Hip joint
Hip joint, art.
coxae, is formed on the side of the pelvic bone by a hemispherical acetabulum,
acetabulum
, more precisely its
facies lunata
, which includes the head of the femur.
A fibrocartilaginous rim, labium acetabulare
, runs along the entire edge of the acetabulum, making the cavity even deeper, so that together with the rim its depth exceeds half the ball.
This rim extends over the incisura acetabuli
in the form of a bridge, forming
a lig.
transversum acetabuli .
The acetabulum is covered with hyaline articular cartilage only along the facies lunata, a fossa acetabuli
occupied by loose adipose tissue and the base of the ligament of the femoral head. The articular surface of the femoral head articulating with the acetabulum is generally equal to two-thirds of the ball. It is covered with hyaline cartilage, with the exception of the fovea capitis, where the ligament of the head is attached. The articular capsule of the hip joint is attached along the entire circumference of the acetabulum.
The attachment of the articular capsule on the thigh in front runs along the entire length of the linea intertrochanterica, and in the back it runs along the femoral neck parallel to the crista intertrochanterica
, stepping away from it to the medial side.
Due to the described location of the line of attachment of the capsule on the femur, most of the neck ends up lying in the joint cavity. The hip joint has two more intra-articular ligaments: the mentioned lig. transversum acetabuli
and ligament of the head,
lig.
capitis femoris , which with its base starts from the edges of the acetabulum notch and from
the lig.
transversum acetabuli ;
with its apex it is attached to the fovea capitis femoris
. The head ligament is covered with a synovial membrane, which rises onto it from the bottom of the acetabulum.
It is an elastic pad that softens the shock experienced by the joint, and also serves to conduct blood vessels into the head of the femur. Therefore, if this shell is preserved during fractures of the femoral neck, the head does not die.
The hip joint is a limited ball-and-socket joint (cup-shaped joint), and therefore allows movement, although not as extensive as in a free ball-and-socket joint, around three main axes: frontal, sagittal and vertical. Circular movement, circumductio, is also possible.
The lower limb flexes and extends around the frontal axis. The greater of these two movements is flexion due to the lack of tension of the fibrous capsule, which has no posterior attachment to the femoral neck. When the knee is bent, it is greatest (118 - 121°), so that the lower limb, at its maximum flexion, can be pressed to the stomach; with the limb extended at the knee, the movement is less (84 - 87°), since it is inhibited by the tension of the muscles on the back of the thigh, which are relaxed when the knee is bent.
Extension of the previously bent leg occurs to a vertical position. Further posterior movement is very small (about 19°), since it is inhibited by the stretching lig. iliofemorale; when, despite this, we extend the leg further, this occurs due to flexion at the hip joint of the other side. Around the sagittal axis, abduction of the leg (or legs, when they are moved simultaneously to the lateral side) and a reverse movement (adduction) occurs when the leg approaches the midline. Abduction is possible up to 70 - 75°. Around the vertical axis, the lower limb rotates inward and outward, which in its volume is equal to 90°.
The external ligaments of the joint are located according to the three main axes of rotation: three longitudinal (ligg. iliofemorale, pubofemoral et ischio-femorale) - perpendicular to the horizontal axes (frontal and sagittal) and circular (zona orbicularis), perpendicular to the vertical axis.
1. Lig. iliofemorale
located on the front side of the joint. Its apex is attached to the spina iliaca anterior inferior, and its expanded base is attached to the linea intertrochanterica. It inhibits extension and prevents the body from falling backward when walking upright. This explains the greatest development of this ligament in humans; it becomes the most powerful of all the ligaments of the human body, supporting a load of 300 kg.
2. Lig. pubofemorale
is located on the medial inferior side of the joint, extending from the pubis to the lesser trochanter, and intertwining with the capsule. It delays abduction and inhibits external rotation.
