Causes of bone cysts.
The causes of bone cysts have not yet been studied in detail. The disease can appear as a result of previous injuries (dislocations, falls, bruises, etc.). It also affects people suffering from rheumatoid arthritis, osteoarthritis and chronic gout. Bone cysts increase the risk of developing fractures because... when they form, the volume of bone tissue decreases, and the bones can no longer withstand the previous load and break easily.
The disease can be asymptomatic for a long time and be discovered accidentally during a fracture or during an X-ray examination for another reason. Sometimes a bone cyst can cause swelling and pain.
Symptoms of a spinal cyst
Symptoms and treatment of cysts in the lumbar spine, as well as its other areas, may not appear for a long time. However, as the disease progresses, the following signs appear:
- pain in the affected area, and gradually the pain can spread to the buttocks and legs;
- the chronic nature of the pain, it can occur both during active movement and when at rest;
- the occurrence of pain in the head, dizziness, tinnitus (typical of an arachnoid cyst of the spine);
- development of various neurological pathologies;
- decreased sensitivity and numbness of the limbs;
- the appearance of pins and needles in the arms and legs;
- sometimes there are disturbances in the functioning of the gastrointestinal tract and genitourinary system;
- in more advanced cases, lameness may occur and the functioning of the vestibular apparatus may be disrupted.
Treatment of bone cysts
The conservative treatment method includes a course of therapeutic punctures (two needles are inserted into the body of the cyst, with the help of which fluid is sucked out, medications are administered to reduce bone destruction), the application of a plaster cast (if there is a fracture), physiotherapeutic treatment, and a course of therapeutic exercises. If there is no result from conservative treatment, the patient undergoes surgical treatment.
Neglect of the disease and lack of necessary treatment can lead to destruction and death of bone tissue, which may entail complete removal of the damaged part.
Aseptic bone necrosis
- a disease in which death (necrosis) of bone areas and bones as a whole occurs as a result of disruption or complete cessation of blood flow in a certain area of the bone. Idiopathic aseptic necrosis develops spontaneously without any particular reason. There are complete and partial necrosis of the bone, and also a distinction is made between superficial and deep necrosis depending on its location in the bone. The disease occurs in several stages.
Diagnostics
A spinal cyst is diagnosed by a neurosurgeon. The doctor prescribes a comprehensive examination:
- a medical history is collected: visual examination, palpation, the patient’s complaints are taken into account;
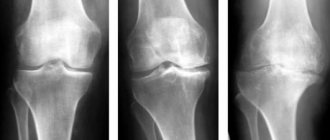
- X-ray of the spine in different projections;
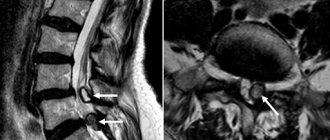
- computed tomography or magnetic resonance imaging;
- Ultrasound of the spine;
Additionally, the neurosurgeon may prescribe myelography. Contrast liquid is injected into the spinal canal, thus examining the pathways for obstruction.
If it is necessary to examine the spinal roots, electromyography is prescribed.
A biochemical test of blood and urine is required.
Neck cyst
Lateral neck cysts
Lateral neck cysts are more common than median ones (in approximately 60% of cases). They are located on the anterolateral surface of the neck, in its upper or middle third, anterior to the sternocleidomastoid muscle and are localized directly on the neurovascular bundle, next to the internal jugular vein. There are both multi-chamber and single-chamber. Large lateral neck cysts can compress blood vessels, nerves and nearby organs.
Symptoms
In the absence of suppuration or compression of the neurovascular bundle, there are no complaints. During the examination, a round or oval tumor-like formation is revealed, especially noticeable when the patient’s head is turned in the opposite direction. Palpation is painless. The cyst has an elastic consistency, is mobile, is not fused to the skin, and the skin over it is not changed. As a rule, a fluctuation is determined, indicating the presence of fluid in the cyst cavity. Upon puncture, a turbid, off-white liquid is found in the cavity of the formation.
