The shoulder area is known to be one of the most difficult to evaluate and rehabilitate. Because of the numerous joints involved during shoulder movement, it is useful to use the term “shoulder complex.” Effective rehabilitation of shoulder injuries requires knowledge of the functional anatomy that underlies the biomechanics of the shoulder complex.
Anatomy
The shoulder complex includes 3 physiological joints and one “floating” joint:
- The glenohumeral joint (HSJ).
- Acromoclavicular joint (ACJ).
- The sternoclavicular joint (SJJ).
- Scapulothoracic joint (SJJ).
When assessing the glenohumeral joint, you also need to consider the contribution of the sternocostal and costovertebral joints.
The GCL is the only place of attachment of the upper limb to the axial skeleton. LGS involves a sliding movement of the scapula along the chest and does not provide for bony attachment. The PLS is of particular interest in understanding the mechanism of injury to the shoulder joint because it is osteologically predisposed to instability.
How to prevent shoulder pain
To prevent pain from occurring, the following conditions must be observed:
- lead an active lifestyle, move more, engage in feasible sports;
- Avoid prolonged periods with your arms raised above your head, as well as movements associated with unilateral load on the shoulder joint; At risk are weightlifters, tennis players, and miners; If a representative of one of these groups feels persistent pain in the shoulder, perhaps he should change his occupation or at least reduce his exposure to harmful factors as much as possible.
Biomechanics
Shoulder joint
Shoulder joint
Osteokinematics:
- Flexion/extension.
- Abduction/adduction.
- Internal/external rotation.
Arthrokinematics:
- Rotation (during flexion and extension).
- Downward sliding (during abduction).
- Sliding upward (during adduction).
- Posterior sliding (with internal rotation).
- Anterior sliding (with external rotation).
The natural arthrokinematics of the PLC during movement under conditions of an open kinematic chain involves multidirectional sliding of the humeral head within the glenoid fossa.
Del Maso and colleagues estimated that during movement of the upper extremity, the humeral head can move upward by 7.5 mm, which is quite large for such a bony structure located in such a compact space. Smooth movement of the humeral head requires well-coordinated work of the rotator cuff muscles. Abnormal/excessive movement of the shoulder is associated with pathology of the shoulder complex and has been suggested to be a contributing factor to pain and discomfort in the LCL and may also cause damage to surrounding structures.
If we analyze the force vectors and moment levers, it becomes clear that during movements, the rotator cuff tendon holds the head of the humerus within the glenoid fossa. For example, the supraspinatus muscle initiates abduction of the arm by pulling the head of the humerus toward the glenoid cavity, thereby providing a fulcrum for movement.
Each rotator cuff tendon limits the movement of the humeral head in certain directions. The supraspinatus helps prevent excessive superior translation, the infraspinatus and teres minor limit excessive superior and posterior translation, and the subscapularis controls excessive anterior and superior translation of the head, respectively.
An imbalance in the activation of any of these muscles can easily cause the humeral head to become dislocated, resulting in impingement of the subacromial structures during movement. Both superior and anterior translation of the head are the leading biomechanical causes of shoulder impingement syndrome.
AC joint
AC joint
The AC joint is a synovial joint that allows axial rotation and anteroposterior glide. Since there are no direct muscle attachments to the joint, all movements are passive and initiated by movements in other joints (such as the scapulothoracic joint).
Osteokinematics:
- Flexion/extension.
- Abduction/adduction.
- Internal/external rotation.
Arthrokinematics:
- Forward/backward rotation.
- Under/over rotation.
- Front/back sliding.
Sternoclavicular joint
Sternoclavicular joint
As mentioned above, the GCL is the only joint through which the upper limb is attached to the axial skeleton. The RCL is classified as a low-moving, flat-type joint that has a fibrocartilaginous articular disc. The ligamentous apparatus of this joint is so strong that the collarbone is more likely to break than the joint itself to dislocate.
