What is osteoporosis?
Osteoporosis is a bone disease in which the bone structure has low density , increased fragility and a tendency to fracture. The weakening of the physical parameters of the bone occurs due to a lack of calcium and the inability of bone tissue cells to renew themselves.
Most often, osteoporosis is diagnosed in older people, however, the pathology can also develop in children.
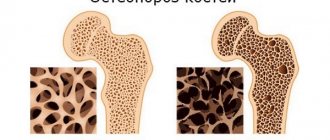
In osteoporosis, the bone structure is greatly weakened
Clinical picture of osteoporosis in children
Symptoms of pathology that develops in childhood are practically invisible and blurred at the initial stage. Osteoporosis is diagnosed in children along with concomitant diseases: scoliosis, kyphosis and other pathologies that require studying the bone structure.
Childhood osteoporosis develops quite quickly, and during its development the following symptoms may be observed::
- gradual disturbance of posture and gait;
- bone pain;
- noticeable slowdown in growth;
- fractures or microfractures due to minor physical exertion;
- neurological symptoms: tingling, short-term numbness of the limbs;
- frequent headaches.
Important! Osteoporosis in children is very rare. In addition, in the early stages the disease is quite difficult to diagnose, since radiation-related diagnostics cannot be performed on children. The initial symptoms of the disease are most often associated with overwork and physical exertion in sports sections.
Degrees and classification of pathology
Pathology that develops in childhood does not have a specific classification . Osteoporosis can be described by various symptoms in accordance with morphological, etiological, pathophysiological characteristics.
As a rule, when a disease is identified, the degree of its development is noted:
- primary _ It occurs under the influence of external factors and the use of various medications. The development of pathology is not associated with parallel diseases;
- secondary _ Develops against the background of concomitant diseases.
Diseases that can provoke the development of osteoporosis in children can be either congenital or acquired.
Video: “Common Causes of Osteoporosis”
Systemic osteoporosis (part 1)
Total duration: 24:16
00:00
Rodionova Svetlana Semenovna, professor, doctor of medical sciences, head of the Scientific Center of the Institute of Traumatology and Orthopedics:
- Good afternoon.
Today we will talk about systemic osteoporosis. This is a disease that today is social. There are a lot of social factors in the risk of its development, which I will focus on.
What is systemic osteoporosis. This is a skeletal disease, which is characterized by a decrease in bone mass and a violation of its microarchitecture. All this leads to a decrease in the strength properties of the bone. Accordingly, it increases the risk of fractures.
This is the WHO definition, which was made in 1994. In fact, the disease as a separate nosological form was identified back in 1941 and belongs to the group of metabolic osteopathies. This group includes osteomalacia, Paget's disease and hyperparathyroid osteodystrophy.
First of all, I would like to say about the high prevalence of the disease. It's clear. Why. This is a social disease, just like hypertension. The more developed the society, the more often and more likely it is to encounter this disease.
Today, about 200 million women in the world suffer from systemic osteoporosis. The older a woman is, the more likely she is to have this disease.
If women aged 60 to 70 years are every third woman, then among women over 80 years old, almost two out of three women suffer from systemic osteoporosis.
There are a lot of classifications. But the very first and most common classification is the division of primary and secondary systemic osteoporosis.
Primary osteoporosis has 4 forms: juvenile, idiopathic, postmenopausal, senile. I will not dwell long on classifications. This classification of forms of primary osteoporosis has existed since 1941.
This division into forms of osteoporosis was primarily based on age. Juvenile is under the age of 25 years. Idiopathic – 25 – 50. Postmenopausal is a form of systemic osteoporosis that is registered in women with menopause. Over 75 years of age is a senile form of osteoporosis.
Secondary osteoporosis is all forms of systemic osteoporosis that are detected against the background of some existing disease. For example, pathology of the endocrine system, rheumatic diseases, taking medications (for example, steroids).