Complications
When suppuration occurs, the neck cyst increases in size and becomes painful. The skin over it turns red, local swelling is detected. Subsequently, a fistula is formed. When opened on the skin, the mouth of the fistula is located in the area of the anterior edge of the sternocleidomastoid muscle. When opened on the oral mucosa, the mouth is located in the area of the upper pole of the palatine tonsil. The hole can be either pinpoint or wide. The skin around the mouth often becomes crusty. Maceration of the skin and hyperpigmentation are observed.
Diagnostics
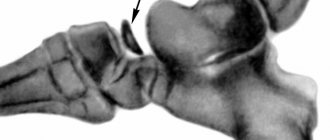
The diagnosis of a lateral neck cyst is made based on the history and clinical picture of the disease. To confirm the diagnosis, a puncture is performed followed by a cytological examination of the resulting fluid. Additional research methods such as ultrasound, probing and fistulography with X-ray contrast agent can be used.
For an uninfected neck cyst, differential diagnosis is carried out with lymphogranulomatosis and extraorgan tumors of the neck (lipoma, neuroma, etc.). A suppurating cyst is differentiated from adenophlegmon and lymphadenitis.
Median neck cysts
Symptoms
Median cysts in traumatology make up about 40% of all neck cysts and are located on the anterior surface of the neck, along the midline. Upon examination, a dense, painless, clearly demarcated formation of elastic consistency with a diameter of up to 2 cm, not fused to the skin, is revealed. The cyst is slightly mobile, fused to the body of the hyoid bone, and moves when swallowing. In some cases, the tumor-like formation is located at the root of the tongue. In this case, the tongue rises, and speech and swallowing problems are possible.
Complications
Median cysts suppurate more often than lateral cysts - in approximately 60% of cases. When infected, the formation increases in size and becomes painful. The surrounding tissues swell and the skin turns red. When the abscess is opened, a fistula is formed with an opening located on the anterior surface of the neck, between the thyroid cartilage and the hyoid bone. If the fistula opens into the oral cavity, its mouth is located on the front surface of the tongue, on the border between its root and body.
Diagnostics
The diagnosis of a median cyst is made based on history and clinical data. Ultrasound and cyst puncture followed by cytological examination are used as instrumental diagnostic methods. During puncture, a viscous, turbid, yellowish liquid containing lymphoid elements and cells of stratified squamous epithelium is obtained. Fistulography and probing are used to study fistulous tracts.
The median cyst of the neck is differentiated from struma of the tongue, dermoid cyst, lymphadenitis, specific inflammatory processes and adenoma of an abnormally located thyroid gland.
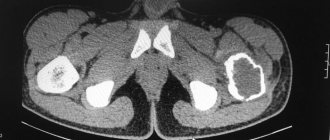
CT scan of the neck. To the left of the midline in the carotid space there is a cystic formation (cystic lymph node).
Alternative medicine
If a cyst is detected, treatment with traditional methods can only be carried out if there is a small neoplasm that has not yet led to central nervous system disorders and has not provoked displacement of the vertebrae.
Elecampane is considered the most effective remedy for the appearance of a sacral cyst. In this case, it is used in the form of an infusion, which is prepared as follows: take 1 tbsp. l. raw materials, pour 3 liters of boiled water and infuse for several days in the refrigerator. After this, the infusion is filtered and taken ½ glass 2 - 3 times a day.
Thistle, or rather its juice, is also an equally effective remedy in the treatment of this disease. To obtain it, the plant is crushed, minced in a meat grinder and infused for 72 hours. The juice that comes out must ferment. It should be taken 20 - 30 ml before each meal.
It is necessary to understand that cysts that occur in the spinal column are dangerous and can lead to serious health problems. Therefore, you should never self-medicate. Alternative medicine can be used exclusively as complementary therapy and only after consultation with your doctor.
Basic preventive measures:
- Observe all rules of personal and intimate hygiene
- Rinse the intergluteal fold
- Wear loose, clean, eco-friendly clothing (avoid tight, tight, synthetic clothing)
- Avoid trauma to the coccyx area
- Avoid prolonged sitting
- Epilation and/or depilation in the tailbone area
- Promptly treat and sanitize primary holes, wounds and microtraumas in the coccyx area.