3. Lig. ischiofemorale
It begins behind the joint from the edge of the acetabulum in the area of the ischium, goes lateral over the femoral neck and, weaving into the capsule, ends at the anterior edge of the greater trochanter. It delays medial rotation of the thigh and, together with the lateral part of the ligamentum iliofemorale, inhibits adduction.
4. Zona orbicularis
has the form of circular fibers, which are embedded in the deep layers of the articular capsule under the described longitudinal ligaments and cover the femoral neck in the form of a loop, growing at the top to the bone under the spina iliaca anterior inferior. The circular arrangement of the zona orbicularis corresponds to the rotational movements of the hip.
It should be noted that in a living person the ligaments do not reach their maximum tension, since inhibition is to a certain extent achieved by muscle tension in the circumference of the joint.
The abundance of ligaments, greater curvature and congruence of the articular surfaces of the hip joint in comparison with the shoulder joint make this joint more limited in its movements than the shoulder joint, which is associated with the function of the lower limb, which requires greater stability in this joint. This limitation and the strength of the joint are also the cause of dislocations that are more rare than in the shoulder joint.
Frontal section of the female pelvis, T1-weighted image (magnetic resonance imaging): 1 - internal iliac artery; 2 - body of the uterus; 3 - ovary; 4 - vertebral body; 5 - psoas major muscle; 6 - uterine rough; 7 - acetabulum; 8- head of the femur; 9 - greater trochanter of the femur; 10 - rectum; 11 - ischium.
X-ray examination of the hip joint
Standard radiography of the hip joint is carried out in 2 projections. In addition to the straight line, an auxiliary oblique is used, which can be a lateral or posterior oblique, providing for hip abduction. The choice, in this case, depends on the goals of the study and the nature of the patient’s disorders.
| Projection | Features of X-rays |
| X-ray of the hip joint in direct projection | The patient assumes a supine position with the lower limbs straightened. The foot on the affected side should be turned inward. This position of the patient's body provides a good view of the medial part of the femoral neck and makes it possible to identify medial fractures. |
| X-ray of the hip joint in oblique projection | The patient assumes a supine position, the affected limb is bent at the knee and turned outward in an oblique projection. If there is a suspicion of a hip fracture localized in the neck area, the oblique projection is not used, since it can lead to displacement of bone fragments and aggravate the situation. |
| X-ray of the hip joint in lateral projection | The patient assumes a supine position, the affected limb is bent at the knee and hip at an angle of 90°. A special stand is placed under the heel, and the X-ray tube is placed on the side of the healthy leg. |
Blood supply to the hip joint
The hip joint receives arterial blood from the rete articulare
, formed by branches
a.
circumflexa femoris medialis et lateralis (from a. profunda femoris) and
a.
obuturatoria . From the latter the city acetabulars departs, which is directed through the lig. capitis femoris to the head of the femur. Venous outflow occurs into the deep veins of the thigh and pelvis - v. profunda femoris, v. femoralis, v. iliaca interna. The outflow of lymph is carried out through deep lymphatic vessels to the nodi lymphatici inguinales profundi. The joint capsule is innervated from the nn. obturatonus, femoralis et ischiadicus.
Hip joint. The muscles acting on it, their innervation, blood supply and lymphatic drainage.
The hip joint is formed by the acetabulum of the pelvis and the head of the femur.
The articular capsule of the hip joint on the pelvic bone is attached around the circumference of the acetabulum so that the latter is located inside the joint cavity. Inside the cavity is a ligament of the head of the femur .
