Inversions of the knee joint are anatomical structures that allow stabilizing the movement of synovial fluid inside a complex bone articulation. The fluid in the knee joint in the normal state constantly circulates and does not stagnate. However, in pathologies, its accumulation may occur. As a result, excess cavity pressure is created inside the joint. Pain, stiffness in movement, and disruption of the position of the patella and the condyles of the tibia and femur may appear.
The knee joint is formed by three bones: the tibia, femur and patella. Two of them enter the joint capsule; the patella, due to its own ligaments, remains outside. Its main function is to limit joint mobility in the anterior plane. The tibia and femur in the joint are connected by the anterior and posterior cruciate and two lateral (lateral and medial) ligaments. This device stabilizes the position of the bone heads and prevents them from moving relative to each other.
Inside the articular cavity is the synovial membrane. It covers the condyles of the femur and tibia and creates several inversions of the knee joint. These protrusions communicate with the cavities of the joint capsules (bursae), due to which the synovial fluid is evenly distributed and the level of cavity pressure is equalized throughout the joint.
Recessus superior is the most impressive in size of the superior recess. It connects to the bursa located at the base of the quadriceps muscle (bursa synovialis suprapatellaris). Therefore, purulent inflammation of this volvulus is always accompanied by suprapatelar bursitis of the knee joint. Puncture of this protrusion is carried out for diagnostic purposes. If pus or accumulation of leukocyte mass is detected in the extracted synovial fluid, it indicates the development of bursitis.
Other volvuluses are less significant, however, fluid can accumulate in them. We will consider their anatomy in more detail later in the article. For now, let us dwell on the possible causes of pathological changes. These include injury to the joint capsules. Inflammatory processes in them can be purulent, degenerative and ischemic in nature.
The bulk of clinical cases of suppuration occur in the posterior inversions. They have no communication with the front ones. Synovial fluid can accumulate in them, and when pathogenic microflora penetrates, the process of inflammation begins. This can be caused by factors such as decreased immunity, the presence of foci of chronic infection in the body (caries, pyelonephritis, glomerulonephritis, adenoiditis, tonsillitis, sinusitis, etc.). The posterior inversions communicate with the synovial joint capsules. Therefore, any accumulation of fluid is compensated by its outflow into the bursa. Acute bursitis develops, accompanied by severe pain, impaired knee mobility, etc.
If you have pain in the knee joint and a feeling of stiffness, then many pathologies may develop. You need to see a doctor as soon as possible. In Moscow, you can make an appointment for a free appointment with an orthopedist at our manual therapy clinic. Here the doctor will conduct an initial examination and make a preliminary diagnosis. Individual recommendations for treatment will be given.
What is fluid accumulation in a joint?
The accumulation of fluid in the joint is considered one of the symptoms of hydrarthrosis or dropsy - a peculiar syndrome in which the volume of the joint increases due to the formation of synovial fluid in its cavity.
Most often, this syndrome is observed in the knee joint, less often in the ankle, elbow and others. In this case, there may be a restriction in joint flexion; the intensity of pain depends on the amount of fluid and the degree of stretching of the joint capsule. An increase in local temperature is not observed unless the inflammatory process has begun.
Superior inversions of the knee joint
When performing an ultrasound or MRI, you can often see in conclusion that the superior inversion of the knee joint is widened or that there is fluid in it. What does this mean and how to carry out treatment correctly?
Normally, fluid in the superior inversion of the knee joint is present in limited quantities. This is due to the special location of the synovial canal. With the development of deforming osteoarthritis, the back pocket is primarily affected, so the shock-absorbing load is shifted to the upper inversion of the knee joint, which provokes excessive stretching of the cavity and accumulation of a large amount of fluid inside. This can lead to compression of the surrounding soft tissue, causing pain, swelling of the joint and limited mobility.
The superior anterior inversion of the knee joint, located above the knee, has a connection with the suprapatellar joint capsule. This allows him to equalize cavity pressure due to the outflow of fluid. However, if it accumulates excessively, a secondary form of suprapatellar bursitis may develop.
The quadriceps femoris tendon lies above this synovial recess. When it is injured, with subsequent scarring, partial displacement of the volvulus may occur with compression of other pockets of the synovial membrane.
The lateral and medial anterior inversions of the knee joint are located above along the lateral projections of the protruding parts of the condyles of the tibia and femur. They are connected to each other - liquid flow is possible. These formations are classified as extra-articular; they come into contact with the menisci and partially supply them with fluid. Connected to the superior patellar inversion.
