Causes of synovial cyst formation
The causes of this pathology have not yet been precisely determined by science. However, frequently occurring concomitant inflammatory diseases of the joints have been noted - arthritis, arthrosis, osteoporosis, etc.
Risk factors for the disease include:
- inflammatory processes in joint tissues;
- injuries;
- constant loads or their incorrect distribution;
- Unhealthy Lifestyle;
- in rare cases, it can form during fetal development.
Symptoms
At the stage of disease development, it is quite difficult to assess symptoms for the first time. While the size of the cyst is small, the patient rarely attaches importance to the changes, but as it grows, he may notice:
- the appearance of an elastic lump under the skin;
- discomfort when working the joint;
- numbness of skin areas.
Synovial formation of a joint
In an advanced state, the neoplasm leads to the following:
- deterioration of joint mobility;
- pain in the affected joint;
- swelling at the site of localization;
- numbness of the extremities (spinal cyst).
Despite the upward trend, the nature of the formation is benign. An articular cyst does not become a malignant tumor and does not cause metastases.
Varieties
Morphologically, all articular cysts are similar to each other. They are divided by location. In the International Classification of Diseases ICD-10, education is assigned two codes:
- 2 – synovial cyst of the popliteal region (Baker).
- 3 – another cyst of the synovial bursa.
Synovial cyst of the popliteal region
A popliteal cyst, or Baker's cyst, is a characteristic accumulation of joint fluid in the back of the knee joint, due to its anatomical structure. It often occurs in professional athletes, but rheumatic inflammatory processes can also be the cause.
Named after the 19th century surgeon who first described this formation in the popliteal region. Causes pain, the bend angle of the knee joint decreases.
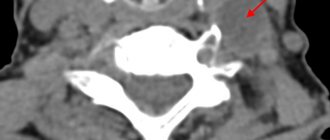
Spinal cyst
Spinal cyst is the most dangerous of the subtypes. Most often it forms in the lumbar and cervical regions. In most cases, it develops asymptomatically, is diagnosed already in an advanced state and may require excision.
Depending on the location of the cyst in the spinal column, symptoms may vary significantly. Monitor your body carefully and consult a doctor immediately if you notice the following changes:
- the appearance of pinpoint pain;
- dizziness, tinnitus;
- headache;
- increased back pain when moving;
- numbness of the limbs;
- muscle weakness;
- malfunctions of the gastrointestinal tract or bladder;
- blood in the urine.
A complex of approaches is used in treatment. If possible, the doctor tries to avoid surgical intervention due to the increased risk and complexity of the operation. But sometimes conservative treatment is not enough. In the absence of alternatives, it is impossible to refuse surgical intervention due to the seriousness of the complications that arise.
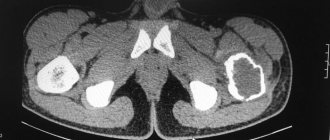
Neoplasm on the spine
Other types of synovial cyst
One of the typical localizations is the area of the wrist joint. Typically, the bulge forms on the back of the hand. Movement of the hand is difficult and painful. There is numbness in the fingers. Similarly, if localized in the ankle, the foot may become completely numb.
Synovial formations also occur in large joints. A hip cyst leads to loss of mobility. A specific symptom may be the so-called starting pain, which appears at the beginning of movement after a period of rest.
Damage to the shoulder joint does not make itself felt for a long time and is asymptomatic for up to several years. Then, as in other cases, discomfort, pain, swelling and numbness appear. It often occurs in the elderly, athletes or those engaged in labor related to carrying heavy loads.
Less common are cysts of the fingers and toes. They are usually inactive and painless, but also require close attention.
Synovial cyst (wrist hygroma)
Home > Wrist pain
I prefer to call hygromas and other tendon ganglia synovial cysts. Firstly, this term most accurately describes the bubble with walls made of connective tissue (synovium) and gel-like contents inside, which the surgeon sees during surgery. Secondly, that’s what they were called where I studied. A synovial cyst in the hand area is the most common neoplasm on the hand. People go to the doctor with complaints of periodic pain that intensifies with exercise, they do not like the appearance of the hand, and sometimes there is a fear of a tumor and malignant degeneration. In fact, the literature does not describe the degeneration of a synovial cyst into a malignant tumor, if it is indeed a synovial cyst.
