Osteoporosis
(some call it “bone osteoporosis,” which is incorrect, since the word already contains the root “osteo,” which means “bone”) is a disease that is systemic and progressive, the main symptom of which is a decrease in density and disruption of the structure of bone tissue. Decreased bone density leads to an increased likelihood of developing fractures. A characteristic feature of osteoporotic fractures is their occurrence due to minor loads. It is the ease of fractures that is the main danger in osteoporosis, since extremely important bone structures of the human body - the spine, the femoral neck - can be susceptible to fractures. Fractures lead to immobility of the patient, which in old age is fraught with a significant number of complications - from the appearance of bedsores to the development of congestive pneumonia, which can be life-threatening. Few people know, but osteoporosis is now the fourth leading cause of death in people - it is second only to cardiovascular diseases, tumors and diabetes. And the main cause of death in patients with this diagnosis is a fracture of the femoral neck.
Causes of osteoporosis
- postmenopausal osteoporosis
in women (associated with low production of female sex hormones after menopause; the vast majority of women over 60 years of age describe its symptoms); - senile osteoporosis
is a broader concept than menopausal osteoporosis. The aging of the human body is accompanied by disruption of the internal structure of a significant number of organs, including bone tissue. It is the general aging of a person that causes a decrease in bone strength in old age; - glucocorticoid osteoporosis
develops in patients receiving long-term treatment with glucocorticoids - hormones of the adrenal cortex and their synthetic analogues, one of the side effects of which is disruption of the functioning of bone tissue; - secondary
is called
osteoporosis,
the cause of which is any chronic serious disease; Moreover, osteoporosis is one of the symptoms or complications of a primary disease - that is why it is called secondary, it seems to develop second. The cause of secondary osteoporosis can be diseases such as diabetes mellitus, malignant tumors, chronic kidney disease with the development of renal failure, some lung diseases, thyrotoxicosis (excessive thyroid function), hypothyroidism (reduced thyroid function), chronic hepatitis, parathyroid adenoma ( primary hyperparathyroidism). Also, the cause of its development may be a long-term deficiency of calcium and vitamin D in food - this disrupts the flow of calcium into the blood, and therefore the body’s needs for calcium are met at the expense of reserves in the bones. The result is osteoporosis.
Markers of bone resorption
To assess the effectiveness of osteoporosis treatment, resorption (reabsorption) markers are used. Their reduction under the influence of therapy begins after 2–3 weeks and reaches normal after 3–6 months. Beta-CrossLaps (C-terminal telopeptides) are formed during the degradation of type I collagen, which makes up more than 90% of the organic bone matrix. Its measurement makes it possible to assess the rate of degradation of relatively “old” bone tissue. With a pathological increase in reabsorption in osteoporosis and in old age, type 1 collagen degrades to a large extent. This leads to an increase in the level of its fragments in the blood.
Currently, there is evidence of the effect of gene polymorphism on bone mineral density. Allelic polymorphism of the bone remodeling gene network is being studied to identify osteoporosis susceptibility genotypes. Widely distributed enzymes are acid phosphatases. Their level is analyzed to determine the degree of bone reabsorption and monitor antiresorptive therapy.
To perform a modern and high-quality diagnosis of osteoporosis in the laboratory of the Yusupov Hospital, make an appointment with a rheumatologist by calling the contact center. After the initial examination, the doctor will prescribe those tests for osteoporosis and instrumental research methods that are most informative for establishing an accurate diagnosis for the patient. Examination for osteoporosis using densitometry allows us to detect a decrease in bone tissue mineralization at the preclinical stage of development of the pathological process.
Mechanism of development of osteoporosis
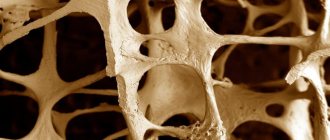
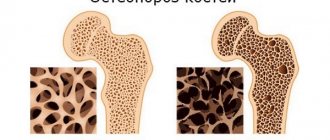
In bone tissue, two mutually opposite processes constantly coexist - osteogenesis (formation of bone tissue) and resorption (destruction) of bone tissue. Bone is a living structure that provides important support and organization functions to the human body. The human bone is a complex network of interconnected and intersecting bone beams, the direction of movement and strength of which make it possible to counteract the mechanical loads acting on the bone as a whole (the weight of the bone and muscles, the weight of internal organs and external loads, loads due to body position or acting on external acceleration, etc.). The nature of loads changes throughout a person’s life - body weight changes, height often changes with age, the nature of activity changes - all this forces the bone to adapt to new conditions and remain resistant to the forces acting on it. Bone beams are destroyed in one place and formed in another - this process is called bone remodeling and occurs constantly.