The lower anterior ones are also divided into internal and external. They provide nutrition to the menisci from the lower surface. Closed by the infrapatellar body. Connected to the joint capsule of the same name.
Causes
The accumulation of fluid in a joint can be a consequence of a disease, but the most common cause is injury. These include:
- Injury – sprain, ligament rupture. This can lead to a buildup of fluid that becomes infected after a viral illness.
- Various joint diseases, including gout or arthritis.
- Lupus erythematosus.
- Bursitis, which is common in dancers or athletes.
- Incoagulability of blood and others.
Important! These reasons must be mentioned when visiting a doctor, this will help to correctly establish a diagnosis and prescribe competent treatment.
Posterior twists of the knee joint
The medial posterior inversion of the knee joint separates the meniscus and the femoral condyle. Attached to the gastrocnemius muscle at the junction of the tendon and the fascial sheath. Inside it is covered by the semimembranosus muscle and partially provides its stabilization during movement.
The posterior lateral recess secures the suprapatellar inversion of the knee joint, stabilizes the plantaris muscle, and connects to the lateral head of the gastrocnemius. It communicates with the articular capsule, which fixes the popliteus muscle. When this inversion is inflamed, compression of the sciatic nerve often occurs at the site of its bifurcation into the tibial and peroneal branches. If characteristic pain and a feeling of numbness appear in the lower leg and foot, it is necessary to exclude damage to this synovial pocket.
Effusion in the superior inversion of the knee joint on the back of the leg can occur with:
- sprain and rupture of the posterior cruciate ligament;
- penetration of infection into the joint cavity;
- violation of microcirculation of blood and lymphatic fluid;
- prolonged compression of the knee area from the back side (often occurs in people who have the habit of sitting with their legs crossed);
- arthritis and exacerbation of deforming osteoarthritis;
- after significant physical exertion.
During the diagnosis, a puncture is made. If it is difficult to make a correct diagnosis, diagnostic arthroscopy is recommended. During the procedure, minimally invasive surgery is possible, for example, to restore the integrity of the cruciate and collateral ligaments.
Classification
The fluid that accumulates in the joint cavity can be classified by its nature into exudate and transudate. Accordingly, exudate is associated with the occurrence of inflammatory processes and comes in several types:
- Serous.
- Purulent.
- Hemorrhagic.
- Frail.
Transudate is formed for other reasons that are not related to inflammation, but are associated with circulatory disorders and other abnormalities.
Pathologies
The accumulation of fluid in the joints is a health hazard and can lead to the development of the following pathologies:
- Hemarthrosis is formed due to damage and blood flow into the joint.
- Arthrosis is the most common pathology and occurs as a result of mechanical damage or age-related changes.
- Arthritis can occur for a variety of reasons, including infections or allergic reactions.
- Synovitis is an inflammatory disease.
- Bursitis can develop due to injury or after an infectious disease.
Diagnosis of the causes of fluid accumulation in the joint
Diagnosis of this pathology consists of an initial examination of the patient by a specialist, for example, an orthopedist or traumatologist. After an external examination, palpation and questioning of the patient, the doctor makes a preliminary diagnosis and refers the patient for additional examination for clarification:
- x-ray,
- Ultrasound of the joint,
- MRI of the joint
- joint puncture and others.
Reference! To identify hidden infections, a general or extended blood test, ECG and blood type identification may be needed.
After carefully studying the examination data, the specialist will prescribe comprehensive treatment depending on the cause of the disease.
Main manifestations
The symptoms by which you can determine what fluid is entering the joint are very diverse. It depends on the cause of the pathology and its location. Common features are:
- red spots on the skin;
- high temperature - throughout the body or only in the area where the pathology develops;
- stiffness or limited movement (manifests itself when there is a large amount of fluid in the synovial bursa);
- mild or clearly noticeable swelling at the site of pathology development;
- dense formations near the joint;
- dull, sharp or constant nagging pain;
- in some cases, headaches and chills (mainly if the cause of the illness is an infection).
Which doctor treats fluid accumulation in a joint?
The accumulation of fluid in the joint is considered a fairly common problem, which, even in the absence of pronounced symptoms, requires immediate seeking qualified medical help. Like treatment of the spine, fluid removal from the joint cavity should be done immediately after the problem is discovered. You need to contact an orthopedic traumatologist who specializes in diseases of the musculoskeletal system and rehabilitation after surgical interventions.
