Arthrosis is to blame
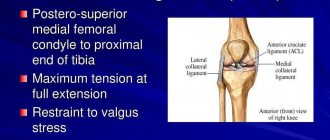
Joint pathology occurs due to deformation of the cartilage that protects the bones from friction and shock. In the first stages of their destruction, the pain is weak and occurs only occasionally, after prolonged rest or, conversely, walking and standing. But as arthrosis develops, they intensify and become permanent.
The movement of the knee joint is limited, and a crunching sound may be heard when flexing and extending.
Arthrosis is characterized by severe joint pain at the end of the day or in the first half of the night, as well as after intense physical activity.
If arthrosis appears on the right leg, then it will soon reach the left. At risk:
- professional athletes and dancers;
- movers;
- people over 40 years old;
- overweight;
- after a knee injury;
- with endocrine diseases and metabolic disorders;
- with a deficiency of microelements necessary for skeletal nutrition;
- regularly exposed to hypothermia;
- systemic exposure to toxic substances.
Over time, the soft tissue around the joint also becomes inflamed. This is why knee pain can also be felt below the knee bend on the back side. The diagnosis is determined by the results of visual tests to assess the patient's condition and X-ray images.
[media=
https://youtu.be/Io186k5vMkE
]
Diagnostic measures
Diagnosis of pathology begins with an examination and study of the medical history. The doctor clarifies the nature and type of pain, its localization, studies hereditary factors and the patient’s professional activity. Next, the doctor prescribes laboratory tests of blood and urine to determine the general condition of the patient and identify the inflammatory process. Then instrumental diagnostics are carried out:
- Ultrasound of the knee joint;
- X-rays using contrast to exclude the development of arthritis;
- MRI of the knee to identify neoplasms and meniscal pathology;
- Doppler;
- Arthroscopy of the composition;
- Puncture.
Diagnosis of pathology must be comprehensive. During the examination, the doctor must determine the cause of the disease in order to correctly develop treatment tactics.
Signs of a cyst
Advertising:
Pain behind the knee - what is it? Among the possible answers to the question you can find the following - cyst. A pathological cavity may appear in the popliteal fossa.
Revision arthroplasty involves replacing the hip joint. Often such an operation is performed due to its wear and tear or illness; the disability group and quota after replacing 1 joint are not allowed. Read more in the article: “rehabilitation after hip replacement at home.”
Its provocateur is usually an inflammatory process in the synovial membrane. The latter produces a lubricating fluid, protects the inner surface of the joint, provides cartilage tissue with useful substances and protects it from impact as a natural shock absorber.
If the synovial membrane becomes inflamed, it begins to produce excess fluid. They accumulate on the back wall of the joint capsule and put pressure on the membrane. This fact explains why pain appears in the posterior popliteal region.
A cyst that forms in the knee joint is a symptom of a complex, primary illness.
A cyst can be identified by the following signs:
- Examine visually, especially on an extended leg. If the cyst has grown in the meniscus, then it is impossible to see or even feel it.
- Joint mobility is impaired.
- When moving, severe pain is felt, which radiates from the back of the popliteal region.
- Swelling appears.
X-ray diagnostics is used to determine the disease.
Ear pain on one side can be a symptom of dangerous diseases such as otitis media or mastoiditis. Timely treatment prevents the development of these ailments and the occurrence of possible complications. Read more in the article: “how to treat a sore ear.”
Description and symptoms of pathologies of the articular zone of the musculoskeletal system
Prolonged manifestations of pain are the reason for an MRI of the hip joint. The bone joint itself is not penetrated by nerve fibers, so some diseases can be asymptomatic for a long time. Soreness appears at the stage of damage or compression of the nerve canals passing in the “hinge” region of the body. At the initial stage of the appearance of disorders, unpleasant sensations arise in a limited area of the connection of the femur with the pelvis. If the disease is ignored, the source of inflammation grows and spreads to neighboring tissues: muscle and tendon fibers, cartilage formations, nerve and blood tracts.
A person may experience the following sensations:
- prolonged radiating pain that does not go away within several days, the cause of which can be identified on an MRI of the hip joint;
- night pain leading to insomnia;
- the desire to change positions as often as possible in order to relieve the pelvic joint with constant discomfort in it.
These signs serve as a reason for a thorough diagnosis, and emergency clinical care is required if the patient complains of the following conditions:
- Irradiation to the groin. Through the conductive canal of the nerve, pulsating sensations spread to the lower abdomen and groin area; with inflammation of adjacent fibers, the sciatic nerve is affected.
- Shootings in the lower part of the back. They can be both sharp and dull, pulsating, leading to limited movement of the body and pelvis.
- Spread of pain to the leg, including the knee area. It may manifest itself as muscle weakness or itchy sensations in the skin.
- A “hinge” clutch that prevents free movement of the limb. It is a sign of arthritic and arthrosis lesions.
- Partial or complete lack of mobility associated with the destruction of pelvic tissues or trauma experienced.