- Immediately contact a surgeon if the first signs of discomfort and inflammation appear
If clinical manifestations or relapse appear, then the only correct preventive measure will be surgical treatment.
Consequences and complications
The consequences of tumors and neoplasms of the spine greatly affect human health, because symptoms intensify due to the enlargement of the tumor itself. Liquid constantly accumulates, because of this the walls of the formation stretch, and the pressure inside increases. A tumor in the spine puts pressure on neighboring tissues and organs; nerve nodes and endings are especially affected by this.
A tumor in the spine puts pressure on neighboring tissues and organs.
Nerves die under pressure because the fluid necessary for functioning does not reach the cells. The skin becomes much less sensitive, the patient does not feel pain from this area and the effects of high and low temperatures. Anemia, loss of sensation, or seizures occur.
With late treatment, the formation of intervertebral hernias, bending of the vertebrae, or even displacement of the discs may occur. Inflammation or suppuration of these formations is possible, and there is a risk of sepsis.
With late treatment, the formation of intervertebral hernias may occur.
Such consequences lead to the death of a person, so prompt treatment and careful attention to health, all symptoms and complications are required. You must contact specialists and doctors immediately.
Causes
The reasons for the formation of spinal cysts are varied:
- For congenital spinal cysts, there are disturbances in the development of tissues in the fetus.
For acquired tumors:
- degenerative-dystrophic processes in the tissues of the spine,
- spinal injury (bruises, fractures),
- excessive, disproportionate loads on the motor segments (including those caused by the type of activity),
- a sedentary lifestyle, which leads to the development of dystrophic changes in the tissues of the spine,
- bleeding in the tissues of the spine,
- parasitic damage (for example, echinococcosis).
Diagnosis of spinal cysts
| euthman flickr |
Diagnosis of spinal cysts is a complex of measures, including:
- Collection of anamnesis and analysis of patient complaints.
- General clinical laboratory tests.
- Spinal examination.
- Palpation of the spine, which aims to characterize the severity of the pathological process, its localization and the presence of certain functional disorders.
- Imaging research methods:
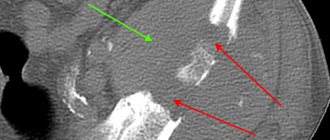
- CT;
- MRI;
- radiography;
- Ultrasound;
- myelography;
- electromyography and others.
Based on the data obtained, an accurate diagnosis can be made, the localization and intensity of the pathological process can be characterized.
How to treat the disease
Treatment of spinal cysts should be comprehensive; it can combine surgical and conservative methods of treating the tumor. Therapeutic methods for treating this pathology include:
- prescription of painkillers and anti-inflammatory drugs;
- prescription of various vitamins (for example, groups B and C, calcium, etc.);
- prescription of drugs to improve microcirculation, etc.
In addition, the attending physician may also prescribe physiotherapeutic procedures, namely:
- physical therapy;
- special massage;
- phonophoresis;
- reflexology.
If the size of the cyst increases, it is removed surgically.
Laparoscopy in the treatment of presacral cysts
A number of undoubted advantages of laparoscopic techniques, confirmed by numerous studies (reducing the trauma of surgical intervention, reducing intra- and postoperative complications, reducing the length of a patient’s stay in the hospital and the duration of temporary disability, reducing postoperative mortality) have made it possible to introduce them in various areas of surgery.
The rapid development of minimally invasive technologies in recent years and their priority use in the treatment of benign diseases of the colon (presacral cysts and tumors) forced us to take a fundamentally different approach to solving this problem.
What is the advantage of laparoscopic (through punctures on the abdominal wall) access:
- Minimal trauma, the operation is performed quickly and bloodlessly;
- The operation is performed without large incisions in the perineum, resection of the coccyx and removal of the stoma;
- In women, the natural process of pregnancy and childbirth is not disrupted, which becomes problematic with perineal access;
- The fastest possible rehabilitation period: get up and sit
the next day, discharge on the 3rd day (the possibility of vigorous activity remains); - Minimal risk of damage to the rectum, sphincter and development of cyst recurrence;
- The technique allows performing simultaneous (simultaneous) operations for various diseases of the abdominal and pelvic organs (uterus, appendages, gall bladder, etc.).
