There is no clear answer to this question. Treatment is carried out by different specialists, depending on the causes. The main goal of therapy is to relieve discomfort. To check the success of treatment, it is necessary to undergo regular examination by a radiologist. Problems with bone tissue regeneration cause malfunctions of the thyroid gland and adrenal glands, so you need to regularly visit an endocrinologist. Frequent fractures that occur during the development of the disease are a reason to seek help from a traumatologist.
What is osteoporosis
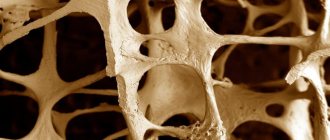
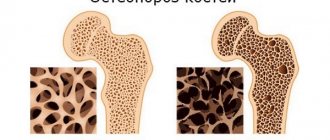
Osteoporosis is a disease that is accompanied by a decrease in the integrity of bone tissue and leads to regular fractures. When a disease occurs, mineral elements are washed out of the bone tissue, and the bones become porous. This condition affects all parts of the skeleton and causes fractures under the smallest loads. The disease affects women aged 55 years and older, during menopause. In addition, impaired bone integrity is observed in people with high levels of sweating, low weight, and a sedentary lifestyle.
What kind of doctor treats osteoporosis in women? At the first signs of the disease, it is better to consult an orthopedist or traumatologist. These doctors specialize in bones and will be able to immediately diagnose which bones and joints are at risk. After 30 years, the amount of calcium begins to decline. After 50 years, women stop producing the hormone that controls calcium balance. The destructive cells are unchecked and attack the bones.
Rheumatologist
A rheumatologist is a doctor who treats diseases of the joints and connective tissue. In advanced cases or in case of inflammation of the joint cavities, the patient should contact this specialist. A rheumatologist will help cure the disease and eliminate the following unpleasant symptoms:
- pain syndrome;
- swelling of the joints and muscles around them;
- sharp pain radiating to the limbs;
- muscle pain;
- weakness and deterioration in health.
Joint inflammation is treated with steroid drugs (hormones), which have side effects, including washing calcium out of the body. Therefore, in the therapeutic course, the rheumatologist must take this factor into account and prescribe a complex intake of drugs containing calcium and vitamin D.
Signs of osteoporosis
The first manifestations of the disease are considered to be:
- decreased bone integrity;
- depression of intervertebral discs;
- vertebral deformity.
These signs are determined during diagnosis in a hospital using x-rays or ultrasound. Ultrasound can detect structural changes when tissue integrity decreases by 5%. If it is not possible to undergo an examination, then you should pay attention to the following indirect signs:
- pain in the back (lumbar or thoracic);
- the nature of the pain can have different intensity, but it does not cause severe discomfort, only after physical activity the pain can become stronger;
- fatigue, weakness, rest takes longer;
- leg cramps, palpitations.
Having determined the signs of the disease, it remains to understand which doctor treats osteoporosis in older women. Traumatologists and orthopedists note that in older age, bones grow together very slowly. Therefore, if you experience the slightest fracture or pain, you should consult a doctor.
Symptoms
Osteoporosis may be asymptomatic for some time. At the next stage, nonspecific symptoms appear, which may indirectly indicate the onset of pathology:
- fast fatiguability;
- leg cramps at night;
- increased salivation;
- presence of bad breath;
- bleeding gums;
- peeling and brittleness of nails;
- hair loss or early graying;
- digestive disorders;
- decreased growth;
- muscle weakness.
Then they intensify, and more pronounced symptoms join them:
- obvious change in posture;
- acute pain in the intercostal spaces, subsiding in the morning, but intensifying when coughing, jumping, or turning the body;
- lower back pain;
- intervertebral hernia;
- frequent fractures;
- swelling of the feet;
- tachycardia.
Forms of osteoporosis
Osteoporosis can be primary or secondary. Primary manifests itself in the following forms:
- postmenopausal;
- senile;
- juvenile
The last two varieties are dominant. The highest bone tissue density in humans is observed at the age of 20-35, after which it begins to shrink. By the age of 75, we lose up to half of our tissue mass. An irreversible consequence of the senile form of the disease is a fracture of the femoral neck. A person stops moving and spends all the time in a lying position, and this is fraught with heart failure. It is not difficult to understand who treats osteoporosis and which doctor deals with the problem. A traumatologist or orthopedist will make a diagnosis and prescribe a certain course of treatment. The secondary form of the disease manifests itself in the presence of disruptions in the body: hormonal disorders, diseases of the endocrine system, arthritis. Experts note that malfunctions in the lymphatic system can also lead to a secondary form of the disease.