03:12
Systemic osteoporosis occurs without fractures or is complicated by fractures. In cases where systemic osteoporosis is complicated by a fracture, it is called a pathological fracture. It is a pathological fracture. The diagnosis sounds like this, for example: systemic osteoporosis, complicated by a pathological fracture of the vertebral body or femoral neck or any other bone.
Causes of primary osteoporosis. Of course, genetic factors must be taken into account. Then there are the adverse effects of the external environment, which include poor ecology, poor nutrition, and lifestyle features (low physical activity).
Today, low physical activity and bad habits such as smoking, alcohol abuse, and drugs are a serious risk factor that leads to the development of osteoporosis. Increasingly, these reasons become or underlie the increase in the number of patients with systemic osteoporosis among children and adolescents. This factor must be taken into account today.
Pathogenesis of osteoporosis. That's a very difficult question. Today it is impossible to simply talk about the pathogenesis of osteoporosis. Considering our capabilities and time, I decided to present it in the form of a diagram. This may be a violation of the histogenesis of osteoblast (OB) and osteoclast (OC) cells - cells that are responsible for the processes of reproduction, that is, the existence and remodeling of bone tissue.
Bone tissue is a very mobile living structure. The processes of resorption and formation constantly occur there, from the moment of birth to the end of life. The main role that falls to these cells is the creation of new bone tissue and its resorption. But the histogenesis of OB and OC cells can or is subject to the influence of systemic hormones. This is parathyroid hormone, sex hormones.
At the same time, cell function very closely depends on a number of cytokines, or local growth factors. There is feedback here. Violation of cell histogenesis affects local growth factors, and these growth factors, in turn, affect the histogenesis of OB and TC cells. All this together leads to impaired bone tissue remodeling. This may be in the form of an increase in the resorption process. This always leads to a deficiency of bone mass.
06:30
The opposite situation may be true. The intensity of resorption remains within normal limits. But for some reason, the process of bone formation is disrupted. At least in children with juvenile osteoporosis, there are a number of studies that show that it is the disruption of OB progenitor cells that triggers the development of this bone tissue deficiency and the formation or development of systemic osteoporosis.
The situation may be even more unexpected. The intensity of resorption and the intensity of bone formation seem to proceed adequately, but the resulting mass of bone tissue remains in deficit. All this leads to the development of the amount of bone tissue deficiency that fits into the picture of systemic osteoporosis.
How does the process of resorption and bone formation proceed in general in normal bone tissue? This is a phase process, but it does not occur immediately normally, not immediately throughout the entire mass of bone tissue, but in separate areas of bone tissue, which are called basic multicellular units. These basic multicellular units work inconsistently. This mismatch in the actions of basic multicellular units most often maintains normal tissue function.
When bone loss, such as bone resorption, occurs in concert across many basic multicellular units, bone loss can result in bone deficiency. Although the intensity of resorption does not exceed the age norm.
But the most important thing is why I am showing this slide - so that you read the word “mineralization”. When new bone tissue (osteoid) is formed, it is formed by OB, then the process of mineralization occurs.
I am showing this slide to emphasize to you once again that with systemic osteoporosis, the mineralization process is never disrupted. There is simply less bone tissue. When we talk about systemic osteoporosis, we are talking about bone loss, a deficiency of bone mass, but in no case about demineralization.
The word “demineralization” or “impaired mineralization” can only be appropriate when we are talking about another metabolic osteopathy - osteomalacia. Where the process of bone tissue is really disrupted.
09:31
Clinical manifestations are very mosaic. There are no pathognomonic symptoms of systemic osteoporosis. There is a set of clinical manifestations that allow us to suspect or think about this disease. For example, back pain, discomfort. It is very typical that these pains appear precisely during physical activity and go away with rest.
This distinguishes the pain syndrome from osteochondrosis or deforming arthrosis, when pain persists even at rest.