Special cells, osteoclasts, are responsible for the destruction of bone tissue during remodeling, which, like bulldozers, “bite” into bone tissue and destroy it. The formation of new bone beams is carried out by “mason” cells, osteoblasts, which form new bone tissue - the bone matrix, into which calcium salts are deposited, ensuring the strength of the constructed structure.
Increased bone resorption processes combined with weakened bone formation processes are the main cause of the development of osteoporosis. Osteoporosis occurs when old bone tissue is destroyed and new bone tissue is formed in insufficient quantities. Also, the reason for its appearance may be insufficient intake of calcium salts into the bones - in this case, the bone becomes soft and ceases to perform frame and supporting functions.
It should be remembered that the causes of osteoporosis are always directed against the formation of new bone, or “help” the destruction of bone tissue - both of which ultimately lead to fractures.
What tests are needed?
An accurate diagnosis of osteoporosis may require a large number of tests. Let's take a closer look at them.
Blood analysis
Allows you to assess the quality of calcium-phosphorus metabolism in the body, which indicates the processes of mineralization in bone tissue. This allows you to indirectly determine the absence or presence of osteoporosis
Biochemical blood tests
Allows you to accurately assess the condition of certain parts of the body.
Osteocalcin . The main non-collagen protein of bone, produced by osteoblasts and is a marker of bone tissue growth. It is done using RIA and ECLA methods. Exceeding the norm indicates postmenopausal osteoporosis, the initial stage of hyperthyroidism, renal osteodystrophy, and hyperparathyroidism.
The ECLA norms (ng/ml) are as follows:
| Age category | in men | among women |
| 18-30 years old | 23,4-71 | 10,9-42,7 |
| 30-50 years | 13,7-43 | 10,9-42,7 |
| 50-70 years | 15-47 | 14,8-47,2 |
RIA standards (ng/ml):
| Age category | in men | among women |
| 20-30 years | 11,1-36 | 8,8-39,3 |
| 30-40 years | 11-33,8 | 7,6-32 |
| 40-50 years | 5,1-34,4 | 7,9-35,9 |
| 50-60 years | 6,1-30,8 | 7,9-51 |
| 60-70 years | 8,7-29,6 | 13-56,1 |
Blood is donated on an empty stomach from 8 to 11 am. The cost of analysis is 460 rubles .
Phosphorus, inorganic
Did you know that...
Next fact
A high level of inorganic phosphorus indicates the development of osteoporosis. A component of the fraction of oxygen-soluble phosphorus, which is determined by metabolism, the level of remineralization in the bones and absorption in the digestive system. Determined by the molybdate colorimetry method.
An excessive value indicates hyperphosphatemia , which may be a sign of the possible development of osteoporosis, hypervitaminosis D, the process of healing and fusion of bones, bone breakdown due to oncology, and so on.
A reduced value indicates hypophosphatemia and indicates the possible presence of rickets in children, malabsorption, osteomalacia, hypercalcemia, gout, somatotropin deficiency, physiological phosphorus deficiency.
Cost - 220 rubles.
General calcium test
Determined by colorimetric method.
Normal phosphorus levels (mmol/l) depending on age are as follows::
| 0-10 days | 1,44-2,89 |
| 10 days -2 years | 1,44-2,17 |
| 2 years - 12 years | 1,44-1,77 |
| 12-60 years | 0,79-1,44 |
| over 60 years old | 0.91-1.33 in women and 0.75-1.19 in men |
Calcium norms (mmol/l):
| 0-10 days | 1,89-2,59 |
| 10 days -2 years | 2,26-2,74 |
| at 2 -12 years old | 2,19-2,69 |
| 12-18 years old | 2,11-2,54 |
| from 18 to 60 years old | 2,16-2,57 |
| from 60 years old | 2,04-2,56 |
Hypercalcemia may indicate thyrotoxicosis , hypervitaminosis D, initial hyperparathyroidism, oncology, milk-alkali syndrome, possible overdose of diuretics, immobilization hypercalcemia.