Traumatologist-orthopedist
An orthopedic traumatologist is a doctor who immediately identifies spinal pathologies and the etiological factor. This specialist examines the patient using instrumental diagnostic methods. It reveals the localization of the pathological process and the reason why the bones lose their strength. After this, the orthopedic traumatologist explains to the patient possible complications in the absence of proper treatment.
The specialist prescribes medications and regular physical exercises that will help restore metabolism in the spine. If osteoporosis is accompanied by a fracture of bones or joints, the traumatologist resets the damaged structures and performs surgical operations.
[node:field_similarlink]
Which doctor treats osteoporosis in women and men
Over the years, our bone tissue shrinks and our bones become fragile. Lack of calcium in the body leads to disruptions in the functioning of many organs. Ignoring the problem can have fatal consequences. At the first signs of osteoporosis, if you do not know which doctor to contact, then a traumatologist, rheumatologist, endocrinologist, and also an orthopedist will help you.
Traumatologist
The first symptoms of the disease are a reason to consult a traumatologist. In case of osteoporosis, this doctor will write a referral for the necessary examination and also develop an appropriate treatment plan. Often, a specialist, in addition to prescribing drug therapy, has to apply bandages and perform operations.
Endocrinologist
An endocrinologist is also a doctor who treats osteoporosis. Malfunctions of the endocrine system lead to the development of this disease. A person who suffers from a malfunction of the thyroid gland or who has been diagnosed with diabetes should be regularly examined by this specialist.
Rheumatologist
What is the name of an osteoporosis doctor who treats connective tissue disorders? Rheumatologist. The skeletal system and joints are components of connective tissue. What symptoms do you see a specialist for? Bone pain and joint dysfunction.
Orthopedist
A specialist can make a preliminary diagnosis during the examination stage. An orthopedist will explain which bones and joints are most susceptible to destruction and what pathologies may arise. If osteopenia (low calcium levels) is detected, the orthopedist will prescribe preventive medications.
Diagnostics
In addition to visiting doctors to identify osteoporosis, the patient will have to undergo a detailed examination, since the symptoms of this disease are in many ways similar to other pathologies. The success of further treatment depends on the accuracy of diagnosis and identification of causes.
For a full examination, the following is prescribed:
- blood test for calcium and phosphorus;
- urine test for markers of osteoporosis;
- skeletal x-ray;
- determination of hormones of endocrine organs;
- Ultrasound or X-ray densitometry.
Prevention of osteoporosis
Restoring the structure of bone tissue requires the following measures:
- healthy lifestyle;
- proper nutrition;
- consumption of drugs that contain easily digestible forms of calcium salts;
- physical education classes;
- sunbathing; getting rid of chronic diseases that cause impaired calcium absorption;
- regular medical supervision.
Remember that it is better to prevent the development of the disease than to get rid of its manifestations through therapeutic measures. Stick to proper nutrition, exercise regularly, and give up bad habits. People over 45 years of age are recommended to take calcium-containing supplements.
Factors indicating the need to seek medical help
This pathology has several stages. Diagnosis in the early stages is complicated by the lack of specific signs, so their appearance indicates worsening processes. For this reason, you should not postpone a visit to a medical facility to clarify the diagnosis.
There are direct and indirect signs of disturbances in phosphorus-calcium metabolism.
The main symptoms are:
- Painful sensations of a long-lasting and non-intense nature. The most common location is the lumbar or cervical spine. Such sensations are confined to periods of prolonged stay of the body in a forced position without the ability to move (30 or more minutes) or after long walks (about an hour);
- Significant decrease in growth rates. The central zone of each of the vertebrae becomes thinner, they become deformed and become smaller in height, which causes a general decrease in the length of the spine, causing deformation processes in it;
- A noticeable change in posture, expressed in the body tilting forward and stooping. These manifestations are caused by the fact that the vertebrae take on a wedge-shaped shape with worsening symptoms;
- A sharp decrease in a person’s weight with a slight decrease in body volume or a complete absence of change in volume;
- Fractures of the spine, neck of the hip joint or wrist joint without the influence of damaging factors.
Osteoporosis is characterized by a clinical picture in which women do not complain of acute pain, indicating other pathologies of skeletal structural elements. This phenomenon is explained by the slow pace of destructive processes inherent in this disease, which is why patients often delay visiting a doctor.
Indirect signs:
- Periodic cramps in the calf muscles, worsening in the evening and at night;
- Fragility and increased fragility of the nail plates;
- Premature occurrence of gray hair;
- Pathological phenomena of dental tissue and gums: worsening periodontal disease, sharp thinning of enamel, rapid deposition of tartar;
- Increased fatigue and increased weather dependence;
- Arrhythmia and increased heart rate.