Finally, a more typical manifestation of osteoporosis is the presence of fractures. Fractures in systemic osteoporosis occur with low-energy trauma. What does it mean. For example, falling from a height. The woman picked up a three-liter saucepan. I cooked borscht, lifted the pan, and felt a sharp pain in my back. An x-ray reveals deformation of the vertebral body.
Fractures that can occur when sneezing, coughing, making a sharp turn, or braking a car - these are all low energy fractures. They are characteristic of systemic osteoporosis.
Another symptom that is most often ignored by both patients and doctors is decreased height.
A later manifestation of systemic osteoporosis is femoral neck fractures. It is hip fractures that have made the osteoporosis system so relevant today. These are fractures that require the greatest material and moral costs.
For the diagnosis of systemic osteoporosis, a very important point, in addition to conventional radiography, is also x-ray densitometry. This is a non-invasive method for assessing bone mass. In general, the introduction of this method into clinical practice can be said to have revolutionized the diagnosis of osteoporosis. It has become possible to detect this bone loss and make this diagnosis.
We must remember that in fact, X-ray densitometry reveals bone loss in any metabolic osteopathy (for example, osteomalacia). Today we should say that X-ray densitometry has high specificity, but insufficient sensitivity, because it does not allow identifying all patients. By doing this we are depriving some patients of treatment.
12:47
I want to tell you the following. When I personally began to use this method in clinical practice, I was completely delighted with it. But very soon I noticed that elderly patients with several fractures of the vertebral bodies in the lumbar spine and a neck fracture or femoral neck fracture had completely normal bone mass.
This should be taken into account and X-ray densitometry should not be prioritized to exclude the diagnosis of systemic osteoporosis. With this method we detect bone loss. The diagnosis of “systemic osteoporosis” is a clinical diagnosis, which should be made on the basis of the clinic, the possibility (inaudible, 13:37) of a set of X-ray (inaudible, 13:38) signs and, finally, X-ray densitometry.
Below I will show you my own data and how it all looks in practice. The column where it says “fractures” is all patients diagnosed with systemic osteoporosis and having vertebral body fractures typical for systemic osteoporosis. The “blue” bar is the proportion of individuals whose bone loss was, respectively, minus 2.5 standard deviations or even this loss was greater.
We see that some patients with true systemic osteoporosis were left without a diagnosis. This should always be kept in mind when we use X-ray densitometry. Normal indicators or insufficiently expressed by individual measures (minus one standard deviation) do not yet allow this patient to be completely discounted and not try to clarify whether he has a diagnosis of systemic osteoporosis or not.
15:01
There is a point of view that it is not necessary to start with X-ray densitometry to make a diagnosis of systemic osteoporosis. First, the clinic, anamnesis, clarification of risk factors, radiography, and only then X-ray densitometry.
Of course, X-ray densitometry is an indispensable method for monitoring the effectiveness of treatment if we find this loss at the beginning of diagnosing the patient.
Today they are talking about a validated method for diagnosing osteoporosis. According to WHO recommendations, it is believed that its diagnostic value can even exceed X-ray densitometry.
What is taken into account here? Age, history of fractures, indication for hormone therapy, low body weight, presence of risk factors such as smoking, alcohol abuse, early menopause, amenorrhea, hypogonadism, prolonged immobilization, insufficient intake of calcium from food, indication that mother or Grandmother had a hip fracture. These are the risk factors that lead the clinician to think about the presence of systemic osteoporosis in a given patient and evaluate him accordingly.
Typical fractures for osteoporosis. These are vertebral body fractures, femoral neck fractures and radial fractures. A radial fracture is a fracture that can be considered a harbinger, a marker that one should think about osteoporosis. These women are at risk.
With systemic osteoporosis, other fractures are also possible. These are fractures of the pelvis, chest, ribs, and shoulder. In my practice, there were several cases when the first fractures in patients with osteoporosis were reconstruction fractures under light load, with minor trauma. Fractures of the tibia.