The GKS has 3 degrees of movement:
- Elevation/depression.
- Protraction/retraction.
- Axial rotation.
There are no muscles that directly act on the sternoclavicular joint. However, the movements of the joint closely mimic those of the scapula.
Scapulothoracic joint
Scapulothoracic joint
Movements in the scapular-thoracic complex:
- Lift and protraction = anterior lift.
- Elevation and retraction = posterior elevation.
- Depression and protraction = anterior descent.
- Depression and retraction = posterior descent.
The movement of the scapula along the rib cage directly affects the biomechanics of the shoulder complex as a whole and, in addition, may predispose to the occurrence of impingement syndrome. Normal motion of the scapula relative to the rib cage during arm elevation includes protraction, posterior tilt, and external rotation (depending on the plane of motion).
Although posterior tilt is commonly understood as movement at the acromioclavicular joint, scapular tilt during arm elevation is critical to minimizing pressure on the soft tissue underlying the acromial arch. The contribution of the LGS is usually expressed as the ratio of the movement of the LGS to the movement in the PLS. The glenohumeral rhythm is quantified by dividing the total amount of shoulder elevation by the amount of superior rotation of the scapula. In the scientific literature, it is generally accepted that the glenohumeral rhythm is 2:1, which corresponds to 2° of elevation of the humerus for every degree of upward rotation of the scapula.
The stability of the LGS depends on the coordinated activity of 18 muscles that directly attach to the scapula. These muscles must dynamically control the position of the socket so that the head of the humerus remains centered and allows movement of the arm.
When weakness or neuromuscular dysfunction of the scapular muscles is present, the arthrokinematics of the scapular scapula is altered, ultimately predisposing the individual to injury to the scapula.
Pathological kinematics of the LGS joint includes the following problems (but is not limited to):
- Increased internal rotation.
- Reduced superior rotation.
- Reduced rear tilt.
These changes in mobility are thought to increase the proximity of the rotator cuff tendons to the coracoacromial arch or labrum. However, there is still controversy regarding exactly which deviations in the trajectory of movement contribute to the reduction of the subacromial space.
For clarification purposes, current literature distinguishes between internal and external impingement. Impingement that involves a reduced space toward the coracoacromial arch is considered external impingement, while internal impingement involves involvement of the labrum and may be associated with PLC instability. Regardless of classification, dysfunctional shoulder mechanisms may contribute to rotator cuff deterioration and should therefore be understood as neuromuscular disorders.
Neuromuscular control of the scapula is based on the balanced action of the global muscles and the local muscles that stabilize the shoulder joint. We can therefore state that the shoulder complex is one of the most kinematically complex areas of the human body and requires a high level of neuromuscular control and proprioception throughout the movement.
Movement of the thoracic spine
When bending the right arm, the upper thoracic vertebrae tilt and rotate to the right, as well as extend. The 1st and 2nd ribs descend, while the 4th, 5th and 6th ribs rise, and the 3rd functions as an axis.
Restriction of movement in any of these structures will negatively affect the biomechanics of the shoulder girdle and may cause or predispose the shoulder to pathological changes.
What to do at home if your shoulder hurts
If you suddenly experience severe pain, you must first of all calm down and make the right decision: seek medical help.
You should know: any acute diseases, including those accompanied by severe pain, are easier to treat and are often completely cured. Therefore, the sooner you see a doctor, the more favorable the outcome of the disease will be.
But there are situations in life when it is not possible to immediately visit a doctor. What to do if shoulder pain does not improve? The advice is still the same: consult a doctor, he will help even in advanced conditions: he will relieve pain and stop the progression of the disease.