Classification
Primary osteoporosis
This is the most common form of the disease. These include:
- postmenopausal osteoporosis
- senile (i.e. senile) osteoporosis
- juvenile (i.e. osteoporosis in adolescence)
- idiopathic osteoporosis (when no obvious cause of bone pain is found).
Secondary osteoporosis
It has many causes, when it is not the primary damage to bone tissue that occurs, but completely other diseases of the body, one of the manifestations of which is osteoporosis.
This group includes osteoporosis due to endocrine diseases, diseases of the gastrointestinal tract, kidney diseases, systemic diseases, blood diseases, and even taking many medications.
FAQ
How to suspect osteoporosis?
The simplest and most accessible means is to simply measure your height and pay attention to your posture. In ordinary adult life, we do not measure our height, and when a doctor comes to us with this question, we simply point to our “height in youth” or focus on the height indicated on the label of our clothes. However, it is useful to update your height annually. A decrease in height of more than 5 cm compared to height in youth or a decrease in height of more than 2.5 cm per year indicates a high likelihood of osteoporosis. The fact is that changes in posture, rounding of the back, and bending are external signs of osteoporosis, when the height of the vertebrae decreases (pathological compression fractures of the vertebral bodies occur). Sometimes patients pay attention to a “stomach that won’t go away” in the absence of general excess weight. This may also indicate osteoporosis, when as a result of asymptomatic fractures and deformities of the vertebrae, the height of the spine decreases, therefore, the volume of the abdominal cavity decreases. The internal organs need the same volume for their comfortable placement, which is why the abdomen protrudes forward.
Fracture of skeletal bones due to inadequately minor trauma is the main symptom of osteoporosis. True, the fracture that has occurred indicates an advanced process of bone suffering, when the loss of bone mass is already great and returning it to normal is simply impossible. Patients rightly ask: “Do you really need to just sit and wait for a fracture to be sure of the disease?!” It is believed that universal screening of all patients to detect osteoporosis is impractical, but it will certainly be required for people who are most at risk of developing osteoporosis.
Which skeletal bones are typically fractured in osteoporosis?
Since osteoporosis is a process that affects the entire skeleton, an osteoporotic fracture can occur in any part of the skeleton. The most common, “favorite places” are the bones of the forearm (“wrist fracture,” as patients call it), the femoral neck (a very severe fracture, after which the patient often dies or becomes disabled), and vertebrae.
Is it worth going to see a doctor and getting examined? Who exactly needs examination and monitoring of the condition of bone tissue?
You are at risk for developing osteoporosis and skeletal bone fractures, and may already be sick, if:
- You have had bone fractures from minimal trauma: spontaneous or from a fall from your own height, compression fractures of the spine accidentally discovered during X-ray
- Your age is over 65 years old
- There are patients with osteoporosis in your family (this diagnosis does not have to be on the outpatient chart), that is, if there are close relatives in the family: mother, father, siblings and brothers who suffered bone fractures from minimal trauma after the age of 45-50 years
- You are underweight, your body mass index (BMI) is less than 20 kg/m2 or your weight is below 57 kg
- You have been diagnosed with a deficiency of sex hormones. Early menopause in women (40-45 years), surgical menopause (removal of the uterus and/or appendages), prolonged amenorrhea (more than a year) in young patients; lack of testosterone in men are signs indicating the possibility of osteoporosis.
- Alcohol abuse and smoking are significant factors in the development of osteoporosis
- You do not like dairy products (the main source of calcium). Low dietary calcium intake contributes to the development of osteoporosis. The human body does not synthesize calcium on its own. We are entirely dependent on the supply of this mineral from the outside. And if this element (extremely important, involved in all life processes - from blood clotting to the transmission of nerve impulses) is not supplied enough, it is washed out of the bone tissue.
- You have at least one of the chronic diseases, such as diabetes, rheumatic diseases, inflammatory diseases of the gastrointestinal tract, celiac disease, chronic liver diseases, conditions after resection of the stomach, intestines, endocrine system diseases, kidney diseases, blood diseases.
- You are taking prednisolone or its analogues (for any disease), or are forced to take anticonvulsants, or are taking psychotropic medications.
(Based on materials from “Clinical Guidelines for Osteoporosis” edited by Prof. Lesnyak, Prof. Benevolenskaya, 2010).
You have discovered risk factors for osteoporosis, what should you do next?
Naturally, it is necessary to carefully assess the condition of bone tissue and the possible conservation of existing bone mass in order to avoid bone fractures. To do this, you need to consult a doctor and discuss a plan for further examination. It is a face-to-face conversation with a doctor that will allow you not to miss important examinations and avoid “unnecessary” tests.