Even the Institute of Orthopedics and Traumatology did not immediately sort out these fractures. We had to take several x-rays to still see these reconstruction fractures, then examine these patients, perform x-ray densitometry on them and confirm the presence of systemic osteoporosis.
Of course, the problem of systemic osteoporosis and its social significance is determined by the number of fractures. The slide shows the total number of fractures in Northern Europe - data from 2005. Fractures due to osteoporosis. The red bars are the number of fractures that are associated with osteoporosis.
18:21
This is why systemic osteoporosis ranks 4th (now, they say, it has moved to fifth) among all causes of disability and mortality. Most likely, not from osteoporosis itself, but from hip fractures. Not even at the moment of fracture, but from the complications that later develop in these patients.
Today, 68% of all fractures in hospital are fractures that occur against the background of systemic osteoporosis. Including, some of the patients are patients who even received high-energy trauma. These are the most difficult cases to diagnose.
A man falls from the second floor and receives fractures of many skeletal bones. He is considered to have post-traumatic fractures and is treated accordingly. Suddenly the fracture does not heal. It does not grow together in the prescribed time frame, within two prescribed periods, it does not grow together for three years. They begin to examine him. It turns out that the person has systemic osteoporosis, so his fracture (one or two) does not heal.
Outcomes of femoral neck fractures. 20% die within the first year, 40% cannot walk without crutches, and 80% have difficulty caring for themselves.
I would like to dwell on the reasons for this mechanical failure of bone tissue. The most important sign of osteoporosis is low bone mass, followed by structural abnormalities. Today, great importance is attached to qualitative disorders of bone tissue.
The role of bone mass reduction. It is obvious. More than half of all fractures of the femoral neck and vertebral bodies in patients with osteoporosis occur against the background of low bone mass. Losses exceed 2.5 SD according to the T-score.
20:24
Risk factors for fracture. If bone mass decreases by even one standard deviation, the risk of hip fracture increases by one and a half times, and with a greater decrease, even by 2.5 times. But it turned out that in patients with low values, femoral neck fractures occur no more often than with normal values in the same age group.
How is this possible, is it possible? We conducted the following research. Patients with systemic osteoporosis were identified, some of whom had femoral neck fractures. Then they made a comparison. The amount of bone loss in the group of patients with femoral neck fractures due to systemic osteoporosis, and simply patients with systemic osteoporosis without a femoral neck fracture.
This was work completed in 2000. It turned out that in the group with fractures the bone mass was higher than in the group without fractures. These data give us, and therefore you, reason to say that bone loss does not always lead to a risk of fracture. Some other structural parameters need to be taken into account. For example, the thickness of the anterior inferior cortical layer of the femoral neck, porosity of the cortical layer of the fracture, the length of the femoral neck.
Studies conducted at CITO and then at other institutes have shown that the axial length of the femoral neck in women is important. The longer the neck, the higher the risk of fracture. We did not find this pattern in men. In women, the structural features of the femoral neck were found to influence bone strength regardless of the amount of bone loss.
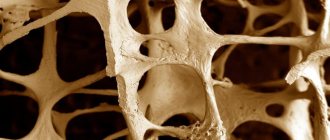
Finally, I would like to dwell on the quality of bone tissue. The quality of bone tissue is the size and shape of hydroxyapatite crystals, the structure of bone proteins, the microarchitecture of trabeculae, the viability of bone tissue cells, and the ability to restore microfractures.
Form of hydroxyapatite crystals (scanning electron microscopy) in osteoporosis and normally. With osteoporosis, hydroxyapatite crystals increase in size, and their strength properties decrease. Moreover, the decrease in hydroxyapatite crystals, which are observed during the use of pharmaceuticals used to treat systemic osteoporosis, increases the activity of the chemical interaction of minerals with inorganic substances of bone tissue. This has a positive effect on bone mass.
Accumulation of microfractures. There are numerous studies that show that in systemic osteoporosis, the number of microfractures accumulates more than normal.