In our Kuntsevo treatment and rehabilitation center, you will not only receive qualified assistance from experienced orthopedic traumatologists if fluid is detected in the joints, but you will also be able to undergo a full examination using the latest diagnostic equipment and, if necessary, recover in our rehabilitation center after injuries according to a specially developed comprehensive program .
The accumulation of fluid in the joint significantly reduces the patient’s quality of life. As a rule, a person cannot fully perform movements and complains of pain and discomfort in the joint area.
Important! This symptom cannot be ignored, because the progression of the pathology can lead to the development of chronic inflammatory joint diseases.
At the first signs of pathology, make an appointment with a qualified doctor - orthopedic traumatologist at the Kuntsevo Treatment and Rehabilitation Center, who will be able to fully examine the joint, find the source of the pathology and prescribe the correct treatment, in particular at the rehabilitation stage.
Sign up
Types of treatment for fluid accumulation in a joint
The accumulation of fluid in the joint can be treated in different ways, depending on the degree of advanced disease. Among the various joint treatment methods offered by the Kuntsevo Center, the following can be listed:
- Drug treatment, which consists of prescribing and taking medications and vitamins.
- One of the ways to treat joint diseases and relieve pain is blockade - special injections into the joint or periarticular tissue. This method of therapy is also used during the rehabilitation period after completion of treatment.
- ACP SVF therapy is the latest unique method for treating degenerative joint diseases. To carry out this type of treatment, it is necessary to extract the stromal-vascular fraction from the patient, then prepare a special composition based on it and introduce it into the affected area of the joint by injection.
Rupture of the lateral collateral ligament of the knee joint
The lateral collateral ligament (LCL), or fibular collateral ligament, is one of the main stabilizers of the knee joint, the main purpose of which is to prevent excessive varus deviation and posterolateral rotation of the knee joint. In most cases, UCL injury results from a forceful blow to the anteromedial aspect of the knee that combines hyperextension and excessive varus force. The UCL can also be injured by non-contact varus deviation or non-contact hyperextension. Most often, UCL injuries occur in sports (40%) with high-speed turns and jumps, such as football, basketball, skiing or hockey. It was found that the highest likelihood of isolated UCL injury occurs in tennis and gymnastics [1].
The UCL can be stretched (grade I), partially torn (grade II) or completely torn (grade III) [2]. The UCL is rarely injured on its own, and therefore concomitant injury to the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), and posterolateral complex often occurs along with the UCL when the lateral aspect of the knee is injured [1][2][3].
Brief overview of anatomy
The lateral collateral ligament is a cord-like structure of the arcuate ligament complex together with the biceps femoris tendon, the popliteus muscle and its tendon, the meniscopopliteal and popliteus fibular ligaments, the oblique popliteal ligament, the arcuate and fabellofibular ligaments and the lateral gastrocnemius muscle [3][ 4].
The UCL is a strong connection between the lateral epicondyle of the femur and the head of the fibula with the function of resisting varus deviation of the knee joint and external rotation of the tibia. When the knee is flexed more than 30°, the UCL is relaxed. The ligament is stretched when the knee is in an extended position [2].
Clinical picture
Acute stage
Patients with acute UCL injury experience pain, swelling, and bruising on the lateral line of the joint and difficulty trying to put full weight on the leg. Less common complaints include limping when walking, paresthesia down the lateral aspect of the lower extremity, and weakness and/or foot drop [1][2].
On examination, a patient with an acute UCL injury may exhibit decreased range of motion (ROM), instability in weight bearing, and quadriceps weakness (inability to lift a straight leg upward). The patient will experience pain and also demonstrate excessive mobility when performing the varus stress test [2].
Subacute stage
Patients with subacute knee joint injury experience pain in the lateral aspect of the knee joint, stiffness in the final range of flexion or extension, general weakness and, in some cases, instability.
Chronic stage
Patients with a chronic UCL injury will have nonspecific knee pain, significant weakness throughout the kinetic chain, and potential instability and maladaptive movement patterns [4].
Differential diagnosis
Because of its close proximity to surrounding structures, UCL injuries often occur in conjunction with other ligament injuries, including the ACL, PCL, and posterolateral complex, and often occur in conjunction with knee dislocations. In some cases, damage to the menisci may occur. Other injuries such as hamstring tendon avulsion, iliotibial tract syndrome, and distal hamstring tendinopathy should be excluded [3].