- Lameness associated with low intensity pain. It requires correction, since a change in motor habit leads to deformation of the entire musculoskeletal system.
Most patients describe the phenomenon of crunching sounds when changing body position or movement. A kind of crunching sound is produced by individual ligaments. If the sound is not accompanied by unpleasant sensations, there is no need to worry. Additional pain requires contacting a medical specialist.
Tendon inflammation
Advertising:
One of the most common tendon diseases is bursitis. All joints are subject to inflammation of the mucous bursae, the knee is no exception. First, a soft swelling appears, which hurts and radiates to the back of the knee.
The development of bursitis is promoted by:
- mechanical irritations (pressure and friction);
- injuries;
- complications after infectious diseases (tonsillitis, brucellosis, gonorrhea, tuberculosis, etc.).
The chronic course of the disease can be replaced by exacerbations, which are replaced by temporary improvement.
[media=
https://youtu.be/pv3yiOOmZRs
]
Meniscus tear
The meniscus consists of cartilage tissue and acts as a shock absorber and stabilizer of the knee joint. It is easily damaged, but it will not be possible to understand immediately that this happened.
A knee meniscus injury causes the following symptoms:
- sharp pain that spreads to the entire knee and nearby tissues;
- clicking sound when bending;
- noticeable swelling and heating of the joint;
- atony of surrounding muscles.
If the tear is strong, then the flexion-extension function of the knee is impaired. The disease is diagnosed by X-rays, MRI, ultrasound and endoscopic arthroscopy.
Hemarthrosis as a result of trauma
The knee joint is the most vulnerable to hemarthrosis. Its occurrence is facilitated by:
Advertising:
- knee bruises after a fall or blow;
- ligament and meniscus tears;
- intra-articular fractures;
- knee surgery.
Under the influence of injury, blood leaks into the joint cavity. It accumulates here, increasing the size of the joint.
If the patient is not hospitalized and the fluid is not pumped out, then there is a possibility of developing purulent inflammation.
After damage, the joint begins to ache and swell. For a long time his movement was limited. The specialist draws conclusions based on the victim’s complaints, examination, MRI and ultrasound.
About traditional methods of treatment
Many people prefer to treat knee numbness on their own. They have a large arsenal of natural medicines at their disposal to help cope with the symptom. However, you should be sure that due to the individual characteristics of each person, the use of such drugs may have negative effects. So:
- Pumpkin compress. Place the peeled and coarsely grated pumpkin in gauze and apply it to your knees. You can dilute the paste a little with warm milk. A similar method for preparing an onion compress. Fresh scratches and abrasions on the skin are not allowed.
- Honey applications. Apply warm honey to your knees, cover with plastic wrap and wrap. Keep this application for half an hour, then rinse with warm water. It is recommended to add rye flour, chicken egg yolk, and a few drops of olive oil to honey.
- Rubbing from bogulnik. Pour the crushed plant with alcohol (1:3) and let it brew in a dark place for a week. Rub into numb knees three times a day.
- Oil rubbing. Mix 100 g of ground black pepper with a liter of any vegetable oil. Boil the product over low heat for half an hour and cool. The irritating baking effect is alleviated by oil components, but at the same time, it activates blood supply processes.
- Compress based on lilac. Place the flowers in a glass, pour half a liter of alcohol (or vodka) and place in a dark place for two weeks. The course of using this compress is 10 days. A tincture for compresses from Kalanchoe leaves is prepared in the same way.
- Black radish tincture. Pour one and a half glasses of juice into 0.5 glasses of vodka. Add a tablespoon of salt and half a glass of honey. Rub on sore knees at night. Sometimes it is recommended to take this composition internally. Then its dosage is 30 ml per dose three times a day.
Most popular recipes
- Burdock and elecampane root baths. Pour boiling water (1 liter) over the crushed mixture of herbs. Leave for a couple of hours and use for baths daily.
- Ointment based on bay leaf. Mix 6 parts of chopped bay leaves with 1 part of juniper needles. Add 12 parts of any fat to the mixture. Grind and leave for a couple of hours. After preparation, rub into the mixture with circular massaging movements.
- Camphor ointment. You can buy it at the pharmacy or prepare it yourself. Mix 100 g of alcohol with 50 g of camphor. Add the same amount of dry mustard and two egg whites. Mix everything thoroughly and start rubbing. Condition: no allergy to any of the components used.
- Blueberry applications. Crush ripe blueberries, collect the pulp in gauze and apply to your knees at the end of the working day. The product has a good anti-inflammatory, soothing, vitaminizing effect on the skin and subcutaneous layers.
You can prepare the medicine for oral administration:
Garlic drink. Squeeze the juice from three large heads. Pour it into a half-liter jar and top up with water. Leave in a dark place for a week, shaking occasionally. Take a tablespoon, you can wash it down or first dilute it in a third of a glass of water.
For the treatment of numbness of the knees of vascular etiology, it is recommended:
- Drops based on beets, cranberries, black radish. Mix the components in equal quantities and add alcohol. Leave for two weeks in a dark, ventilated place, then strain and take 30 ml half an hour before your morning meal.