In fact, microfractures are the engine of progress. Normal functioning of bone tissue always occurs with microfractures, but their number is certain. The more they accumulate and the process of bone tissue restoration slows down, the more likely the formation of bone tissue deficiency.
Prevalence and significance
Osteoporosis in childhood is not common . Pathology of bone tissue structure most often occurs in old age. However, the onset of the disease in childhood can cause serious pathological processes in the bone skeleton, which can subsequently negatively affect the functioning of internal organs.
During the primary stage of development of the disease, attention should be paid to nutrition, physical activity and lifestyle, since most often the disease occurs due to a lack of vitamins (calcium, vitamin D) and an unbalanced diet.
Important! During the period of growth, the child’s nutrition should be selected in such a way that the diet provides the body with all the necessary minerals and vitamins. Most often, children with an unbalanced and vitamin-poor diet, as well as those with a genetic predisposition to the disease, suffer from the disease.
Can we fix everything?
The process of formation of healthy bone tissue can be adjusted as the child grows. For treatment, medications containing calcium are prescribed.
There is a wide choice: for example, for the sake of prevention and in case of a slight deviation from the norm, calcium supplements with vitamin D are prescribed. If a deficiency of not only calcium, but also some microelements is detected, complex preparations are used (they also include manganese, boron, copper, zinc, magnesium ).
Since the absorption of calcium is affected by some chronic diseases, children who have them are selected with special medications, for example, for gastritis with high acidity - those that “protect” the process of its absorption from the aggression of gastric juice. The course of continued treatment is individual.
But medication alone is not enough. Treatment should be supported by a diet: cottage cheese, cheese, kefir or yoghurt, fish (salmon, sardines), meat, eggs, broccoli, bananas, and legume dishes are recommended.
And, of course, you need to make time for sports: at least for regular visits to the pool or fitness room. Precisely regular, not occasionally.
Risk factors, causes in children
Risk factors that can provoke the development of osteoporosis in children can be divided into:
- modifiable (which may subsequently change). These include calcium deficiency, insufficient vitamin D in the body, poor physical activity;
- unmodifiable (unchangeable processes). This category includes genetic predisposition, bone mineral density, and a tendency to fall.
The definition of osteoporosis is based on mineral density and the ability of bone tissue to regenerate.
Pay attention to how bone tissue is formed
The following conditions may increase the risk of osteoporosis in children::
- early birth (prematurity);
- diseases of the gastrointestinal tract in chronic form;
- pathologies of the endocrine system;
- rare exposure of the child to the sun;
- intestinal diseases;
- exposure to toxic substances;
- smoking in early (childhood) age.
Taking glucocorticosteroids for adrenal disease may also adversely affect bone health.
Consequences
If we consider the consequences of the development of osteoporosis, it is important to note that when the disease appears, the structure of bone tissue is disrupted , which contributes to the occurrence of fractures even with minor bruises and falls.
If the bone is brittle, there is a possibility of fracture of the spine or important joints . This circumstance can cause the child to be immobilized for a long time or become disabled.
Video: “Causes of osteoporosis in children”
Osteoporosis due to pathology of the parathyroid glands
PTH increases the calcium content in the blood plasma, promoting its absorption in the intestine (affecting the synthesis of 1,25-(OH)2-D3) and stimulating the reabsorption of calcium in the renal tubules, as well as affecting bone resorption.
Disorders of parathyroid hormone metabolism are one of the common causes of endocrine AP in children. Hyperparathyroidism is divided into primary, secondary and tertiary. Primary hyperparathyroidism in children is uncommon and can be caused by an adenoma and, less commonly, hyperplasia of the parathyroid gland (or glands). Hyperparathyroidism occurs in newborns with mutations in both alleles of the calcium-sensitive receptor gene, which is manifested by hypocalciuria and hypercalcemia.