Various treatment methods are possible, let's start discussing them from simple to complex. The simplest thing is observation - if this “hygroma” does not grow, does not hurt and does not interfere with life, then there is no need to rush. Sometimes they go away on their own.
In the case when a person still wants to get rid of this “disease,” he may be offered different options. Old school surgeons suggest crushing them under the skin, and this can be an effective procedure. The disadvantages are that it is painful, and the cyst may appear again over time. To enhance the effect, folk medicine suggests using not only fingers for crushing, but also a hammer or even a Bible.
A very elegant way is to puncture the cyst followed by the administration of an anti-inflammatory drug. This works especially well if the puncture is performed under ultrasound guidance. A lasting effect persists in 20-30% of patients. There are times when such manipulation is irreplaceable. For example, when the only manifestation of a cyst is pain, it is so small that it can only be seen with an ultrasound or MRI. Then the precise administration of a small dose of steroids can relieve a person of pain and discomfort.
The most reliable way to remove a synovial cyst is surgery. With complete excision of the cyst, relapses, although possible, are extremely rare. The operation is performed on an outpatient basis (there is no need to stay in the hospital) under local anesthesia (without general anesthesia), the procedure itself takes about 40 minutes, rarely when the patient stays in the clinic for more than 2 hours. After 2 weeks, the sutures are removed, and I also recommend using a fixator for 3 weeks to relieve the load on the operated arm. Arthroscopy has also been described, which can eliminate capsule defects on the joint side. The results of arthroscopic and open removal of synovial cysts are comparable.
The estimated cost of surgical treatment of this pathology is 15,000 - 50,000 rubles, depending on the method of operation
You might be interested in:
- Arthrosis of the wrist joint
- De Quervain's tendonitis (styloiditis)
- Arthrosis of the first metacarpal joint
Diagnostics
If you suspect you have a synovial cyst, do not delay going to the doctor. It is important to treat its root causes and consequences with an orthopedist.
For primary diagnosis, a doctor may need to perform an examination and collect an anamnesis. But to confirm the diagnosis and determine the etiology of the disease, a number of diagnostic procedures are used:
- general analysis (blood and urine);
- rheumatic tests (blood tests to detect inflammation in the joints);
- X-rays from different angles to detect displacement or injury;
- myelography – radiography of the spinal cord with the introduction of a contrast agent;
- Ultrasound – to identify abnormalities in tissue structure;
- MRI;
- puncture of cyst contents;
- arthroscopy (diagnostic).
Hand surgery
The hand is our intermediary in the material world, it transmits information and fulfills our will, expresses feelings. This is the finest living instrument, which even the most advanced machines cannot come close to. “It’s like having no hands,” we say about the most necessary things. “Lending a helping hand” is about a noble act.
And who will lend a helping hand if trouble happens to the limb itself? This cannot be done without qualified, partly narrow, specialists. The fact is that the hand has many specific differences from other parts of the body. Small but very important anatomical formations that require exceptional attention are concentrated in a small area. Damage to tendons and nerves that are only a few millimeters in diameter can lead to permanent disability in an instant. The hand has complex and delicate biomechanics. Hand treatment requires special skills, deep knowledge, special tools and equipment. Hand surgery is by no means a minor surgery and there are no size discounts.
Hand surgery formed into a separate area of traumatology and orthopedics in the middle of the last century and since then has been constantly developing, opening up new horizons of possibilities. It combines orthopedics, traumatology, vascular, plastic surgery, and neurosurgery.
Our clinic provides state-of-the-art treatment for injuries, consequences of injuries and diseases of the upper limb.
Injuries:
- Open and closed fractures of the metacarpal bones and phalanges of the fingers, carpal bones, radius
- Damage to nerves at the level of the fingers, hand, and forearm.
- Damage to tendons at all levels of extensors and flexors.
- Dislocations of open and closed phalanges of the fingers, metacarpal bones, bones of the wrist, hand, head of the ulna.
- Combined injuries, gunshot wounds, severe injuries.
Consequences of injuries:
- Fractures healed with displacement, false joints.
- Old dislocations.
- Old flexor tendon injuries.
- Old extensor tendon injuries.
- Old nerve damage.
