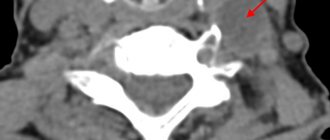
In practice, pediatricians have to deal with such a rare disease as osteochondropathy of the navicular bone of the foot. The pathology occurs in children and adolescents during the period of intensive formation of bone tissue. One of the reasons is impaired trophism of the growth zone. It begins with mild osteoporosis and gradually leads to deformation, microfractures, and complete destruction of the scaphoid bone against the background of simultaneous expansion of the joint spaces.
General information
Keller's disease is a disease that affects the bones of the foot. As a rule, it is diagnosed in adolescence and childhood. The development of this disease is expressed by osteochondropathy - a gradual process of destruction of bone tissue and its subsequent restoration.
This disease was first described by radiologist Keller from Germany; this happened at the beginning of the last century. When a person develops Keller's disease, the body experiences disruption of blood flow to the bones of the foot. As a result, the feet do not receive the required amount of oxygen and a number of nutrients necessary for the normal functioning of tissues. The process of bone tissue dying begins, which in medicine is commonly called aseptic necrosis . Death of foot tissue in Keller's disease occurs without the participation of infectious processes. Among the variety of ailments of the human skeletal system, osteochondropathy accounts for approximately 3%.
Causes
The disease manifests itself as a consequence of a number of reasons that lead to deterioration of blood circulation in the foot area. First of all, these are various foot injuries, constant wearing of tight and uncomfortable shoes of the wrong size. Keller's disease can develop in people suffering from arthritis , arthrosis , as well as some diseases associated with endocrine and hormonal disorders. Another important factor in this case is the hereditary predisposition to the development of this disease. Acquired or congenital foot defects (most often flat feet ) can also lead to the manifestation of this disease. An important factor is also the disruption of metabolic processes in the human body. However, experts note that the exact causes of osteochondropathy are still not completely known.
Forms of the disease
Doctors who diagnose Keller's disease define two types of disease, depending on which bones are affected.
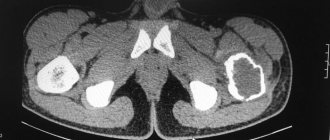
If a person is diagnosed with Keller's disease 1 , then we are talking about damage to the navicular bone of the foot. This bone is located at the inner edge of the foot. Keller's disease 2 is manifested by pathological changes in the heads of the second and third metatarsal bones of the foot. These bones are connected by articular surfaces to the phalanges of the fingers. Stage 2 Keller's disease most often develops in adolescents.
In addition, when determining the symptoms that manifest osteochondropathy, doctors divide the course of the disease into several stages. At the stage of necrosis, the patient’s bone beams, which are the structural elements of the bones, die. Such changes are clearly expressed, they can be seen even in the photo. At the stage of a compression fracture , new elements of bone tissue are formed, but now they do not yet have sufficient strength. During this period, bone beams often cannot withstand heavy loads. As a result, their fractures occur, and the beams can wedge into each other. This is followed by the fragmentation stage , in which osteoclasts (those cells that destroy bone) promote the resorption of bone beams. The final stage of the disease is the process of restoring the shape and structure of the bone. The answer to the question of how to treat a disease directly depends on what stage of the disease is currently occurring. Therefore, treatment of Keller's disease can only begin after a thorough professional diagnosis.
Effective and safe treatment
A plaster cast does not help stop the destructive process in the bone.
Conservative therapy for osteochondropathy of the scaphoid gives a positive result. It is carried out at all stages. Surgeons must prescribe foot immobilization in children for a period of 1 month. A plaster cast is applied to a height of up to 1/3 of the tibia, even if there is no history of a fracture of the scaphoid element. The main goal is to ensure maximum peace and stop destruction. A scaphoid fracture complicated by opposing fragments is treated surgically.
The lack of effect from conservative measures, as well as unbearable pain, is an indication for surgery. During revascularization osteoperforation, additional channels are created through which new capillaries begin to grow. Trophism is significantly improved and the bone structure is regenerated. Good results for osteochondropathy are achieved by:
- physiotherapy;
- electrophoresis with nicotinic acid and analgesics;
- ultrasound;
- darsonvalization;
- phonophoresis;
- laser therapy;
- thermal procedures.
For rapid regeneration, normalization of blood circulation and metabolic processes, young patients are prescribed medications presented in the table:
Medications
| Group | Action provided | Example |
| NSAIDs | Reduce inflammation, relieve pain | "Nurofen" |
| "Ibuprofen" | ||
| "Nise" | ||
| Chondroprotectors | Restore osteochondral tissue | "Don" |
| "Arthra" | ||
| "Rumalon" | ||
| Antiplatelet agents | Normalize blood flow and clotting | "Dipyridamole" |
| "Pentoxifylline" | ||
| "Heparin" | ||
| Angioprotectors | Strengthens the vascular wall | "Etamzilat" |
| "Dicynon" | ||
| "Solcoseryl" | ||
| Analgesics | Eliminate pain | "Paracetamol" |
| "Calpol" | ||
| Vitamins | Activate metabolic processes | "Folic acid" |
| "Vitamin B2" | ||
| "Vitamin E" |
Symptoms
Keller's disease I is most often diagnosed in preschool boys aged 3 to 7 years. Initially, the child notices pain and signs of swelling on the back of the inner edge of the foot. Due to the pain, there is a constant limp in the child, who tries to lean on the opposite, outer part of the foot while walking. Typically, the disease affects only one foot. It lasts about a year, after which the pain gradually stops.