Rice. 1. Layout of the operating team and trocar insertion points.
Rice. 2. Giant presacral teratoma. Laparoscopic view.
Rice. 3. Final view of the sutured pelvic peritoneum. The anatomy of the pelvic organs has been completely restored.
Technique for removing presacral teratomas laparoscopically.
Surgery is performed under general anesthesia in the supine position. The layout of the operating team and the trocar insertion points are presented in the figure below.
During laparoscopy, the intestine is retracted to the left. In our work, we always use the Clermont-Feran uterine retractor, which allows us to clearly visualize the uterine space behind. Fixation of the uterus with a retractor in the ante-flexio position and traction of the rectum make it possible to obtain dosed tissue tension necessary for safe work in the pararectal space. The pelvic peritoneum is opened, exposing the upper pole of the cyst. If the cyst is large (7 cm or more), aspiration of the contents is advisable to obtain the necessary tissue tension. After evacuating the contents of the cyst with an electric suction, it becomes possible to traction it in all directions. This technique creates the tissue tension necessary for gentle dissection. Such tension cannot be created with a full cyst. To prevent injury to the intestinal wall, we insert a probe we developed with an expanding cuff into the rectum. We isolate the cyst walls from the surrounding tissues using a 5 mm LigaSure instrument connected to a computer-controlled electrosurgical unit - the Force Triad energy platform (Switzerland). This tool has no lateral heat spread. What is a reliable prevention of thermal injury to the intestine and, consequently, removal during intestinal stoma surgery. If the cyst is located very low, in the area of the levators or external portions of the rectal sphincter, then it is necessary to move apart the muscle fibers without crossing them, so as not to disrupt the function of the anorectal zone. It is necessary to identify the place of fixation of the cyst to the sacrum and, if possible, excise this area as much as possible - this is the basis for preventing tumor recurrence. If the cyst is complicated by suppuration and the formation of external perirectal fistulas, then at the same time we perform excision of the fistula to the wall of the cyst. The resulting cavity in the pelvic area is thoroughly washed, hemostasis is carried out and, if necessary, drained. The pelvic peritoneum is hermetically sutured with a continuous suture. After excision, the cyst is placed in a special plastic container and removed from the abdominal cavity through a trocar puncture. Cosmetic stitches are applied to the skin.
It should be noted that the laparoscopic approach should be used primarily to remove large teratomas or those located far from the perineum. In this situation, an alternative to laparoscopic is laparotomic access, which is more traumatic and has worse exposure to the surgical field.
What worries you about a coccyx cyst? Symptoms
If the coccyx cyst is not complicated or is in the “cold period” after inflammation, then in the vast majority of cases it does not manifest itself and is asymptomatic. From time to time there may be some discomfort in the coccyx area, serous discharge or moisture above and between the buttocks. Sometimes anal itching can be disturbing. Small points (retractions) of the skin in the area of the coccyx and intergluteal fold are visually determined.
When an infection enters the cavity, discomfort increases significantly, inflammation and pain occur in the area of the coccyx and sacrum. Primary openings (holes, fistulas) may appear from which serous, sanguineous or purulent discharge is released. With suppuration and abscess formation, secondary purulent fistulas can form.
In the absence or delay of discharge from the cyst, a painful infiltrate (swelling, edema, tumor, lump) appears through the holes with clear contours in the area of the coccyx and intergluteal fold, which interferes with movements and walking. When the contents of the cyst become infected, acute inflammation develops. Pain, swelling, and redness appear in the area of infiltration. Increased body temperature (fever). Abscess formation occurs (formation of a cavity with suppuration).