- Post-traumatic contractures – tenogenic, neurogenic, arthrogenic, cicatricial, mixed origin.
- Amputation shortening of the phalanges of the fingers and metacarpal bones.
Diseases:
- Diseases of the synovial membranes (chronic tenosynovitis, synovial cyst, nodular tenosynovitis, stenosing ligamentitis, de Quervain's disease)
- Tumors and tumor-like diseases (lipoma, gigantoma, glomus tumor, hemangioma, exostoses and bone osteophytes, enchondroma, ecchondroma, osteoid osteoma, neurofibroma, oleoma, mucosal cyst, vascular aneurysm, epidermal cyst, bone cyst)
- Degenerative-dystrophic diseases (Dupuytren's contracture, Sudeck's syndrome, tunnel syndromes, Ollier's disease, Kienbeck's disease, deforming arthrosis of the wrist and finger joints).
- Congenital hand diseases (clinodactyly, polydactyly, syndactyly).
Contact a specialist - a hand surgeon if:
- There was an accident and you injured your hand. Pay attention to such points as the presence of a wound, deformation, abnormal mobility, lack of normal mobility, decreased sensitivity, change in skin color, and the presence of foreign bodies.
- You have an old injury, and you are worried about pain, limitation of movements, deformation, the presence of a scar, non-healing wound, or foreign body.
- You have discovered a tumor.
- Decreased mobility, sensitivity and strength of the limb
The most common hand diseases:
- Subcutaneous extensor tendon rupture
Most often, such injuries are the result of sharp, forced bending of a tense finger. The tendon tissue at the level of the extreme joint cannot withstand it. The phalanx “hangs” and stops straightening. The pain is usually minor.
Treatment.
The essence of treatment is to fix the nail phalanx in the position of maximum extension. In this position, the ends of the damaged tendon come closer together, and within the prescribed 6 weeks they grow together with a strong scar. The easiest and safest way is external fixation using a special splint. It is given the required shape and placed on the finger. The disadvantage of this method is the need to take care of the splint for a month and a half, making sure that the fixation continues to remain reliable and the position is correct. If the patient’s work is manual, and a month and a half of incapacity for work is an unaffordable luxury, or if you don’t want to appear in public with a bandage, or you simply need a reliable result, then surgical treatment is indicated in these cases. The phalanx is fixed using a knitting needle. The needle sinks under the skin and allows full use of the hand. During your consultation, your doctor will help you choose the treatment method that is right for you.
A slightly different situation is a rupture of the extensor pollicis longus tendon. Most often this occurs some time after a fracture of the radius. The tendon undergoes a degenerative change and at one point cannot withstand it and ruptures. The thumb does not straighten. The peculiarity here is that it will not be possible to sew such a tendon end-to-end, as with a fresh injury with a sharp object. Transposition (transplantation) of one of the extensor tendons of the index finger into the position of the extensor of the thumb is used. After a short “retraining”, the patient begins to use the redirected muscle in accordance with its new role.
Synovial cyst
A synovial cyst (the outdated name is hygroma) is not a tumor in the strict sense of the word. It is a protrusion of the joint shell beyond its capsule. It appears in the form of a “bump” above the joint, its favorite localization is the radiocarpal joint, others are also affected.
Appears as a result of injury, constant overload, due to inflammation. There may be no visible reason; in these cases, the constitution of the body is “to blame” - weakness of the connective tissue. The most common complaint is pain during exercise, but often a synovial cyst does not cause complaints, creating only aesthetic discomfort.
Treatment
In some cases, conservative treatment (immobilization, anti-inflammatory therapy, pressure bandages) leads to success, but not always. The decision on the need for surgical intervention is made taking into account the severity of the process, the nature of the complaints and subjective sensations. In any case, it is necessary to exclude the presence of diseases with similar external manifestations - tumor and tenosynovitis.
Dupuytren's contracture
This is a cicatricial degeneration of the palmar aponeurosis, the dense “lining” of the palm, leading to persistent limitation of finger extension. Without treatment it progresses.
Treatment
Mostly surgical. Excision of the altered areas of the aponeurosis is performed, followed by gradual removal of the fingers from the vicious position. To achieve the best results in the postoperative period, it is necessary to wear a special splint that prevents bending of the fingers and the occurrence of relapse.