The examination revealed osteoporosis. Nothing bothers me yet, there have been no broken bones, but do I need treatment?
If osteoporosis is established, it is necessary to both treat and monitor the condition of the bone tissue. Here we work “for the long term” in order to stop or minimize bone loss.
If a disease has appeared and still cannot be “completely cured”, but only slowed down, are there drugs against this disease?
Medicines for the prevention and treatment of osteoporosis exist. Basic therapy is necessary to prescribe calcium supplements, so that the intake of calcium into the body through medications and food is normal (1000-1500 mg per day). But you cannot limit yourself to just prescribing calcium supplements - this is not the main treatment of the disease; calcium is only one of the “building blocks in bone restoration.” Next, special drugs must be added to inhibit bone destruction or stimulate bone formation.
Only an endocrinologist can prescribe treatment, decide on the choice of drug, and monitor the tolerability and effectiveness of treatment.
I am receiving treatment for osteoporosis and “don’t feel anything”, how do I know if the medication is working and if it is helping?
It is not possible to track the effectiveness of treatment immediately; the bone gains mass quite slowly, so only after 1-2 years of treatment can we do a special x-ray examination and determine bone growth. Laboratory indicators of calcium metabolism can and should be performed repeatedly during treatment; they will also allow one to navigate the correct choice of therapy.
Is the fact that I am receiving treatment for osteoporosis a 100% guarantee that there will be no bone fractures?
Unfortunately, doctors are not able to give such a 100% guarantee, even with proper treatment. Bone fractures are possible both during treatment and after treatment. However, if we put patients with osteoporosis who were treated and those who did not receive treatment in one row, then in the first group (treated) the incidence of fractures will be significantly lower.
Denosumab
Denosumab (Prolia) is a human monoclonal antibody directed against receptor activator of nuclear factor-kappa B ligand (RANKL), which is a key mediator of the resorption phase of bone remodeling. The drug reduces bone resorption by inhibiting the activity of osteoclasts. Denosumab may be considered as a treatment option in some patients with renal failure because renal impairment does not significantly affect the metabolism or excretion of the drug.
Denosumab also increases bone mass in men at high risk of fracture who are receiving androgen deprivation therapy for nonmetastatic prostate cancer.
Denosumab in combination with teriparatide has been shown to increase BMD more than either drug alone.
Forecast
With proper treatment and monitoring of the patient, the progression of bone loss and the risk of fractures can be slowed down. Fractures of the vertebrae and peripheral bones that have already occurred cannot, of course, be corrected. But even stopping the progression of the disease during osteotropic therapy is considered a success in treatment. If it is possible to achieve an increase in bone mass, then this has an even more positive effect on the course of the disease.
Since in the treatment of such a serious disease as osteoporosis we work more “for the future”, trying to stop the progression of the disease, the effect of treatment is not noticeable quickly.
It is important for the patient not to quit treatment halfway, but to constantly be in contact with the attending physician to discuss the details of treatment.
This is only possible with competent supervision (the so-called “management” of the patient by the primary attending physician with the involvement of advisory assistance from doctors of other specialties, if required by a specific clinical situation). The prognosis with this approach to therapy is most favorable in relation to the patient’s quality of life and treatment of the disease.
Immobilization
Comfortable mechanical support of the spine should be provided and, in some cases, a thoracic orthosis should be used. The main reason for using a thoracic orthosis is the need to limit movement in the spine. The length of time a patient must wear a rigid orthosis depends on the individual patient. It is well known that immobilization promotes bone demineralization. In the early period of mobilization, it is necessary to perform deep breathing exercises, strengthening the pectoral and intercostal muscles and back muscles.
Parathyroid hormone
Teriparatide (Forteo) is a recombinant human parathyroid hormone (PTH) that acts as an anabolic agent for the treatment of osteoporosis. This drug is recommended for the treatment of women with postmenopausal osteoporosis who are at high risk of fracture and other treatments have not been shown to increase bone mass. This drug is also indicated for men with idiopathic or hypogonadal osteoporosis who are at high risk of fracture and have not responded to other medications. Teriparatide is also recommended for the treatment of patients with glucocorticoid-induced osteoporosis.
Before prescribing teriparatide, serum calcium, PTH and 25(OH)D levels should be monitored. Teriparatide should not be taken for more than 2 years.
Contraindications for the use of this drug:
- Previous hypercalcemia
- Severe renal failure
- Pregnancy
- Breastfeeding mothers
- History of bone metastases or bone malignancies
- Increased baseline risk of osteosarcoma (eg, Paget's disease, unexplained elevated alkaline phosphatase)
- Children and young people with patent epiphyses or previous radiation therapy to bone structures
- Monoclonal gammopathies of undetermined origin