Externally, the capsule is strengthened by three ligaments: the iliofemoral ligament
,
the pubofemoral ligament
, and
the ischiofemoral ligament
. The hip joint is a type of ball-and-socket joint. It allows movements around three axes. Flexion and extension are possible around the frontal axis of the hip joint. Due to movements around the sagittal axis in the hip joint, abduction and adduction of the lower limb occurs in relation to the midline. The head of the femur rotates around the vertical axis in the hip joint. Circular movement is also possible in the joint. Iliopsoas muscle , m. iliopsoas. Function: flexes the thigh at the hip joint. Innervation: plexus lumbalis. Blood supply: a. iliolumbalis, a. circumflexa ilium profunda. Gluteus maximus muscle, m.
gluteus maximus, Innervation: n.
gluteus inferior.Blood supply: a. glutea inferior, a. glutea superior, a. circumflexa femoris medialis. Gluteus medius muscle, i.e.
gluteus medius, Innervation: n.
gluteus superior.Blood supply: a. glutea superior, a. circumflexa femoris lateralis. Gluteus minimus, i.e.
gluteus minimus , Innervation: n.
gluteus superior.Blood supply: a. glutea superior, a. circumflexa femoris lateralis. Tensor fascia lata, i.e.
tensor fasciae latae, Innervation: n.
gluteus superior.Blood supply: a. glutea superior, a. circumflexa femoris lateralis. Quadratus femoris muscle, i.e.
quadrdtus femori Innervation: n. ischiadicus.
Blood supply: a. glutea inferior, a. circumflexa femoris medialis, a. obturatoria. Obturator externus muscle, i.e.
obturator externus. Innervation: n. obturatorius. Blood supply: a. obturatoria, a. circumflexa femoris iateralis.
Links
| This is a draft article on anatomy. You can help the project by adding to it. |
| : Incorrect or missing image | To improve this article it is desirable:
|
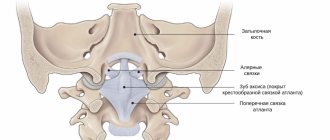
| Trochlear joint: | Interphalangeal joints • Humeral-ulnar joint |
| Condylar joint: | Atlanto-occipital joint • Knee joint |
| Saddle joint: | Carpometacarpal joints |
| Flat joint: | Facet joints |
| Stiff joint (amphiarthrosis): | Sacroiliac joint |
| Rib cage: | Sternoclavicular joint • Acromioclavicular joint |
| Taz: | Sacroiliac joint • Articulus pubis |
| Shin | Bones (Tib bone • Fibula) Sections: distal (Ankle (ankle)) |
| Foot | Sections (Tars • Metatarsus • Toes); Support points (Heel • Ball of foot) |
| see also | Synovial fluid • Meniscus (anatomy) • Plantar • Locomotion • Flatfoot • Lower extremity girdle • Hip joint • Knee joint • Ankle joint • Achilles heel • Calves • Buttocks • Nails |
Anatomy of the human hip joint: structure of muscles and ligaments and bones
Hello, dear guests and site visitors! The main load during movement falls on the musculoskeletal mechanisms and joints.
The quality of a person’s full life depends on the health of the hip joint. At the same time, the anatomy of the hip joint is characterized by complexity.
This is the connection between the pelvic bone and the head of the femur. To protect against abrasion, the surface is equipped with hyaline cartilage.
The bursa is a protective barrier. The performance of the hip joint depends on its health and condition.
What is the structure of the hip joint?
The hip joint is a ball-and-socket joint formed by the acetabulum and the head of the femur. Let's look at the structure of an important joint and its main components:
- The head of the femur bone is round in shape and covered with cartilage tissue. Fixed with a neck.
- The acetabulum is created by three fused bones. Inside there is a cartilaginous lining in the shape of a crescent.
- The acetabular labrum is a cartilaginous border for the acetabulum.
- The joint capsule is a sac of connective tissue that encloses the head, neck and acetabulum.
- Ligaments strengthen the capsule from the outside. There are only three of them.
- The ligaments of the femoral head are located in the joint cavity.
- Bursae are containers of fluid. They are located under the tendons.
- Muscles that fix elements. They help move the hip and strengthen the joint.
Blood flow and innervation of the joint involves the participation of the following arteries:
- Circumflex femoral artery, ascending branch.