Dislocations.
For a completely unknown reason, many people have the belief that a dislocation is “no big deal, just a dislocation.” In fact, unlike many other injuries, it is a dislocation that necessarily requires medical intervention. Precisely medical. Pulling it like in the movies or applying ointment like in the commercials won’t work. Dislocation is a severe damage to the joint, accompanied by separation of the articular surfaces, in 100% of cases leading to permanent impairment of joint function. The simplest thing that may be required is the removal of a dislocation, a medical procedure aimed at restoring the normal relationship of the bones. Let us emphasize, medical manipulation. The best thing to do on your own is to rest the limb and seek help immediately. It is usually not difficult to recognize a dislocation - after the injury, there is an unnatural position of the limb or its segment, pain, severe swelling and almost complete impossibility of movement.
Dislocation of finger, phalanges
Even with timely treatment, it is not always possible to eliminate the dislocation closed, without surgery. The situation becomes much more complicated if a week or more has passed since the injury. Old (more than 3 weeks) dislocations can only be treated surgically.
Fracture-dislocation of a finger, phalanx, metacarpal bone
This is an injury in which the articular end of the bone is fractured, and part of it remains in place, held by ligaments, while the entire bone moves out of its place - dislocates. The main method of treatment is surgical.
Dislocations in the wrist joint.
There is a wide variety of dislocations and fracture-dislocations in the wrist joint. In all cases this is a serious injury. Without treatment - loss of function, often neurological disorders. In some cases, treatment costs “little blood”, but only with timely treatment.
Old dislocation.
One of the most unpleasant situations in traumatology. Damaged tissues, including the joint capsule and ligaments, turn into rough, hard scars and make it impossible to eliminate the dislocation without surgery. Surgical treatment often has to be carried out in two stages. First, the joint is stretched using a special apparatus, then open or closed reduction is performed, followed by metal fixation.
Treatment
After making a diagnosis and identifying associated disorders in the body, the doctor determines the method of treatment. Depending on the degree of development of the cyst, its location and the causes of its occurrence, conservative therapy, surgical intervention, or their combined use are used.
Drug treatment
In cases where a cyst forms against the background of inflammatory processes, the use of pharmaceuticals is necessary. Inflammatory processes can be caused by disruption of the immune system or metabolism, or infections. In these cases, treatment may include:
- anti-inflammatory drugs;
- antihistamines;
- corticosteroids;
- antibiotics;
- chondroprotectors.
Remember that only the attending physician can prescribe medications. Self-medication is unacceptable.
Non-invasive therapy
If the tumor is small in size, some effective non-invasive methods and procedures are often used in combination with drug treatment:
- stabilization of the joint with a special corset;
- massage;
- transition to a balanced diet;
- inclusion of vitamins B and C in the diet;
- suitable physical therapy exercises.
Ultrasound therapy is also effective for treatment. Its effect on the joint fights inflammation, accelerates the healing process, and has an analgesic and relaxing effect.
If you're a fan of alternative medicine, consider acupuncture or its modern equivalent, electroacupuncture. Experts in this field report the positive effect of the procedure on joint rehabilitation. It is believed that such stimulation normalizes collagen production, improves the properties of synovial fluid and accelerates tissue regeneration.
The use of non-invasive methods is also discussed with a doctor and is not prescribed independently.
Surgical intervention
When the cyst has developed so much that only conservative methods are powerless, surgical excision is used. The choice of surgical intervention method depends on the nature of the formation and the factors of its occurrence:
- Puncture or incision of the cyst and drainage of its cavity. A minimally invasive operation with minimal risks of complications, but less effective than complete excision. Since the synovial lining continues to fill the cavity with joint fluid, relapses occur in most cases.
- Complete removal of the formation is the most effective treatment method. The walls of the cyst are opened, the joint fluid is sucked out, the body of the cyst is completely removed and plastic surgery of the synovial membrane of the joint is performed if necessary. The indication for surgery is often localization in the spinal column.
What is a Baker's cyst? How to treat?
Surgeon of surgical department No. 1 Alnadfa M.N.
Baker's cyst, or popliteal fossa cyst, is a dense, soft and elastic tumor-like formation located on the surface of the knee joint behind (in the popliteal fossa).
