Almost every adult has encountered pathological fractures in one way or another - either from their own sad experience, or from the example of relatives and friends. And now we ourselves begin to say: “The most important thing is not to break your hip in old age and not to lie bedridden” or “I, like many women of my age (over 50 years old), broke my wrist.” Alas, along with vertebral fractures, fractures of the femoral neck and distal epiphysis of the radius are indeed among the most common pathological fractures. However, the good news is that these injuries are now preventable in many cases.
Pathological fracture: an idea of the problem and its symptoms
A pathological fracture is a violation of the integrity of the bone at the site of its pathological restructuring. Most often, a pathological fracture occurs “out of the blue” - that is, in the case when the force of the impact (from a bruise or fall) is clearly insufficient to damage healthy bone tissue. At the same time, a typical story about an injury looks something like this: “Well, I didn’t seem to hit it hard, but I broke my arm.” Or: “Every year in winter I fall 1-2 times, like all people. But this year I seemed to fall quite lightly and get a fracture out of the blue.”
In this case, the clinical signs of a pathological fracture completely coincide with those of ordinary fractures. In fact, the only distinguishing feature of this injury is that a pathological fracture most often occurs with minor trauma. Therefore, patients often seek medical help too late, without even realizing that they may have a fracture.
Pathological fractures of the spine (which in the vast majority of cases are compression fractures localized in the vertebral body) are especially often “overlooked.” The easiest way for a non-medic to imagine the essence of this damage is to draw an analogy between the spongy bone of a vertebra and a slice of fresh bread. If you squeeze the bread with your fingers, the crumb will crumple—the same way the vertebral body “crushes” during a compression fracture. The healing of this injury will be somewhat similar to restoring the shape of bread that is not too “bruised”, only very extended over time.
Despite the fundamental ability of the vertebral body to restore its structure with relatively minor damage, any fracture of the spine (including compression) is very dangerous. If the height of a vertebra is violated, the spine becomes deformed (kyphosis occurs), which contributes to damage to other vertebrae and the progression of kyphosis. In the case of compression of nerve endings accompanying the injury, pain, paresis (numbness, “pins and needles”) and muscle weakness occur in the corresponding innervation zone.
With a pathological fracture, when interviewing the patient, in some cases it is possible to identify a history of complaints of pain and discomfort in the area where the fracture subsequently occurred.
The final diagnosis of a pathological fracture can be confirmed (or refuted) by radiography or computed resonance tomography.
Symptoms
A pathological bone fracture is accompanied by very mild symptoms of the disease. This is due to the fact that it occurs at the slightest injury, after which it is impossible to immediately determine the presence of a fracture.
At first, the disease causes minor pain, which may be accompanied by swelling of the soft tissues. It is these signs that may indicate the presence of a pathological bone fracture. Unpleasant manifestations of the disease can occur under loads, even minor ones.
With this type of fracture, there is no hemorrhage, or its presence is not visible during the initial examination. This happens because it is internal.
Sometimes a bone callus appears in the area of the fracture, which can be felt when palpated. Very often, the presence of cracks, bends, or indentations can turn into a fracture due to any damage.
Such symptoms do not make it possible to quickly diagnose a pathological fracture, as they cause a late visit to a medical facility.
Pathological fracture: causes
The causes of pathological fractures are conditions leading to the destruction of bone tissue. Thus, demineralization of bone tissue is promoted by excessive formation of the parathyroid hormone (parathyroid hormone), which occurs in hyperparathyroidism, including those caused by parathyroid adenoma.
Another cause of a pathological fracture is a tumor lesion of the bone. If there is a primary tumor or metastasis of a malignant neoplasm in the bone tissue, its structure changes, the bone becomes more fragile, and with the slightest damage a pathological fracture occurs in the affected area. That is why, if there is a suspicion of an oncological process, it is necessary to begin diagnostic measures, in particular, prescribe a biopsy of bone tissue from the damaged area.