After the abscess of the coccyx cyst is drained independently or as a result of surgery (outflow of pus), relief occurs. Pain, swelling and redness disappear, inflammation subsides. The fistula gradually closes, and the postoperative incision wound heals. A period of imaginary well-being begins (the cold period). There is no point in waiting for a complete cure, since there remains a focus of dormant chronic infection (the substrate of chronic inflammation), which becomes aggravated or becomes re-inflamed under certain favorable conditions.
If radical surgery is not performed, then periods of exacerbations and remissions (the interval between exacerbations) can alternate for months and sometimes years. During remission, there is usually no edema or hyperemia. Periodic dull pain or discomfort in the tailbone area may be bothersome. Inconvenience occurs when sitting and in the presence of scanty discharge from holes or fistulas. Fistulas can function, open and close. With prolonged remission, pigmentation and scar tissue changes appear around the holes.
Therapy methods
How to treat tumors on the back is decided only by the doctor after a complete examination of the patient. As mentioned above, for small cysts, drug therapy is used, which includes taking medications:
- Anti-inflammatory drugs (NSAIDs).
- Relieving pain syndrome.
- Strengthening metabolism.
- Boosting immunity.
https://youtube.com/watch?v=ZePoCsTqUPE
Oral or topical agents in the form of ointments and gels can be used to relieve pain. The first ones, as a rule, are used when the patient has stomach diseases, for which it is undesirable to take a large number of medications. However, it should be noted that such drugs are less effective than drugs in tablet form. Therefore, people rarely use ointments for this pathology.
If medications do not help stop the growth of the tumor and the patient’s condition only worsens, surgery is prescribed. The cyst is completely excised, but before that the pathological contents are pumped out of it with a special syringe, which helps prevent infection of nearby tissues.
After the operation, the patient is prescribed strict bed rest, taking antibacterial and immunostimulating drugs. The duration of the rehabilitation period depends on the complexity of the operation and the size of the removed tumor. On average it takes 3 – 4 weeks.
Reasons for education
A spinal cyst manifests itself when bones begin to grow rapidly during adolescence.
Doctors divide vertebral cysts into congenital and acquired. The cause of the former, which occurs more rarely, is a violation of the formation of bone tissue of the embryo at the stage of its intrauterine development. Such pathologies are not diagnosed in the perinatal period; they usually begin to manifest themselves at the age of 14-17 years, when rapid growth of the musculoskeletal system begins.
Acquired cystic neoplasms are much more common. Their formation can be provoked by the following negative factors:
- Chronic overload of the spinal column.
- Injury to the vertebral bodies (bruises, dislocations, compression fractures).
- Hemorrhages caused by trauma.
- Dystrophic processes due to a sedentary lifestyle.
- Spinal tumors – both malignant and benign.
- Protrusion and herniation of intervertebral discs.
- Infectious pathologies of vertebral bone tissue (tuberculosis, osteomyelitis)
- Inflammatory processes against the background of arthropathy (osteoarthrosis, osteoporosis).
- Excess body weight.
Symptoms
A perineural cyst at the level of the s2 vertebra or in the neighborhood at the beginning of the disease shows almost nothing of itself. As the nerve structures grow, they are compressed, resulting in discomfort and sharp pain when exerting themselves. In addition, the patient may experience the following symptoms:
- Acute pain at the location of the cyst.
- Numbness in the lower extremities.
- The appearance of hypersensitivity of the epidermis in the area of localization.
- Frequent headaches, loss of consciousness or poor concentration.
- Malfunctions of the gastrointestinal tract.
- Problems with urination and bowel movements.
- Impotence and other sexual dysfunctions.
- "Goosebumps" and tingling in the legs.
A cyst up to 1.5 cm in size is discovered completely by accident in most people. But if this happens, the patient is scheduled for a scheduled examination and periodic examination in order to determine the dynamics of growth and gradual correction of treatment to obtain the desired result.
The clinical picture is more pronounced when the cyst grows in the area of the s2 and s3 vertebrae. But the signs of the disease are similar to other pathological processes, including damage to internal organs. Therefore, to confirm or refute the diagnosis, a full examination is prescribed. It allows you to identify the problem and choose adequate treatment.
Acute lower back pain is the first sign of the development of a cyst in the spine
Spinal cyst