- Round ligament artery.
- Deep branch of the medial artery.
- Both types of gluteal arteries.
Characteristics of the circulatory system are important for a full study of the structure of joints. You can see how the vessels pass in the photo.
With age, nutrition through the vessels decreases.
Excerpt describing the hip joint
On the 22nd, at noon, Pierre was walking uphill along a dirty, slippery road, looking at his feet and at the unevenness of the path. From time to time he glanced at the familiar crowd surrounding him, and again at his feet. Both were equally his own and familiar to him. The lilac, bow-legged Gray ran merrily along the side of the road, occasionally, as proof of his agility and contentment, tucking his hind paw and jumping on three and then again on all four, rushing and barking at the crows that were sitting on the carrion. Gray was more fun and smoother than in Moscow. On all sides lay the meat of various animals - from human to horse, in varying degrees of decomposition; and the walking people kept the wolves away, so Gray could eat as much as he wanted. It had been raining since the morning, and it seemed that it would pass and clear the sky, but after a short stop the rain began to fall even more heavily. The road, soaked by rain, no longer absorbed water, and streams flowed along the ruts. Pierre walked, looking around, counting steps in threes, and counting on his fingers. Turning to the rain, he internally said: come on, come on, give it more, give it more. It seemed to him that he was not thinking about anything; but far and deep somewhere his soul thought something important and comforting. This was something of a subtle spiritual extract from his conversation with Karataev yesterday. Yesterday, at a night halt, chilled by the extinguished fire, Pierre stood up and moved to the nearest, better-burning fire. By the fire, to which he approached, Plato was sitting, covering his head with an overcoat like a chasuble, and telling the soldiers in his argumentative, pleasant, but weak, painful voice a story familiar to Pierre. It was already past midnight. This was the time at which Karataev usually recovered from a feverish attack and was especially animated. Approaching the fire and hearing Plato’s weak, painful voice and seeing his pitiful face brightly illuminated by the fire, something unpleasantly pricked Pierre’s heart. He was frightened by his pity for this man and wanted to leave, but there was no other fire, and Pierre, trying not to look at Plato, sat down near the fire. - How's your health? - he asked. - How's your health? “God will not allow you to die because of your illness,” said Karataev and immediately returned to the story he had begun. “...And so, my brother,” continued Plato with a smile on his thin, pale face and with a special, joyful sparkle in his eyes, “here, my brother... Pierre knew this story for a long time, Karataev told this story to him alone six times, and always with a special, joyful feeling. But no matter how well Pierre knew this story, he now listened to it as if it were something new, and that quiet delight that Karataev apparently felt while telling it was also communicated to Pierre. This story was about an old merchant who lived decently and God-fearingly with his family and who one day went with a friend, a rich merchant, to Makar. Stopping at an inn, both merchants fell asleep, and the next day the merchant's comrade was found stabbed to death and robbed. A bloody knife was found under the old merchant's pillow. The merchant was tried, punished with a whip and, having pulled out his nostrils - in the proper order, said Karataev - he was sent to hard labor. “And so, my brother” (Pierre caught Karataev’s story at this point), this case has been going on for ten years or more. An old man lives in hard labor. As follows, he submits and does no harm. He only asks God for death. - Fine. And if they get together at night, the convicts are just like you and me, and the old man is with them. And the conversation turned to who is suffering for what, and why is God to blame. They began to say, that one lost a soul, that one lost two, that one set it on fire, that one ran away, no way. They began to ask the old man: why are you suffering, grandpa? I, my dear brothers, he says, suffer for my own and for people’s sins. But I didn’t destroy any souls, I didn’t take anyone else’s property, other than giving away to the poor brethren. I, my dear brothers, am a merchant; and had great wealth. So and so, he says. And he told them how the whole thing happened, in order. “I don’t worry about myself,” he says. It means God found me. One thing, he says, I feel sorry for my old woman and children. And so the old man began to cry. If that same person happened to be in their company, it means that he killed the merchant. Where did grandpa say he was? When, in what month? I asked everything. His heart ached. Approaches the old man in this manner - a clap on the feet. For me, he says, old man, you are disappearing. The truth is true; innocently in vain, he says, guys, this man is suffering. “I did the same thing,” he says, “and put a knife under your sleepy head.” Forgive me, he says, grandfather, for Christ’s sake.