Secondary and tertiary hyperparathyroidism are more common. Secondary develops in response to a decrease in the level of calcium in the blood due to diseases of the liver, kidneys, intestines, as well as vitamin D deficiency. Tertiary hyperparathyroidism develops in those patients in whom the secondary form has existed for a long time, and it is subsequently joined by the autonomous synthesis of PTH in the body , even when eliminating the factor that stimulated excessive PTH secretion.
Hyperparathyroidism in children is manifested by: excessive activity of osteoclasts, fibrosis and the formation of cyst-like cavities (osteitis fibrosa cystica). This is a classic variant of bone changes, however, due to the increasing use of modern diagnostic techniques and early diagnosis, such changes are detected less and less often. More often, diffuse demineralization of bone tissue is found, similar to that in senile AP [7]. To a greater extent, the compact bone substance is involved in the process. Bone resorption occurs at the growing ends of long bones and subperiosteally, especially on the medial side of the phalanges of the fingers. Patients may have complaints of painful sensations in the bones, low-painful pathological fractures of various locations that do not heal for a long time. A strong bone callus usually forms at the site of fractures, which is why repeated fractures in the same place are not observed. Patients experience changes in their “duck-like” gait. The clinic is characterized by multiple deformations of the axial skeleton: the height of the vertebral bodies decreases, they become fish-shaped, and kyphosis and kyphoscoliosis develop as a result of compression fractures. For primary hyperparathyroidism, surgical treatment is indicated.
Hypoparathyroidism can develop both when there is insufficient secretion of PTH, and when the structure of the hormone or its receptors is disrupted. Hypoparathyroidism can occur already in the neonatal period: transient, sporadic, familial forms of the disease. In pseudohypoparathyroidism, the concentration of PTH in the blood is normal, but the target cells are insensitive to it as a result of a G protein mutation. This is accompanied by hypocalcemia and hyperphosphaturia. It is considered typical that such patients have a lag in physical and mental development, the development of early cataracts and subcutaneous ossifications. Skeletal changes are also characteristic, which manifest themselves in the bones of the feet and hands by shortening the 4th and 5th metacarpal and/or metatarsal bones. This skeletal change is easy to detect when examining a patient; you just have to ask him to bend his hand into a fist, and it will be clearly visible that the knuckles are not in the same line. In addition to skeletal pathology, in all variants of hypoparathyroidism, the presence of other symptoms associated with hypocalcemia is noted: tonic spasms of skeletal muscles, mainly of the extensor group of the upper extremities, which are preceded by a stage of precursors (pins and needles, paresthesia, etc.), spasm of the facial muscles (“sardonic smile” ), spasm of the “obstetrician’s hand” type, spasms of intestinal smooth muscles manifested by abdominal pain, and spasms of the respiratory muscles (laryngospasm). Sometimes spasms of the smooth muscles of internal organs simulate the clinical picture of many diseases: appendicitis, cholecystitis, stomach ulcers, bronchial asthma, migraine, etc. Prolonged laryngospasm can lead to death due to asphyxia.
With long-term hypoparathyroidism, children are stunted in growth, their tooth formation is impaired, and caries develops. Due to reduced mobilization of calcium from bones, its content in the blood serum remains low. X-ray diagnostics and determination of bone mineral density indicate a decrease in calcium content in the bones.
Calcium preparations, vitamin D and its analogues are used in treatment. The best drug is considered to be calcitriol, an analogue of the active metabolite of vitamin D - 1,25-(OH)2-D3.
Symptoms and diagnostic methods
Did you know that...
Next fact
The main reason for late detection of pathology in a child is the asymptomatic course of the disease in the early stages of the disease.
The following symptoms may prompt you to consult a doctor::
- complaints of pain in the legs, back (spine);
- fatigue when standing or sitting for a long time;
- discomfort and pain that go away while lying down;
Among the main symptoms of childhood osteoporosis are frequent bone fractures and distorted posture; the child’s mood and pain in the bones intensify with sudden changes in weather.