Causes of cysts
A Baker's cyst can be a consequence of either injury or previous disease of the knee joint:
- joint injuries;
- damage to joint cartilage;
- damage and degeneration of meniscus changes;
- osteoarthritis;
- patellofemoral arthrosis;
- inflammation of the synovial membrane of the joints (chronic synovitis);
- osteoarthritis;
- rheumatoid arthritis.
Complications
Untimely treatment of Baker's cyst can cause the following complications:
- rupture of a Baker's cyst due to high pressure with tumor enlargement. When ruptured, the contents of the cyst spill into the intermuscular space of the upper third of the leg, causing pain, swelling, as well as redness and fever. Note that cyst rupture is the most common complication of this disease;
- compression of the tibial nerve, resulting in numbness, tingling or muscle weakness in the knee joint;
- compression of lymphatic and blood vessels, resulting in pain and swelling of the lower leg;
- the occurrence of deep vein thrombosis and thrombophlebitis of the leg;
- the appearance of varicose veins of the saphenous veins of the leg, as a result of compression of the veins.
Diagnostics
Diagnostic research methods that make it possible to accurately determine the presence of a cyst, its size, as well as the connection of the cyst with other elements that make up the knee joint are:
- X-ray of the knee joint;
- Ultrasound of the knee joint;
- arthroscopy of the knee joint;
- MRI of the knee joint.
It is also necessary to puncture the cyst itself, followed by extraction of its contents for studies of the intracystic fluid.
Treatment
- drug therapy;
- by surgical intervention.
If the pathological formation is not in an advanced state, you can limit yourself to conservative treatment. The first thing the patient needs to do is immobilize the affected knee. A bandage will help with this. However, it should not be too tight, otherwise it may interfere with normal blood circulation. In addition, in the first days after the appearance of unpleasant symptoms, ice compresses are good, which should be kept for no more than 20 minutes.
How to treat Baker's cyst with medication:
- chondroprotectors (Chondroitin sulfate);
- NSAIDs (Naprofen, Indomentacin, Diclofenac);
- steroid hormones (Prednisolone, Hydrocortisone);
- ointments that reduce inflammation (Troxevasin, Fastum-gel).
A popliteal fossa cyst can also be treated with exercise therapy. However, before doing such exercises, you should consult a physiotherapist. More often, gymnastics is used to increase muscle elasticity. These exercises can only be done if the cyst is caused by a degenerative-inflammatory process occurring in the knee joint.
Baker's cyst drainage
The second name for this procedure is aspiration. During this manipulation, the
synovial cyst of the popliteal fossa. After this, using an empty syringe with a needle, the fluid is pumped out from the cyst.
Treatment of Baker's cyst with laser
The beam temperature reaches 800°C. It has hemostatic and antibacterial effects. The procedure using it is recommended when the cyst reaches a large size. The popliteal cyst is removed under local anesthesia.
Surgery to remove Baker's cyst
If drug therapy and physiotherapy do not give a positive result, drastic measures are resorted to. Baker's cyst of the knee joint is large for surgery. Surgical intervention may be as follows:
- Using an arthroscope , a device with instruments is inserted through two incisions made in the popliteal cavity. First, the liquid is pumped out, then the capsule itself is removed.
- Classic surgery - an incision is made in the skin, the capsular cyst is excised, and then a suture is placed on the incision. A tight bandage is placed on top of the knee.
Possible complications
If timely diagnosis and treatment are not carried out, there is a risk of irreversible complications. In an advanced state, the cyst puts pressure on tissues, blood vessels and nerves. Muscle atrophy progresses, blood flow becomes difficult, swelling and varicose veins appear.
Of particular danger are blood clots that occur when blood stagnates in the veins. Once detached, they can migrate, causing fatal complications.
Lack of blood supply also affects bone tissue. Osteomyelitis develops, necrotic processes occur in the bones, causing sepsis.
A cyst that increases in size can rupture, infect surrounding tissues and provoke the development of arthrosis.
A formation even on the interphalangeal joint of a finger can, in case of complications, lead to complete loss of mobility. If there is a rupture in the hip joint, paralysis of the legs is likely.
If you suspect the appearance of neoplasms, consult your doctor.