Basic joint movements
Now briefly on the movements of the joints.
The hip joint is responsible for the following actions:
- Hip flexion. In this case, the muscles of the anterior surface are loaded.
- Extension. The muscles of the back of the thighs and buttocks are involved.
- Hip abduction. The muscles located on the outer surface of the thigh act.
- Bringing. Cross steps. In this case, the muscles of the inner thigh are involved.
- Supination or outward rotation. In this case, the external muscle group functions.
- Pronation rotates the hip inward. The back of the thigh and buttock muscles work.
- Circular rotation of the hips.
Treatment of coxarthrosis (arthrosis of the hip joint)
Coxarthrosis, or arthrosis of the hip joint, is a degenerative-dystrophic disease, often starting with damage to the cartilage and accompanied by the development of an inflammatory process, which over time leads to varying degrees of deformation of the joint, which is why it is also called deforming arthrosis.
Coxarthrosis can occur at any age, but is more common in the elderly. There may be significant damage to one or both hip joints, which often leads to disability and/or surgical treatment. The disease is more common in women than men.
Causes of frequent damage to the hip joint
This is due to some features of its structure and function:
- As you know, the entire weight of a person’s body is transferred directly through the hip joints to the lower limbs, and in old age it is often excessive.
- Throughout life, this organ periodically experiences severe overload - lifting weights, playing sports, running and multiple microtraumas from small jumps, bruises, falls and after car accidents.
- The deep position of the articular head in the articular cavity and the fact that most of it is covered with hyaline cartilage affects its blood supply - it is often insufficient. This leads to disruption of its “nutrition,” premature “wear and tear” of the articular parts, and the development of degenerative-dystrophic changes with compensatory involvement of periarticular (para-articular) soft tissues in the process.
- Heredity and congenital anomaly of the femoral head
- The joint is also susceptible to the development of osteoporosis, and this leads to a decrease in its strength and frequent injury; and a sedentary lifestyle exacerbates this process.
- Often there are developmental disorders (dysplasia) and congenital deformities of one or two hip joints, pelvic bones, which the patient first learns about only after undergoing an X-ray examination, examination by an orthopedist, and often already as an adult.
Mechanism of formation of joint coxarthrosis
The process, as a rule, begins with the articular cartilage: it dehydrates, becomes less elastic, gradually becomes thinner and loses its strength and shock-absorbing properties. Therefore, the bone tissue adjacent to it becomes denser - osteosclerosis develops in it, and the articular surface gradually flattens, and small outgrowths - osteophytes - form along its edges.
At the same time, single small cysts appear in the bone tissue of the articular cavity, and osteoporosis develops. All this is often accompanied by inflammation in the synovium. Gradually, the range of motion in the joint decreases, the adjacent tendons and muscles are involved in the process, they are often tense, spasmodic and painful.
As the process progresses, the articular cartilage is gradually destroyed, the bone tissue of the articular head and articular cavity is “exposed”, their surfaces come closer and gradually grow together, a bone block is formed - bone ankylosis. At the same time, the limb is shortened, the pelvis is distorted, and the load on the other joint increases significantly, which will accelerate the development of similar changes in it.
The most common symptoms of coxarthrosis
At first, patients begin to be bothered by stiffness when moving the joint, then a slight pain when walking, over time it intensifies, becomes longer and more intense, and then permanent, this leads to “sparing” the sore limb, the desire to reduce the load on it and the appearance of lameness , and over time, muscle wasting of the diseased limb.
