Etiology
Damage to cartilage in the form of a rupture of varying severity occurs due to the influence of various etiological (causal) factors, the most common of which are:
- Previous or acute knee injury that results from excessive flexion of the joint, a blow or fall on the joint, or twisting of the leg (rotation of the hip while the shin is locked). Traumatic changes predominantly occur in young people who lead an active lifestyle or engage in outdoor sports.
- Degenerative-dystrophic changes in cartilage tissue, developing against the background of age-related changes, nutritional disorders (trophism) and leading to a decrease in its strength. This reason often occurs in older people, which is associated with general age-related changes (involution processes).
- Congenital weakening of cartilage structures, caused by changes at the genetic level (the functional activity of genes responsible for the synthesis of the intercellular substance of cartilage tissue changes). Damage to the meniscus in this case develops against the background of normal stress in children or young people.
- Long-term inflammation of the structures of large joints, leading to disruption of their functional state. This etiological factor occurs during the development of an autoimmune pathological process (rheumatoid arthritis, rheumatism), characterized by the formation of autoantibodies by immunocompetent cells that affect their own tissues, mainly the structures of the musculoskeletal system.
Knowledge of the factors that became the main cause of meniscus damage allows a medical specialist to select the optimal rehabilitation, as well as make recommendations regarding the prevention of its development.
Kinds
Kinds
- Partial rupture, in which there is a focal violation of integrity while maintaining the general anatomical structure and shape of the meniscus.
- Complete rupture - a violation of integrity affects the entire thickness of the cartilage, resulting in a fragment that can be displaced relative to other structures of the knee.
To more accurately determine the severity of damage, there is a classification according to Stoller, which distinguishes 4 degrees:
- Grade 0 – no changes.
- Grade 1 – there are small focal changes.
- 2nd degree - more pronounced changes that have a linear shape and do not extend beyond the surface of the cartilage.
- Grade 3 – changes affect the entire thickness of the cartilage, with a complete rupture of the meniscus.
Classification of a tear of the medial meniscus of the knee is possible based on the results of a thorough clinical examination, as well as objective diagnostic data, in particular using MRI (magnetic resonance imaging is necessary for Stoller classification).
Radiographic imaging
Radiographic imaging
Arthroscopic diagnostic examination is also performed for therapeutic purposes. In this case, special manipulators and small-sized instruments are introduced into the cavity of a large component of the musculoskeletal system.
Symptoms
Damage to the internal meniscus of the knee in the form of a tear is characterized by the appearance of several main clinical signs:
- Pain localized mainly on the inside of the knee. Its intensity depends on the cause of the injury (after an injury the pain is acute, but during degenerative processes it develops gradually). It increases when trying to perform movements in the knee, as well as against the background of loads on the lower limbs.
- Limitation of mobility with a decrease in the range of movements in the knee, up to complete block, which occurs with a complete rupture of the meniscus, accompanied by a sharp onset of acute pain.
- Inflammatory signs include redness of the skin (redness), swelling of the soft tissue (edema), and increased pain that may be present at rest.
The severity of clinical symptoms depends on the location and severity of the pathological process. With the gradual destruction of cartilage tissue against the background of degenerative-dystrophic processes, signs appear gradually, they can intensify over a fairly long period of time.
Indications for surgery
For what diagnoses is surgery indicated - suturing the meniscus of the knee joint, cutting off the disintegrated edges or its complete removal, inserting a synthetic implant? Common problems requiring corrective surgery include the following types of injuries, confirmed by MRI and radiography:
- separation of a flap (fragment) of the meniscus;
- central longitudinal gap;
- large-scale fragmentation;
- rupture along the periphery with or without displacement.
Types of meniscal tears.
As for the separation of the cartilage flap: here it is urgent to perform surgery on the meniscus of the knee joint; the postoperative period will need to be taken as seriously as possible. If the necessary measures are not taken in time, the free existence of the severed body will impede movement, cause terrible pain and block the knee. The separated fragment, however, like the dangling piece, will begin to create a mechanical obstacle, since during the motor act it will fall into the main working center of the joint.
Schematic representation of the result of suturing the meniscal horn.
Important! It should be clearly understood that the speed and fullness of the return of functional potential subsequently depends on compliance with a special postoperative regimen, and it does not matter what type of manipulation was carried out - correction or removal.
Rehabilitation after surgery on the meniscus of the knee joint is no less significant than the plastic surgery of the functional element itself. Therefore, in no case should you neglect the basic recommendations that will be given by a specialist. Only flawless adherence to a recovery program based on improvement of the ligamentous apparatus and regeneration of the operated area will allow for a quick and successful rehabilitation, as well as avoiding quite dangerous complications.
Conservative therapy
Conservative therapy
Once a medial meniscus tear has been diagnosed, treatment without surgery is prescribed only on the basis of certain criteria, which include the location, characteristics and severity of the damage. The medical specialist must take into account the cause of the pathological condition.
It is usually possible to prescribe conservative measures if small changes have been identified that do not extend beyond the surface of the cartilage. An incomplete meniscal tear can be treated without surgery using medications, physical therapy, and rehabilitation measures. During treatment, the knee is provided with functional rest, which is achieved by immobilization (immobilization) using tight bandages or a plaster splint.
rehabilitation
rehabilitation
If the patient is treated with conservative methods after a meniscus injury, the limb must be immobilized. But if he has undergone surgery, this is not always done. There are different opinions among doctors regarding the need to immobilize the leg with bandages. Many people are of the opinion that avoiding immobilization contributes to better preservation of the tone and volume of the thigh muscles.