The rate below normal is determined in childhood rickets, as well as osteomalacia in adulthood, hypoparathyroidism, pancreatitis, and chronic renal failure.
Cost - 230 rubles.
B-Cross Laps
A marker that determines the level of mineral leaching. Thanks to the study, it is possible to determine the destruction of the first type of collagen.
Normal values are as follows:
| Age | among women | in men |
| up to 50 years | up to 0.580 | |
| up to 55 years old | up to 0.573 | |
| up to 70 years old | <1,008 | > 0,700 |
| over 70 years old | < 1,008 | < 0,854 |
Exceeding the indicator may indicate the onset of menopause in women, rheumatoid arthritis, hyperparathyroidism, and metabolic osteopathy. Price -1150 rubles .
Alkaline phosphatase
An enzyme whose high activity may indicate the development of bone diseases or liver diseases associated with blockage of the bile ducts.
The standards are as follows (El):
| Age | among women | in men |
| 3-6 years | up to 644 | |
| 6-12 years | up to 720 | |
| 12-17 years old | 448 | 936 |
| From 17 years old | < 105 | < 115 |
If exceeded, bone pathologies, rickets, osteomalacia, cancer, resorptive processes, and bone tissue healing are possible.
Cost - 220 rubles.
Hormone tests
Hormone tests may be needed to diagnose osteoporosis. By studying the active substances involved in mineral metabolism, changes characteristic of osteoporosis can be determined.
Tests determine the following hormones:
- Parathyroid hormone (660 rubles);
- Estradiol (410 rubles);
- Cortisol (270 rubles);
- Testosterone (890 rubles).
Urine tests
Inorganic phosphorus . Determines the content of phosphorus excreted through the kidneys in the urine. The indicator varies depending on the time of day and diet. With a normal diet, sudden changes can indicate pathologies. The norm is 13-42 mmol/day. Cost - 85-310 rubles.
Deoxypyridinoline in urine (DPID). Shows the content of collagen in bone and connective tissue and is the main marker of bone destruction. Normal (pyridine nmol/creatine mmol). For women, the norm is 3-7.4, for men - 2.3-5.4. The cost of the analysis is 1280 rubles.
Bone analysis for osteoporosis
The following methods are used to study bone density and pathological processes in it::
- Densitometry . The most common technique for analyzing bone structure. The mineral density of the tissue and the risks of fractures are determined in order to develop further treatment tactics. For this, an ultrasonic densitometer, which has a high level of sensitivity and accuracy, and x-ray densitometry, which determines the surface density of bone, can be used. Other methods are also possible, such as plain radiography, biochemical parameters, bone biopsy. The cost is determined by the part of the body, but on average it is 1000-3000 rubles.
Densitometry is used to analyze bone structure
- Radioisotope bone scan . It involves studying the structure of bone tissue by introducing a radioactive substance into the blood, which penetrates into the bones to the most affected areas. Features a high level of accuracy.
- Trephine biopsy . It is a study of bone tissue when it is removed from the bone with the preservation of the structure of the bone marrow that is located in it, and the determination of pathological changes in it. Involves the use of a special needle.
Video: “Diagnostics using densitometry”
Risk factors for osteoporosis
In childhood and adolescence, the process of bone tissue formation significantly prevails over its resorption. The older a person gets, the more bone destruction begins to prevail over its formation. The process of bone resorption intensifies especially in women after menopause. That is why osteoporosis in women is a typical and very common disease that occurs in old age.
There are factors that increase the risk of developing osteoporosis:
- female gender (women are much more susceptible to this disease than men);
- osteoporosis in blood relatives in the family (genetic predisposition to this disease is very important);
- age (as we mentioned earlier, with age the likelihood of developing the disease increases significantly);
- low mobility (immobilization, fixation of the patient’s limbs or body in case of injury, significant patient weight, mental disorders that make movement difficult - all these conditions are causes of the development of osteoporosis);
- drug therapy using glucocorticoids, high doses of thyroxine (a synthetic analogue of the thyroid hormone); bone tissue is also negatively affected by long-term use of aluminum-containing drugs - for example, antacids used to reduce the acidity of gastric juice during gastritis or peptic ulcers;
- the patient is overweight or underweight.