How to help yourself
The pain can be very severe and then the question arises, how to help yourself, how to survive this condition and get to a specialist? You can call an ambulance or help yourself:
- Take painkillers:
- Ibuprofen
- quickly and effectively relieves pain, swelling and fever; if there are no contraindications for use, you can take 1 – 2 tablets of 200 mg, washed down with half a glass of water (this will make the drug work faster); contraindications: erosive and ulcerative diseases of the gastrointestinal tract (GIT), increased bleeding; - Paracetamol (Panadon, Efferalgan)
is also an effective drug in sufficient dosage; To eliminate pain, take 1 tablet of 500 mg; There are practically no contraindications; - Ibuklin
is a combination drug; 1 tablet for adults contains 400 mg of ibuprofen and 325 mg of paracetamol; It acts quickly and effectively, but has the same contraindications as Ibuprofen. - Use external agents - gels, ointments. They can relieve pain well, especially in combination with painkillers or injections:
- Diclofenac gel (Voltaren, Diclovit, Ortofen)
– applied in a thin layer to the painful area; very effective ointment; - Ketoprofen gel (Artrum, Bystrumgel)
- after application to the skin, the ointment for shoulder pain is quickly absorbed and has an analgesic effect; - Menovazin
is an alcohol combination solution that contains painkillers and sedatives.
Carrying out pain relief on your own is a necessary measure and it does not in any way cancel a visit to the doctor!
Exercise can help too. Training is carried out after the acute pain has been eliminated. Regular exercise helps improve blood circulation and metabolism in affected tissues, and prevents the development of irreversible changes that block the motor activity of the hand.
Basic training requirements:
- regularity – classes should be held daily;
- lack of heavy physical activity and sudden movements;
- all exercises must be performed smoothly;
- if there is a sharp increase in pain, stop training; exercises are continued after the intensity of the pain syndrome has decreased with lower loads, increasing them very gradually.
Several exercises designed specifically for patients with glenohumeral pain syndrome:
- Starting position (IP) – lying on your back, arms along the body, palms up, legs slightly apart. Inhale: raise your hands and place them behind your head; exhale: smooth return to IP.
- IP - lying on your back, arms outstretched to the sides. Inhale: without lifting your hands from the surface, make a sliding upward movement. Exhale - return to IP. Repeat the exercise moving down and back.
- IP - lying on your stomach, arms extended forward, legs spread. Inhale: raise your right arm and left leg, exhale - move to IP. Repeat the exercise with your left arm and right leg.
Exercises for shoulder pain
What not to do
In case of chronic pain syndrome in the glenohumeral region, the following is contraindicated:
- some hand movements - which ones are determined by the doctor after clinical tests and additional examinations; it all depends on which structures are affected;
- any sudden hand movements and heavy lifting;
- frequent smoking and alcohol abuse - has a negative effect on blood circulation and metabolism, which aggravates the problems;
- self-medication - the result will be impaired hand function and increased pain; treatment must be carried out at a professional level.
When you need to see a doctor urgently
A doctor’s consultation is required if there is pain in the glenohumeral region:
- appeared immediately or some time after the injury; they intensify when the hand moves in a certain direction;
- the shoulder hurt against the background of existing chronic arthritis affecting other joints;
- accompanied by fever, redness, swelling and pain in the shoulder area;
- appeared against the background of cervical osteochondrosis with painful lumbago in the neck, extending to the glenohumeral region;
- discomfort, crunching when moving and occasional minor pain have been bothering me for more than 3 months.
Self-medication for such diseases almost always ends in the development of persistent pain and impaired movement in the hand. You will be provided with qualified assistance at the Moscow Medical Center.
Static structures and mechanoreceptors
Friends, Georgy Temichev’s seminar “Diagnostics and treatment of problems of the glenohumeral complex” will take place very soon. Find out more...
The static structures of the shoulder complex, including the labrum, capsule, articular cartilage, ligaments, and fascia, collectively act as physical restraints and have a stabilizing effect on the humeral head.
In addition to their passive stabilizing role, they also provide additional protection through various mechanoreceptors embedded in their fibers. Mechanoreceptors can be understood as neural sensors that provide afferent input to the central nervous system for motor processing and the generation of descending motor commands necessary to perform movements.