Physical examination
The information collected during the subjective examination of the patient is important for making a diagnosis. Conducting a full physical examination will allow the specialist to make the most appropriate differential diagnosis. On examination, patients with suspected UCL injury will have swelling, bruising, and possible localized temperature elevation along the lateral line of the joint. The full range of motion should be assessed and careful palpation along the lateral line of the joint should be performed. If possible, a clinical gait analysis should be performed to identify the classic sign of knee varus, which is common in UCL injuries. Isolated injury to the UCL is rare, so specific tests should be performed to determine associated ligamentous, meniscal, or soft tissue injuries [1].
Objective examination:
- Inspection
- Palpation
- Active Range of Motion (ROM)
- Muscle testing
- Gait Analysis
- Special tests
- Neurological examination (if necessary)
Special tests:
- The varus stress test is the most useful specific test in the evaluation of UCL injury. First, the test is performed with the knee joint flexed 30 degrees. Increased weakness or poor contact between the articular surfaces indicates injury to the UCL with possible damage to the posterolateral complex. The test is then performed with the knee fully extended. Improvement in stability indicates isolated injury to the UCL, whereas persistence of loose apposition is a positive test for injury to the UCL along with the posterolateral complex.
- External rotation test with recurvation - excessive hyperextension compared to the opposite limb indicates a positive test.
- Posterior drawer test - excessive posterolateral displacement is a positive test and indicates injury to the posterolateral complex.
- The reverse anterior subluxation test is positive if there is tibial displacement at 30 degrees of knee flexion. The test must be performed on both legs to detect a negative result on the opposite limb.
- Dial test - performed on both legs at 30 degrees and 90 degrees of knee flexion. An increase in external rotation of 10 degrees or more is a positive test and indicates injury to the posterolateral complex.
*Due to the possibility of other ligamentous lesions, anterior and posterior drawer tests should be performed, as well as specific tests for patellar luxation [1].
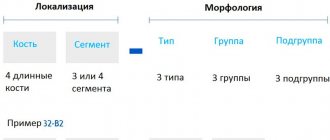
Classification of injuries: [1]
LCL injuries are classified into three grades depending on severity.
I degree: minor sprain
- Increased tenderness and pain over the lateral collateral ligament.
- Little or no swelling.
- The varus stress test at 30° is painful but does not show ligament laxity (<5 mm laxity).
- No instability or mechanical symptoms.
II degree: partial rupture
- Considerable tenderness and pain over the lateral and posterolateral side of the knee.
- Severe swelling in the LCL area.
- The varus stress test is painful, there is excessive mobility in the joint with a pronounced end point (mobility 5-10 mm).
III degree: complete rupture
- Pain may vary and be less severe than with a second degree tear.
- Increased sensitivity and pain in the lateral part of the knee and in the area of injury.
- The varus stress test shows the presence of significant excess joint motion (mobility >10 mm).
- Subjective instability.
- Significant swelling.
Diagnostic Imaging
- Radiographs—PZ and lateral radiographs are used to rule out associated structural injuries such as fibular head fractures/avulsions (arcuate sign), tibial roughness avulsions, or lateral tibial plateau fractures (Segond fracture). If an arcuate sign or Segond fracture is evident, it indicates injury to the posterolateral complex and further evaluation of the UCL is warranted [1].
- MRI is considered the gold standard in the diagnosis of injuries to the UCL and posterolateral complex. Coronal and sagittal T1 and T2 weighted images have 90% sensitivity and specificity in detecting UCL injuries [1].
- Ultrasound is an effective tool used when it is necessary to quickly diagnose a UCL injury. On examination, injury to the UCL may be apparent if thickening and hypoechogenicity are present. If a complete tear is present, ultrasound may show increased swelling, dynamic laxity, and/or lack of continuity of the UCL fibers [1].
Medical treatment
1st and 2nd degrees: for acute injury of the 1st and 2nd degree LCL, rest, use of cold, pressure bandage and NSAIDs are recommended [1]. In cases of grade I or II injury to the UCL, conservative treatment is most often performed [5]. Patients are contraindicated to bear weight on the leg for the first week and are advised to continue wearing the hinged orthosis for the next 3-6 weeks, along with functional rehabilitation to maintain medial and lateral stability [1].