The patient cannot always change anything about the causes of osteoporosis, even if he understands that they can be dangerous. Indeed, neither gender nor age (the main risk factors) can be changed. However, there are factors that the patient can and should change in order to reduce the risk of developing such a dangerous disease. Smoking, excess consumption of alcohol and caffeine-containing drinks, lack of exercise, low consumption of foods rich in calcium (for example, dairy), little sun exposure, insufficient vitamin D intake - all of these factors can be changed, which is why they are called modifiable factors. risk.
Classification of osteoporosis
- Primary postmenopausal (occurs in women after menopause, when the amount of sex hormones that play an important role in the formation of bone mass decreases)
- senile (occurring in older people due to natural degenerative processes)
- juvenile (occurring in young people)
- idiopathic (with unknown cause)
Osteoporosis - symptoms and signs
Unfortunately, osteoporosis is a hidden disease that occurs for a long time without noticeable symptoms, and therefore its diagnosis is often delayed. Very often, the first symptom is a fracture - only after the fracture does the patient begin the examination and learn that the cause of the injury was osteoporosis.
At the same time, there are symptoms that make it possible to notice this disease at an earlier stage, before fractures appear. Patients are often concerned about changes in posture, stooping, decreased height, and accelerated destruction of dental tissue. Bone pain is one of the important signs to suspect the development of osteoporosis. Most often, pain occurs in the spine, hip bones, bones of the forearms and wrist. Often the pain intensifies with prolonged exposure to an uncomfortable position or mechanical stress. When there is a fracture or a sharp decrease in the height of the vertebrae, the pain is localized in the back, between the shoulder blades, and in the lumbar region. A symptom of calcium deficiency in the blood may be the appearance of convulsive muscle contractions.
Signs of osteoporosis
There are many clinical symptoms of osteoporosis, and not all of them relate directly to the skeleton.
There are common signs of osteoporosis, which include the following::
- Pathological fatigue, the cause of which is a systemic lack of calcium.
- Increased cramping, especially in the calves.
- With osteoporosis of the spine, lower back pain often occurs, both at rest and during movement.
- Brittleness and frequent splitting of nails.
- Diffuse myalgia or muscle pain.
- Frequent tachycardia.
- Protrusions and hernias in different parts of the spine.
- Scoliotic deformity of the spine, decreased height.
In patients with osteoporosis, the patient may experience a fracture even with very little stress. That is why timely diagnosis plays an important role.
Diagnosis of osteoporosis
Currently, diagnosing osteoporosis does not present significant difficulties. We only need to remember that traditional radiography is not able to assess the degree of development of osteoporosis, so other methods are used for diagnosis. Radiography allows one to only suspect the presence of osteoporosis based on a characteristic change in bone density on X-ray images, however, to plan treatment and assess the dynamics of changes in bone density, it is necessary to have quantitative information about the condition of the bone - i.e. it is necessary to be able to express bone density digitally.
Quantitative assessment of bone density is central to the diagnosis of osteoporosis. For this study, a special term was invented - “densitometry”,
those. density measurement. It is often written differently – “osteodensitometry”, emphasizing that bone density is measured.
Densitometry can be of three main types:
- X-ray densitometry (synonyms: DEXA, dual-energy X-ray computer densitometry);
- computed tomographic densitometry;
- ultrasonic densitometry.
With X-ray densitometry
X-rays of bones are taken at standard points (usually there are three standard points: femoral neck, lumbar spine, radius). After receiving the X-ray image, a special computer program calculates the bone density in the area of interest to the doctor and compares it with indicators characteristic of a healthy person of the same age (this is called the Z-index) or for a healthy person aged 40 years (this indicator is called the T-index ).
Diagnosis of osteoporosis
is carried out according to the deviation of the T-index from normal values:
- from 0 to -1 – normal bone density;
- from -1 to -2.5 – osteopenia (loss of bone tissue);
- less than -2.5 – osteoporosis.