Osteomyelitis - another cause of pathological fractures - is most often found in children, as well as in the area of endoprosthetics, comparison of bone fragments, as well as bone injuries of any origin, complicated by infection (in the vast majority of cases - Staphylococcus aureus). The most typical localization of osteomyelitis is the lower leg bones, femur and humerus, upper jaw, and vertebrae. Pathological fractures also occur, caused by a bone abscess that develops as a result of trauma.
Finally, the most common cause of pathological fractures is osteoporosis.
Total information
The provocateur against which the described damage occurs can be congenital and acquired diseases of bone tissue. The impact of force is only an impetus for the occurrence of a fracture.
The incidence of the described disorder naturally increases with age. The reasons are as follows:
- age-related depletion of cat tissue is observed;
- in older and older people, systemic lesions of bone tissue more often appear, against the background of which the described pathological fracture occurs.
All areas of the humerus are affected equally often.
Fractures due to osteoporosis
Osteoporosis is a widespread pathology that occurs, on average, in every third woman and every fifth man over 50 years of age. We can say that the world is experiencing an epidemic of osteoporosis in people in the second half of life! What is this terrible disease?
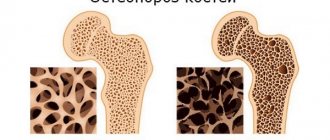
Osteoporosis is a metabolic bone disease in which bone mass decreases and bone structure changes so that bones become more fragile and therefore more prone to pathological fractures. In the vast majority of cases, osteoporosis is spoken of in connection with menopausal changes in the female body. This connection is understandable: during fertile (i.e. childbearing) age, female sex hormones (estrogens) maintain bone strength, and with changes in hormonal levels associated with menopause, the amount of estrogens decreases, and bones become especially fragile. Although osteoporosis is also not uncommon in older men. This is why pathological fractures are much more common in older people.
Osteoporosis is confirmed by bone densitometry (primarily bone mineral density) and biochemical markers of osteoporosis. Most often, blood tests are performed for osteocalcin, bone alkaline phosphatase, acid phosphatase, pyridinoline, collagen degradation products, and procollagen peptides. Sometimes some of these markers are detected in urine.
But a study such as radiography, which is mandatory for any fracture, cannot always help in diagnosing osteoporosis: on an X-ray, its signs are visible only when at least 30% of the bone mass is lost.
Therefore, experienced doctors often begin to suspect osteoporosis (and, as a consequence, a pathological fracture) not so much based on the changes in the affected bone recorded on x-rays, but rather based on the location of the fracture. Thus, the most typical location of pathological fractures in osteoporosis is the distal epiphysis of the radius (Collis fracture), femoral neck, and vertebrae. At the same time, fractures in osteoporosis tend to become “cascading”: the first fracture increases the risk of the second by 2 times, the second fracture increases the risk of the third by 5 times, and so on.
Actually, a fracture in a person over 50 years of age should, in principle, raise suspicion regarding the pathological nature of the damage. In this regard, it is necessary to clarify whether the force of the fall (impact) was adequate to the injury received and find out whether the patient has had other fractures in recent years, whether she (he) has been examined for osteoporosis, or received whether anti-osteoporosis drugs. After all, it is at this age that the clinic of osteoporosis makes itself felt, which without treatment will only get worse over time.
It is also important to note the fact that pathological fractures, which occur quite easily against the background of osteoporosis, heal poorly. Speaking in “medical language,” a distinctive feature of pathological fractures is their poor consolidation, which often leads to disability in patients. And this is understandable: until the factor that caused the pathological restructuring of the bone is eliminated, restoration of its structure during healing of the damage is also extremely difficult. In addition, prolonged immobilization of patients with pathological fractures leads to the development of complications, including fatal ones (congestive pneumonia, PE (pulmonary embolism), bedsores, thrombophlebitis, etc.).
For this reason, a doctor who diagnoses a fracture in an elderly patient is obliged to prescribe an adequate examination that can identify osteoporosis: only eliminating the influence of the cause of the pathological fracture allows one to achieve not only successful treatment of the injury, but also to prevent its complications. And, of course, serve as hope for the prevention of subsequent pathological fractures!