Mechanoreceptors are characterized by their specialized nerve endings that are sensitive to mechanical tissue deformations and therefore contribute to the modulation of motor responses of local muscles.
Muscle spindles and Golgi tendon organs, as well as Ruffini, Pacini, Meissner, Merkel corpuscles and free nerve endings are responsible for our sense of touch and proprioceptive positioning. They provide feedback regarding muscle length, tension, orientation, speed and force of contraction.
Thus, the passive structures of the shoulder provide mechanical protection and, through a neurological feedforward and feedback mechanism, directly influence the stabilizing function of the shoulder musculature.
Shoulder Pain Treatment
Treatment of shoulder pain should be carried out strictly individually, taking into account examination data and the established diagnosis. It is performed by an orthopedist-traumatologist or rheumatologist. In case of very severe pain, pain therapy is carried out by an anesthesiologist-resuscitator. A specialist will always find something to treat even very severe shoulder pain.
Diagnostics
A correct diagnosis is the path to prescribing adequate treatment and relieving the patient of pain. In diagnosis, examination and clinical examination of the patient by the attending physician using special assessment tests is of particular importance. They allow you to preliminarily determine which structures were damaged. The location of the damage is determined in more detail using functional tests.
Clinical data are confirmed by laboratory and instrumental studies that reveal inflammatory reactions, the presence or absence of infectious, autoallergic processes, the degree of destruction of articular and periarticular tissues. In identifying tendonitis and capsulitis, the main instrumental diagnostic methods are ultrasound and MRI.
How to treat shoulder pain
Treatment for shoulder pain begins with limiting the load on the affected limb. The patient is allowed movements that he can perform painlessly. Immobilization of the limb (scarf bandage) is carried out in short courses if the severity of the pain syndrome is very great. Prolonged immobilization contributes to the consolidation of hand dysfunction. Today, for partial gentle immobilization, taping is often used - fixing muscles with adhesive tapes in a certain position to prevent injury. This significantly improves the quality of conservative therapy.
After acute pain in the shoulder has been eliminated, treatment is continued by prescribing courses of physical therapy (physical therapy) and massage. At any stage of the disease, conservative therapy includes physiotherapy and reflexology courses. In case of severe pain, this is electrophoresis with novocaine, then warming procedures, mud and baths.
At the same time, drug therapy is prescribed. We remove pain by prescribing drugs from the NSAID group in tablets, injections, ointments (the drug with the best analgesic properties is Ketorol). For very severe shoulder pain, treatment includes narcotic painkillers (Tramadol) and glucocorticosteroids (GCS - Betamethosone). Sometimes folk remedies are also used.
To restore cartilage, chondroprotectors (Dona, Artra, Structum) are prescribed. Drugs in this group also help restore damaged periarticular tissues - tendons and ligaments, since they have the same origin as cartilage cells.
Surgical assistance will be required for some types of fractures, dislocations, ruptures of tendons and ligaments. If joint function is completely lost, if conservative treatment does not help, the destroyed joint must be removed and replaced with an artificial one (endoprosthesis surgery).
To prevent pain from reoccurring, a complex of rehabilitation measures is carried out using exercise therapy, massage, reflexology courses, and sanatorium-resort treatment.
What injections to give for shoulder pain
Injections are prescribed for severe pain that is not relieved by pills and external means:
- Analgin (Baralgin)
- one ampoule contains 1 ml of solution or 500 mg of active substance - a single dose for an adult; may have a toxic effect on hematopoiesis, so use it with caution; - Ketorolac (Ketorol)
– in one ampoule 30 mg of active ingredient – a single dose for an adult; contraindications: peptic ulcer of the stomach and duodenum, increased bleeding.
Blockades are widely used - injections of painkiller solutions into the most painful points.