3rd degree: for acute 3rd degree LCL injury, rest, use of cold, pressure bandages and NSAIDs are also recommended [1]. A grade III UCL tear is a more severe injury with the potential for injury to the ACL, PCL, and posterolateral complex. In this case, surgery is necessary to prevent further instability of the knee joint [6]. Recent literature reports that reconstructive surgery is the best treatment option for grade 3 UCL injuries in order to achieve knee stability with normal biomechanics [1][7]. Surgical treatment of isolated UCL injuries includes reconstruction of the UCL using a semitendinosus tendon autograft [1].
- Postoperative rehabilitation may include modification of the foot's weight bearing capacity during the first six weeks. After surgery, leaning on the leg is contraindicated [5]. A knee immobilizer may be used to limit valgus/varus loading of the knee and to limit knee flexion during walking. At an early stage, exercises should be performed to restore the range of motion in a position without support on the leg. Upon completion of the initial stage of the postoperative period, you can proceed to full rehabilitation, which is described in detail in the next section. It should be noted that in case of concurrent meniscus surgery, deep squats should be avoided for the first four months [5].
Physical Therapy/Rehabilitation
Acute stage [5]
- POLICE or RICE protocols.
- Measures to reduce pain.
- Measures to reduce swelling.
- Fixation in a knee immobilizer or adjustable brace that allows limited flexion but full extension of the knee.
- Unload the knee with crutches (as needed).
- Early mobilization of the knee joint.
- Exercises to activate the quadriceps muscle.
- Raising the straight leg up.
- Electrical stimulation to prevent muscle atrophy due to immobilization [8].
Subacute stage
- Full support on the leg - retraining to walk.
- Full active range of motion (AROM) of the knee joint.
- Progressive exercises for the quadriceps, glutes, calves, and hamstrings.
- Training in a closed kinetic chain.
Long-term therapeutic measures
- Development of proprioception.
- Plyometric exercises with emphasis on reducing excessive knee varus or tibial external rotation [9].
- Strengthening and loading the entire kinetic chain.
- Aerobic training.
Exercises for a torn lateral collateral ligament (LCL)
see exercises for rupture of the knee joint
Let's sum it up
Injury to the lateral collateral ligament of the knee can be caused by varus deviation or hyperextension. With an injury to the UCL, there is likely to be associated damage to the ACL, PCL, posterolateral complex, and lateral structures of the knee joint. In cases of a grade III UCL tear, reconstructive surgery may be required to prevent further instability of the knee joint. Conservative treatment should always be the initial choice.
Sources
- Yaras RJ, O'Neill N, Yaish AM. Lateral Collateral Ligament (LCL) Knee Injuries. StatPearls [Internet], 2020
- Logerstedt DS, Snyder-Mackler L, Ritter RC, Ax MJ, Godges JJ. Knee stability and movement coordination impairments: knee ligament sprain: clinical practice guidelines linked to the international classification of functioning, disability, and health from the Orthopedic Section of the American Physical Therapy Association. Journal of Orthopedic & Sports Physical Therapy. 40(4):A1-37, 2010
- Recondo JA, Salvador E, Villanúa JA, Barrera MC, Gervás C, Alústiza JM. Lateral stabilizing structures of the knee: functional anatomy and injuries assessed with MR imaging. Radiographics. 20(suppl_1):S91-102, 2000
- Ricchetti ET, Sennett BJ, Huffman GR. Acute and chronic management of posterolateral corner injuries of the knee. Orthopedics. 31(5), 2008
- Lunden JB, BzDUSEK PJ, Monson JK, Malcomson KW, Laprade RF. Current concepts in the recognition and treatment of posterolateral corner injuries of the knee. journal of orthopedic & sports physical therapy. 40(8):502-16, 2010
- Pekka Kannus, MD Nonoperative treatment of Grade II and III sprains of the lateral ligament compartment of the knee. Am J Sports Med. vol. 17 no. 1 83-88, 1989
- Cooper JM, McAndrews PT, LaPrade RF. Posterolateral corner injuries of the knee: anatomy, diagnosis, and treatment. Sports medicine and arthroscopy review. 14(4):213-20, 2006
- Dr Pekka Kannus, Markku Järvinen, Nonoperative Treatment of Acute Knee Ligament Injuries. Sports medicine. Volume 9, p244-260, 1990
- Mohamed O, Perry J, Hislop H. Synergy of medial and lateral hamstrings at three positions of tibial rotation during maximum isometric knee flexion. The Knee. 10(3):277-81, 2003