At the same time, the pain begins to bother me more at night, when the weather changes (meteosensitivity appears). Often the pain radiates to the knee, buttock and along the outer surface of the thigh - trochanteritis and bursitis (inflammation of the periarticular bursae) develop there; very often patients are bothered by severe pain in the groin area.
In addition, asymmetrical load on the legs and pelvis leads to a redistribution of the load on the entire musculoskeletal system and is often accompanied by pain in the back, lower back, radiating along the back of the thigh (along the sciatic nerve). Patients tend to move less, complain of increased fatigue, irritability, sleep disturbances, and decreased mood.
What should you do if such signs appear?
You must first consult a doctor (preferably an orthopedic traumatologist or rheumatologist) and undergo the examination prescribed by him. Usually this:
- radiography, computed tomography of the hip joints and pelvic bones or magnetic resonance imaging,
- Ultrasound of the hip area and vessels of the lower extremities,
- ultrasound or x-ray densitometry to determine bone density and determine the severity of osteoporosis,
- clinical blood test,
- biochemical blood test (creatinine, urea, total and direct bilirubin, ALAT, ASAT, alkaline phosphatase, total protein, C-reactive protein, rheumatoid factor, antistreptolysin-O, uric acid, total calcium, phosphorus, calcitonin, parathyroid hormone and others),
- consultations with related specialists (neurologist, endocrinologist and others),
- electroneuromyography and other studies.
You should consult a doctor when the first symptoms appear, while the joint is still preserved and you can stop the development of inflammation, prevent complications, without bringing the process to surgical treatment and its replacement with an artificial implant (endoprosthetics).
Trying to treat pathology on your own leads to an increased risk of disability. By self-medicating, patients only waste time, since taking dietary supplements, rubbing with ointments, compresses, therapy with various home physiotherapeutic devices, etc. cannot stop this process, but only muffles the pain and other symptoms.
Treatment of coxarthrosis of the hip joint
Treatment of the pathology depends on the stage of development of the pathological process, among which are coxarthrosis of the hip joint of degrees 1, 2 and 3. First of all, therapy is aimed at reducing pain, relieving muscle spasms, improving tissue trophism and blood circulation in the organ, improving nutrition and restoring the structure of damaged cartilage tissue, increasing joint mobility and strengthening the muscles of the limb.
Conservative therapy includes a combination of medications and physiotherapeutic methods. Various groups of drugs are prescribed:
- analgesics,
- NSAIDs (Voltaren, Arcoxia, Movalis, Xefocam, etc.),
- muscle relaxants (mydocalm, sirdalud) – to relieve muscle spasms and improve blood circulation,
- chondroprotectors (glucosamine, chondroitin sulfate, alflutop, rumalon, structum, etc.) – to restore the structure of damaged cartilage tissue,
- vascular drugs to improve blood supply to the joint area, which restores metabolism and oxygen delivery to tissues.
In particularly difficult cases, intra-articular injections are performed:
- anti-inflammatory drugs are used in the acute stage of the disease to reduce inflammation in the joints, manifested by edema and swelling; in such cases, intra-articular injection is quite effective and alleviates the patient’s suffering. More than three injections are not given into one joint, and the interval between injections should be 5-7 days;
- drugs from the chondroprotector group, these drugs are used not only at the early stage of the disease, which occurs without tumor and edema. They contribute to the partial restoration of articular cartilage tissue, promote the production of joint fluid and improve its properties. This is a fairly effective group of drugs, since they directly affect the cause of the disease and stop the process of destruction of articular cartilage;
- hyaluronic acid preparations - to reduce friction of damaged articular surfaces, which improves joint mobility and protects cartilage surfaces from further destruction;
- intra-articular injections of autologous platelet-rich plasma isolated from the patient’s blood – PRP therapy. Platelets contain growth factors that stimulate regeneration processes.