The Moscow Paramita clinic uses the most modern methods of diagnosis, treatment and rehabilitation of all diseases that cause shoulder pain syndrome.
If necessary, if the disease threatens the patient’s life, after examination by a doctor, he is urgently sent to the hospital. But we treat most pain syndromes on an outpatient basis. Detailed information about treatment can be found on our website.
Injections for shoulder pain
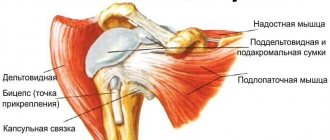
Shoulder muscles
Shoulder muscles
In addition to the complex network of ligamentous structures that connect adjacent bones, the importance of the surrounding musculature cannot be overstated. Active muscle contractions are necessary to maintain stability of the shoulder complex.
The musculature of the shoulder complex can be divided into global motors of the shoulder and finely tuned stabilizers of individual joints. Larger muscles such as the trapezius, levator scapulae, pectoral muscles, deltoid and serratus anterior, latissimus dorsi, rhomboids, teres major, biceps brachii, coracobrachialis and triceps brachii are responsible for various actions during time of movement of the shoulder joint. They provide gross movements of the upper quadrant.
The PCL-stabilizing muscles: the supraspinatus, subscapularis, infraspinatus, and teres minor muscles are classified as the rotator cuff muscles, and are attached to the head of the humerus within the glenoid fossa. Collectively, they act as dynamic stabilizers of the ACL joint, maintaining a centralized position of the humeral head within the glenoid fossa, under both static and dynamic conditions. It has been suggested that the rotator cuff tendons fuse with the ligaments and labrum, so contractions of these muscles may provide additional stability to the RCL by strengthening static structures during movement.
Synchronized contractions of the rotator cuff muscles center the humeral head during movement. This avoids physical damage to tissue (located primarily anterior and superior to the LCL), which is associated with injury and pain in the shoulder area. As previously noted, due to its anatomical location in the subacromial space, the rotator cuff tendons are particularly vulnerable to compression, abnormal friction, and ultimately pinching during active activities. Correct positioning of the humeral head is important for normal motion of the humeral head and activities of daily living.
Read also[edit | edit code]
- Examination (arthroscopy) of the shoulder joint
- Damage (tear) of the rotator cuff
- Subacromial bursitis
- Biceps tendinitis
- Biceps rupture
- Torn pectoralis major muscle
- Shoulder instability
- Shoulder dislocation: symptoms, treatment
- Labral rupture
- Shoulder capsulitis
- Clavicle fracture: symptoms, treatment
- Humerus fracture
- Clavicle dislocation
- Brachial plexopathy
- Long thoracic nerve neuropathy
- Suprascapular nerve neuropathy
- Musculocutaneous nerve neuropathy
- Axillary nerve neuropathy
- Thoracic outlet syndrome
FAQ
In what cases does pain radiate to the shoulder?
With cervicothoracic osteochondrosis, it begins in the neck and extends to the shoulder girdle and arm.
Why might shoulder pain occur during pregnancy?
As a woman's body prepares for childbirth, the ligaments and tendons relax. This happens not only in the pelvic area, through which the fetus passes during childbirth, but throughout the entire body. This includes the shoulder joint becoming slightly unbalanced. With light loads, it may become sore. This is not dangerous.
With adequate conservative therapy, the patient can be relieved of pain, achieving complete recovery or stable remission. In medicine they know how to do this.
Literature:
- Belyaev A.S. Principles of treatment of myofascial pain syndromes / A.S. Belyaev, O.M. Maslova, I.V. Eliseeva // Manual medicine. 1994. No. 7. pp. 24-25.
- Mironov S.P. et al. Shoulder pain syndrome: monograph. Volgograd: VolgMU Publishing House, 2006. 287 p.
- Campbell CC, Koris MJ Etiologies of shoulder pain in cervical spinal cord injury. Clin-Orthot. 1996. 322(2). 140-145.
Sign up for a free initial appointment