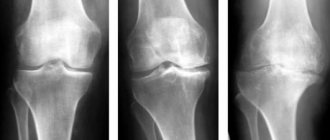
Keller II disease is most often diagnosed in teenage girls. It was first described by traumatologist Freiberg from the USA, and Keller studied this type of disease in more detail and gave its description. This form of the disease is often bilateral. As a rule, the onset of the disease goes unnoticed. Initially, pain develops in the area of the head of the II or III metatarsal bones. They immediately appear in cases where a load is placed on the forefoot, and later the patient feels pain even at rest. The appearance of lameness is gradually noted, the patient cannot walk in shoes with thin soles, it is very difficult for him to walk barefoot, especially if the surface is uneven. Where the pathological process develops - on the dorsum of the foot - swelling appears. The finger that is located next to the head of the affected bone becomes shorter, and movements in the joint are limited. All these symptoms are present in the patient for about two years, after which the pain gradually begins to subside. However, if changes have occurred in the joint during this period, the pain may soon reappear. Sometimes familial cases of foot involvement are diagnosed. Most often, the disease is localized at the head of the second or third metatarsal bones, but damage to several bones rarely occurs.
Accessory navicular bone
Early postoperative period
Almost all patients after surgery for Achilles tendon ruptures are discharged from the clinic on the day of surgery.
For two weeks after surgery, the ankle joint will be fixed with a plaster or polymer rigid bandage, similar to the one shown in the photo below.
Do not remove the cast until the next dressing change, which will take place 2 weeks after surgery.
You should not put any weight on your limb for 2 weeks after surgery. Before you are discharged home, you will be advised by a physiotherapist, who will include: will tell you how to use crutches correctly.
In the first 2 weeks after surgery, try to elevate your foot and keep it in that position 95% of the time.
Elevated foot position
Most people certainly don't have a functional bed at home like the one in this photo. However, the same effect can be achieved on a regular bed or sofa by placing a pillow under your foot. You should not put your feet in an elevated position when you are sitting on a chair. And once again we advise you to stay at home for the first two weeks.
To minimize the risk of infection, keep your feet dry and cool. Avoid excess humidity and heat. When showering, wear a sealed bag over your foot.
In order to prevent venous thrombosis, regularly perform movements in the foot and ankle joint. Drink enough fluids. If you have risk factors for thrombosis, be sure to tell your doctor about this; if necessary, he can prescribe you anticoagulants.
Two weeks after surgery
You will be examined by your doctor and your dressing will be changed. If the wounds have completely healed, then we will tell you how to properly massage the tissues in the intervention area. Measures aimed at reducing the sensitivity of the scar begin only after the wound has completely healed. For this purpose, you can use a massage cream (for example, E45), which should be rubbed into the scar area and around it. You can expose the surgical area to moisture and take a shower only after the wounds have completely healed.
At this stage, if post-operative swelling has largely subsided, we will allow you to lower your foot down more often, but recommend that you still keep it horizontal most of the time if possible.
You will be allowed to drive for a short time, but only if your left leg has been operated on and your car has an automatic transmission. If the right leg has been operated on, we recommend driving no earlier than 6-8 weeks after the operation.
At this point, you may be referred to physical therapy to begin early rehabilitation and exercises to strengthen your tibialis posterior muscle.
Six weeks after surgery
If the healing process is going well, by this time your swelling and bleeding will have largely disappeared, but some swelling may persist for up to 3-4 months after surgery.
You will be able to wear regular shoes (if swelling allows), but we recommend wearing hard-soled shoes for now. Over the next 3-6 months, you will undergo physical therapy classes, which will allow you to achieve the most optimal result of the surgical intervention.
Three months after surgery
If you are satisfied with the result, then this is your last visit to the doctor.
Prevention
To ensure the right approach to prevention and prevent the development of both forms of Keller's disease, parents must, first of all, ensure that children always wear only comfortable and appropriately sized shoes. It is also important to reduce the mechanical load on the feet. To ensure that this condition is met, serious physical activity should not be allowed in preschool children. If you receive any foot injury, you must consult a doctor and undergo the tests prescribed by him. It is also important to pay attention to the presence of foot deformities and be sure to consult a specialist about this.
Measures to prevent osteochondropathy of the navicular bone of the foot
After removing the plaster cast for osteochondropathy, children are recommended to use special insoles with reduced pressure on the scaphoid bone. This relieves pain and promotes faster recovery. Orthopedic shoes retain their correct shape and are effective during the rehabilitation period. Children are prohibited from running and jumping for 2 months to avoid the appearance of a false joint or fissure. For any injury to the foot and ankle, be sure to contact a traumatologist. Correct adherence to recommendations and high-quality implementation of techniques leads to complete recovery. Lack of treatment causes severe flat feet, osteoarthritis, contracture and deformation of the foot bones.
List of sources
- Traumatology and orthopedics / Guide for doctors: In 3 volumes T.Z / Ed. SOUTH. Shaposhnikova. -M.: Medicine, 1997.
- Movshovich I.A. Operative orthopedics. M.: Medicine. 1994;
- Sorokin, S.A. Diagnosis of the second Köhler disease / S.A. Sorokin // Restorative treatment of children with diseases and injuries of the musculoskeletal system: collection. scientific tr. / ed. B.L. Andrianova. - St. Petersburg, 1991.
- Traumatology and orthopedics. Multi-volume guide for doctors. Ed. N.V. Kornilov. SPb.: Hippocrates. 2006; III;
- Varshavsky G.I. On the differential diagnosis of Keller II disease / G.I. Varshavsky, I.M. Varshavsky // Annals of Traumatology and Orthopedics. 1994. -№2;