As the disease progresses, other symptoms may occur.:
- poor posture, sharp decrease in growth rate;
- change in gait with waddling from side to side;
- headache;
- cramps in the legs, goose bumps in the hands;
- dull, brittle nail plates;
- brittle hair;
- dental problems.
Important! If signs of osteoporosis appear, the child frequently complains of pain in the legs and other symptoms, you should undergo a medical examination. Do not hesitate to visit a doctor, as any fall of a child can cause serious problems.
Diagnostics
To identify the cause of the symptoms of the disease, it is necessary to carry out a number of measures:
- X-ray examination. Can determine bone density, vertebral transformation;
- blood chemistry. Detects the amount of calcium in the body;
- ultrasonography. Determines the degree of thinning of bone tissue;
- densitometry. A study that helps determine the mineral density of tissue.
The doctor studies genetic predisposition, risks and propensity to develop the disease. Young children are not examined using hardware; most often, the composition of the blood is studied.
Pay attention to the features of osteoporosis in adults:
- What tests are taken for diagnosis of osteoporosis in men and women?
- The causes, symptoms and treatment of male osteoporosis are described on the page
- Learn more about the causes and treatments of osteoporosis in women here
Features of treatment in children
Treatment of osteoporosis in children involves the use of several techniques, each of which is advisable to use at a specific stage of the disease:
- drug treatment;
- exercise therapy exercises;
- massage;
- additional treatment at home.
In extreme cases, when the disease leads to compression of the vertebrae, surgical treatment is required. Kyphoplasty or vertebroplasty are used - methods that ensure straightening and stabilization of the vertebra by introducing a polymer or a special balloon into it. In childhood, as a rule, such operations are not required, since the disease is cured at earlier stages.
Drug treatment
When treating the disease, the emphasis is on additional intake of vitamin D and calcium into the body. This includes taking medications that contain calcium, as well as vitamin D , which helps absorb calcium.
These elements are basic when using drug therapy.
In addition, drugs that help improve metabolism in bone tissue : flavone elements and hydroxyapatite compounds with ossein.
In addition to medications, it is advisable to use medications that inhibit bone resorption (bisphosphonates, strontium, calcitonin).
Physical therapy exercises
It is worth noting that exercise therapy for osteoporosis should be carried out with great caution and only under the supervision of a specialist.
As part of the complex therapy of osteoporosis, therapeutic exercises are important, as they help strengthen not only muscle tissue, but also bones. For children, exercise difficulty is not a priority for treatment. The ability to actively move and develop the bone skeleton is the main focus of physical exercise.
Massage
For osteoporosis, massage can also be used as a general strengthening remedy , as well as to increase muscle tone. Massage can improve blood supply to bone tissue, as well as eliminate pain and improve well-being.
Treatment at home
Treatment of osteoporosis in children at home is aimed at taking foods, herbs, and decoctions that improve the condition of bone tissue and help strengthen bone structure.
It is effective for children to include foods rich in calcium and protein in their daily diet. In folk medicine, eggshells, dill decoction, propolis and other remedies are often used internally.
Important! Most often, treatment of osteoporosis in children is limited to taking painkillers, as well as including foods in the diet that help improve bone structure. The result of treatment for osteoporosis largely depends on the approach to the disease and correctly prescribed therapy.
Recovery prognosis and prevention
To prevent osteoporosis in children, special attention should be paid to nutrition. To prevent osteoporosis in childhood, you should pay close attention to the child’s nutrition - this is the key to not only preventing osteoporosis, but also eliminates the risk of improper development of the child’s body and its health.
An important condition for preventing serious bone diseases is mobility, daily exposure to fresh air, and moderate exposure to the sun.
For children, training and sports activities will not hurt to stimulate the strength and health of the body.
Children suffering from osteoporosis can be successfully treated , restore bone strength and ensure stable bone density for many years if all doctor's recommendations are followed. After treatment, you should constantly monitor your lifestyle and diet to ensure a normal balance of vitamins and minerals in your body.