- Lemon tincture with added garlic. Squeeze the juice from 4 lemons and 4 heads of young garlic. Pour two liters of water and close the lid. It must stand for at least three days. Take half a glass daily, preferably in the middle of the day. The product is good at cleaning blood vessels from cholesterol plaques and preventing atherosclerosis.
Neurovascular diseases
The cause of pain under the knee can be various diseases of the nervous and vascular systems. Their full symptoms are reflected in detail in the table.
| No. | Name of the disease | Features, reason | Symptoms |
| 1. | Inflammation of the tibial nerve | The tibial nerve continues the sciatic nerve, starting at the popliteal fossa and passing along the back of the popliteus muscle. The disease can be triggered by injury, excessive pressure or inflammation. | The muscles atrophy and lose sensitivity. The patient cannot straighten the foot and toes, or rise onto the toes. Originating behind the knee, the pain radiates to the foot. On examination, changes in reflexes are observed. |
| 2. | Thrombosis of the popliteal vein. | Blood clots form in it, which disrupt free blood circulation. | Aching pain appears in the posterior popliteal region. |
| 3. | Popliteal artery aneurysm | Due to thinning or stretching of the artery, its lumen may increase several times. | The affected areas are characterized by nagging pain, including under the knee |
Pathologies are often confused with other diseases. X-rays, MRIs, vascular scans and electrodiagnostics are used to determine diagnoses.
Benefits of osteopathy in treating knee pain
- Gentle techniques that do not cause increased pain.
- In many cases, osteopathy helps to cope with the disease without surgery.
- Only an osteopath in case of leg diseases will help restore the balance of the body and remove secondary dysfunctions.
- After surgery, osteopathy helps speed up the recovery process.
- We conduct a full examination of all patients, regardless of symptoms, as well as complete correction of all significant dysfunctions of the body, since everything in our body is interconnected!
Purulent-inflammatory processes
The likelihood of purulent-inflammatory processes in the knee area increases with wound infection. If it is not disinfected in time, there is a danger of developing an abscess of the popliteal fossa.
Advertising:
The situation is complicated by the fact that the lymph nodes are located here. If pathogens from the wound penetrate here, lymphadenitis will most likely develop.
This dangerous disease is difficult to diagnose, since the lymph nodes are located deep in the tissues. When diagnosing, specialists use the following symptoms:
- external swelling;
- hyperemia;
- pain when pressing;
- joint enlargement;
- fever.
After the examination, laboratory and radiographic examinations are prescribed.
Which doctor should I contact if my leg muscles are numb?
Various specialists can deal with the correction of numbness: a neurologist, a vertebroneurologist, a vascular surgeon, a chiropractor, a rheumatologist and other doctors, depending on the profile of the disease.
It is enough to inform the administrator of the Center for Progressive Medicine “Doctor Pozvonkov” about the problem, he will select a specialist for initial treatment. His consultation will help you begin to solve the problem. In the future, the necessary examinations will be prescribed; it may be necessary to examine doctors of related specialties.
It is convenient to make an appointment using the feedback form.
How to avoid problems with knee joints?
Treatment of any of the above diseases is a long process, not always favorable. To avoid it, you need to take care of your knees from a young age. Prevention means are:
Advertising:
- wearing special protection during training and competitions;
- warming up the muscles before starting sports activities using a warm-up or warming gels;
- avoiding hypothermia and excessive weights;
- proper nutrition with sufficient amounts of microelements;
- organization of drinking regime;
- fight against extra pounds, which increase the load on the joints;
- swimming, therapeutic exercises, cycling and walking;
- hardening the knee joint with cold water.
If for any reason pain does occur, you can relieve the discomfort with painkillers, anti-inflammatory ointments and an elastic bandage. Such measures are appropriate only initially, but require subsequent examination.
What are the treatment approaches?
The order of therapeutic prescriptions depends on the cause of the disease, the presence of concomitant pathologies, characteristics of the development process and the patient’s life history.
If the symptom of knee numbness is functional in nature, it may be worth changing your working conditions, rest habits, hobbies, and lifestyle. It is necessary to exclude factors that contribute to delayed blood supply and uneven innervation.
A symptom that is a sign of a disease will not go away on its own. Its manifestation is the result of the physiological inability of the knee joint to perform its functions. Therefore, the main focus is on treating the primary disease.
Along with targeted medications (anti-inflammatory, muscle relaxants, neuroprotectors, atherosclerotic, anticoagulants, statins and others), doctors recommend taking physiotherapeutic procedures, as well as:
- follow a diet rich in vitamins and microelements;
- develop a scheme of physical activity on the legs and practice according to it with a gradual increase in strength;
- avoid hypothermia;
- take contrast baths and shower procedures;
- do not drink alcohol and stop smoking;
- Limit your consumption of coffee, carbonated drinks and foods prepared with artificial flavor enhancers.