By refusing immobilization, other effects are achieved:
- trophism of the joint capsule improves;
- less risk of developing degenerative processes of hyaline cartilage;
- there are no degenerative changes in bone tissue.
Physical exercise is a must. They form the basis of the rehabilitation process. Rehabilitation after a meniscus injury involves:
- isometric tension of the quadriceps femoris muscle;
- walking on a flat surface;
- active movements in the operated knee joint, which are performed initially in the unloading position;
- exercises for all muscle groups aimed at maintaining the general physical condition, nonspecific resistance of the body, and the patient’s vitality;
- training on special simulators.
Physiotherapy methods are used. They improve the recovery processes of the meniscus and soft tissues of the knee by improving blood circulation. During the initial recovery period, cooling procedures are used. Cryotherapy, hydromassage, and pneumomassage are widely used.
Thermal procedures begin no earlier than 4 days of rehabilitation. This could be UHF, electrical stimulation of the thigh muscles, magnetic therapy, etc.
Features of early rehabilitation
Drug treatment
Medicines, their dosage and regimen of use are determined by a medical specialist individually for each patient, necessarily taking into account various factors, such as the person’s age, gender, location and severity of damage. Drug therapy primarily includes the use of drugs from several pharmacological groups:
- Non-steroidal anti-inflammatory drugs - drugs are used to reduce the severity of inflammation of moderate intensity. Usually tablet or injectable dosage forms are prescribed in combination with drugs for external use (cream or ointment).
- Glucocorticosteroids are hormonal drugs that are prescribed for severe long-term inflammation, in particular against the background of an autoimmune reaction.
- Chondroprotectors are a group of drugs that reduce the rate of destruction of cartilage tissue and also promote its restoration.
- Vitamins - allow you to speed up the process of tissue regeneration, as well as improve the general condition of the patient.
As an alternative method of conservative therapy, intra-articular administration of platelet mass (a biological preparation that is a suspension of platelets in physiological solution) is possible. It contains biologically active compounds “growth factors” that stimulate regeneration processes in cartilage and connective tissue.
Physiotherapeutic procedures
Physiotherapy involves the use of various physical factors that reduce the severity of inflammatory, degenerative-dystrophic processes, and also promote faster tissue restoration. For this, depending on the severity of the pathological process and the technical capabilities of the medical institution, the following can be used:
- ozokerite;
- mud baths;
- electrophoresis with various anti-inflammatory drugs.
The duration of use of physiotherapeutic procedures is determined individually by a medical specialist. They are usually combined with drug treatment.
Injection in the knee
Injection in the knee
It is important to comply with several conditions:
- Disciplined compliance with all medical prescriptions and recommendations.
- Providing rest for the lower extremities.
- Periodic visits to the doctor to monitor the effectiveness of the prescribed therapy.
- There is no need for parenteral (intramuscular, subcutaneous or intravenous) administration of drugs.
If injections are necessary in certain cases, treatment can also be carried out at home, but manipulations can only be performed by medical personnel or the patient must visit the manipulation room of a medical institution.
Folk remedies
Some medicinal plants (medicinal chamomile, St. John's wort, burdock) have an anti-inflammatory and decongestant therapeutic effect. They can be used as an additional component of therapy.
However, before using them, you should definitely consult a medical specialist. An attempt at self-treatment can lead to the development of various complications, including allergic reactions.
physical therapy complex
complex of physical therapy
After the basic therapeutic course, restorative procedures and measures are prescribed. They involve special physical training in a physical therapy complex (PT). In this case, the load on the knee increases in stages, and this allows the cartilage structures to adapt to it in order to avoid repeated damage.
Due to the fact that the joint is in a state of functional rest for quite a long time, there is a risk of developing contractures (connective tissue adhesions), so rehabilitation with exercises is necessary to prevent the development of this complication. The duration of the course of such measures depends on the type of treatment performed, as well as on the severity of the damage. Typically it varies over a period of time from several months to six months.
Diagnostics
Detection of ruptures can be difficult due to injuries to nearby soft tissues, so a comprehensive diagnosis is required. First of all, they collect an anamnesis of the disease - find out the circumstances of the injury, the nature, and severity of pain. Next, a visual examination of the affected knee is carried out for the presence of swelling, deformation, hemarthrosis, and the volume of passive and active movements is assessed.
To recognize injury, there are a number of special tests, for example, McMurray. The patient is placed on his back, the knee joint is bent as much as possible, the lower leg is rotated and displaced, then extended at the knee joint. The test will be considered positive if there is a click, which indicates an unstable meniscus fragment.
After collecting anamnesis and examination, instrumental diagnostic methods are prescribed to visualize the rupture and possible complications:
- X-ray – the meniscus tear cannot be seen in the image, but the study clearly shows the bone structures. It is necessary to confirm or exclude intra-articular fractures and bone cracks. Pictures are taken in several projections to obtain maximum information.
- Ultrasound examination is a safe diagnostic method that does not cause radiation exposure to the body, so it can be performed repeatedly. Ultrasound reveals meniscus tears, separation of its fragments, degenerative processes, post-traumatic cysts.
- MRI is a highly informative diagnostic method for assessing soft tissue structures and cartilage. Helps assess the degree of rupture and select the optimal treatment tactics.
- CT scan is similar to radiography, but provides a three-dimensional image. The study is necessary if complex injuries of the tibia and femur are suspected.
In some cases, patients are prescribed arthroscopy. Unlike other methods, this is an invasive procedure in which an instrument is inserted into the joint cavity.