Negative consequences
Pathological fractures of the vertebral bodies can permanently bind a person to bed and make him deeply disabled. In this case, bedsores, chronic heart failure, and congestive pneumonia develop.
Other complications include the following problems:
- Instability of the affected part of the spine, which leads to persistent limitation of its mobility and functionality.
- Neurological disorders. Their nature depends on the location of the fracture and is caused by damage from bone fragments to the spinal cord and the nerve roots extending from it. Motor and sensory disturbances, disruptions in the autonomic system, problems with urination and defecation are often observed.
- Decreased height, changes in posture and gait.
- Violation of the physiological state of neighboring vertebrae and their gradual deformation.
Measures to prevent pathological fractures
It is necessary to undergo an annual medical examination, including laboratory and instrumental examination methods. This is especially true for older people, who are most susceptible to osteoporosis. An examination by doctors of different profiles will help diagnose various health conditions and begin timely treatment.
To avoid fractures caused by osteoporosis, you need to adjust your diet, lead an active and healthy lifestyle, and take vitamins enriched with calcium and other minerals.
Treatment of pathological fractures - general principles
Treatment of pathological fractures in general is practically no different from the treatment of conventional ones. However, as a rule, the periods of immobilization for pathological fractures are extended. Therefore, in case of pathological fractures, whenever possible, special orthopedic methods are used (for example, the Ilizarov apparatus, the Shevtsov-Matsukatov apparatus), which make it possible to maintain a person’s capacity even if the consolidation is very slow.
What is most important in the treatment of pathological fractures is identifying the cause of painful bone remodeling and its elimination. So, with cancer, of course, the issue of eliminating the tumor (by surgery, chemotherapy, radiation, or a combination of these methods) comes to the fore. For pathological fractures caused by osteomyelitis, antibiotics are necessary. In some cases, surgery may be required (for example, with a bone abscess).
Well, if the cause of the pathological fracture is osteoporosis, it is necessary to treat metabolic disorders of bone tissue with the help of drugs that improve the mineral composition and microarchitecture (specific “structure”) of bones.
Bonviva for the prevention of pathological fractures in osteoporosis
The dangers of osteoporosis have been known for so long that many popular media have not ignored this topic. In particular, information about the leading role of calcium in the prevention of pathological fractures has become widespread.
However, the authors of most of these materials lose sight of the fact that the pathological changes in bone tissue that occur during osteoporosis are caused not so much by calcium deficiency in the body, but by the inability of the bones to absorb and retain it. Therefore, it is impossible to cope with osteoporosis with calcium supplements alone: special agents are also needed that will act only in bone tissue, helping to restore its structure and increase mineralization. Otherwise, it is almost impossible to prevent the pathological restructuring of bones. Therefore, at present, the greatest interest among anti-osteoporotic drugs is drugs from the group of bisphosphonates - powerful modulators of bone metabolism that can suppress the resorption (“resorption”) of bone tissue, for which special cells, osteoclasts, are “responsible”.
One of the most studied (and, most importantly, clinically tested) drugs in this group is ibandronic acid. It is on the basis of this active substance that Bonviva was created - a modern, highly effective tablet drug that is well tolerated and designed to enhance the mineralization of bone tissue and reduce the risk of pathological fractures.
It is noteworthy that Bonviva is recognized as the “gold standard” for the treatment of osteoporosis, not only due to its highest effectiveness, but also due to its ease of use: for the prevention and treatment of osteoporosis, including those complicated by pathological fractures, the drug is taken 1 tablet (150 mg) 1 time per day. month.
The exceptional convenience of using Bonviva significantly increases patient adherence to treatment: in other words, they do not stop therapy because they are tired of complying with all the requirements for the regularity and frequency of taking the medication (which, alas, is not uncommon). Well, adherence to treatment is a very important criterion for the success of treatment for osteoporosis, since anti-osteoporosis drugs must be taken for years. Thus, after 3 years of regular use, Bonviva reduces the likelihood of a fracture by more than 50%.