Along with drug therapy, the attending physician prescribes a course of physiotherapy (SWT, laser therapy, ultrasound), therapeutic massage, kinesio taping, manual and other types of therapy methods. They are necessary not only to reduce tension and spasms of muscles and ligaments, but also to improve blood supply and innervation, also help to activate metabolic processes, reduce swelling and inflammation, and subsequently help restore range of motion in the joint and prevent the development of contractures .
Surgical methods are resorted to when conservative therapy does not bring results.
You can find out more about the treatment and prevention of coxarthrosis, and make an appointment for a consultation and appointment with our specialists by calling us in the Contacts section.
Hip problems
The hip joint is subject to various unpleasant phenomena. This can be trauma, fracture, dislocation, inflammation and pathology.
After 40 years, due to wear and tear of cartilage, bone destruction and coxarthrosis occur. As a result, joint contracture may develop.
Congenital dislocation is a consequence of dysplasia. Femoral neck fractures are common in older people. Bones become brittle due to lack of calcium. Therefore, a fracture can occur even after a minor injury and it is difficult to heal.
Inflammation or arthritis occurs against the background of systemic diseases that affect the joints.
Ligaments of the hip joint
The most powerful ligament is the iliofemoral ligament. The ligamentous apparatus also includes the pubofemoral ligament. It limits the range of motion within which the hip is abducted.
The ischiofemoral ligament begins on the ischium. The circular ligament is located inside the joint capsule. It covers the neck of the femur bone and protects the blood supply to the vessels that are inside it. Thanks to powerful ligaments on the front surface of the thigh, the vertical position of the torso is achieved.
These parts of the joint maintain the vertical position of the femoral bones of the pelvis and torso. The iliofemoral ligament is capable of stopping extension.
The ischiofemoral ligament, which runs along the back of the joint, is not so developed.
Muscles
The shoulder and hip joint have several axes of rotation - vertical, anteroposterior and transverse.
In each of them, the pelvic joint uses a specific group of muscles:
- The transverse axis performs flexion and extension, thanks to which a person sits down.
- The following muscles are responsible for hip flexion: the sartorius, the tensor muscle, the rectus muscle, the pectineus muscle, and the iliopsoas muscle.
- The gluteus maximus, semimembranosus and semitendinosus muscles extend the thigh.
- The gluteus minimus and medius, piriformis and obturator internus muscles are responsible for hip abduction.
- Pronation is provided by the semimembranosus, semitendinosus and tensor muscles.
- The quadratus, gluteus maximus and iliolumbar muscles are responsible for supination.
Indications and contraindications for radiography of the hip joints
Indications
Diagnosis of hip joints is carried out for many diseases of the musculoskeletal system. It allows you to identify pathological conditions of the joint that occur as a result of:
- Injuries suffered: dislocations, cracks and injuries;
- Degenerative-dystrophic disease - osteoarthritis;
- Death of the bone tissue of the femoral head - necrosis;
- Neoplasms of hip bone tissue;
- Pathologies of inflammatory etiology: arthritis, osteomyelitis;
- Congenital anomalies in the form of hypoplasia or dysplasia;
- Metabolic disorders, which are represented by diseases such as osteoporosis and gout.
In addition, radiography of the pelvis and hip joints is carried out as part of preoperative preparation in order to determine the scope of the intervention and its tactics.
Contraindications
Despite the fact that the radiation dose during diagnostics is minimal and does not cause harm to the human body, the procedure is used only in extreme cases - if:
- the patient is pregnant or breastfeeding;
- the patient is in serious condition;
- if the patient is under 15 years of age;
- if the patient has received a high dose of radiation in the last 12 months;
- for diseases of the thyroid gland.
As for contraindications when using radiopaque agents, in addition to the above, they are as follows:
- individual intolerance to contrast components;
- severe renal and liver failure;
- intestinal obstruction;
- blood clotting disorders;
- diabetes mellitus in severe form.