With computed tomographic densitometry
Computed tomography is performed on a multislice tomograph, followed by calculation of bone density and comparison with the reference one. As a result, the density of 1 cubic centimeter of bone tissue in the study area is calculated, and the T- and Z-indices are calculated. The advantage of computed tomographic densitometry is its high accuracy and the ability to calculate bone tissue density regardless of the patient’s weight, the presence of adhesions, and metal structures, which can make it difficult to obtain results with conventional X-ray densitometry. The disadvantage of densitometry on a tomograph is the increased radiation exposure to the patient’s body.
Ultrasound densitometry
carried out by measuring the speed of passage of an ultrasonic wave through bone tissue. It has been proven that a decrease in bone density makes it looser and does not allow the bone to quickly conduct sound waves. The lower the bone density, the slower the sound wave travels along the surface of the bone. The ultrasound densitometer is equipped with special sensors for measuring the speed of ultrasound along the surface of the bones, and the built-in software of the device allows you to calculate bone density with the determination of T- and Z-indexes.
Ultrasound densitometry uses superficially located bones to determine density - the phalanges of the fingers, the radius on the forearm, the anterior surface of the tibia, the fifth metatarsal bone on the foot. The indicators calculated using ultrasound densitometry (T- and Z-indices) can be compared with similar indicators obtained from X-ray densitometry (that is, if osteoporosis was detected during X-ray densitometry, then ultrasound densitometry will reveal the same changes). At the same time, if the patient underwent X-ray densitometry during the first study, which revealed osteoporosis, and then treatment for osteoporosis was prescribed, then the second study should be carried out using the same assessment method, that is, also X-ray densitometry - only in this case will it be most reliable evaluate the effectiveness of treatment. Of course, the same rule applies to ultrasound densitometry - if treatment is carried out based on the results of the initial ultrasound examination, then monitoring of the treatment results should be carried out using ultrasound densitometry.
Diagnosis of osteoporosis using ultrasound densitometry has a number of advantages - ultrasound densitometry is not accompanied by radiation and can be carried out in a convenient environment for the patient for a fairly short time. The safety of the study is so high that ultrasound densitometry can be performed on both children and pregnant women.
In short, densitometry allows you to completely solve the problem of diagnosing osteoporosis, while any densitometry method is cheap, painless, and accurate.
Densitometry should be performed on all women aged 65 years
– following this simple rule could significantly reduce the incidence of fractures among older women. At the same time, densitometry is absolutely indicated for other groups of patients, including young patients. Among the indications for densitometry, the following should be noted:
- early onset of menopause;
- hormonal disorders in women, accompanied by estrogen deficiency, with the development of amenorrhea (absence of menstruation);
- low body weight (including due to a disease such as anorexia nervosa);
- presence of blood relatives suffering from osteoporosis;
- the presence of primary hyperparathyroidism (parathyroid adenoma);
- the presence of secondary hyperparathyroidism due to chronic renal failure;
- thyrotoxicosis (due to diseases such as diffuse toxic goiter, polynodose toxic goiter, toxic thyroid adenoma);
- decreased testosterone levels in men;
- long-term immobilization for fractures or other injuries;
- Itsenko-Cushing syndrome and disease;
- long-term use of glucocorticoids;
- the presence of rheumatic diseases (spondyloarthritis, rheumatoid arthritis), which are often combined with the development of osteoporosis.
It is important to understand that osteoporosis significantly complicates the treatment of joint diseases. Osteoporosis of the joints reduces the strength of the bones that articulate at the joint. Nowadays, endoprosthetics of hip and knee joints for arthrosis has become widespread. In this case, instead of a joint, the patient is fitted with a metal endoprosthesis, which is attached to the bones that form the joint. The stability of the resulting structure directly depends on the strength of the bones that bear the load of the endoprosthesis. The presence of osteoporosis of the joint creates preconditions for instability of the endoprosthesis, bone fractures in the area where the endoprosthesis is attached, and the development of severe complications. Therefore, diagnostics aimed at identifying osteoporosis is mandatory for all patients planning to undergo endoprosthetics.
Laboratory tests are of auxiliary importance in the diagnosis of osteoporosis. There are a number of markers (they are also called “osteoporosis tests”
), allowing to assess the severity of osteoporosis and the dynamics of its progression (osteocalcin, bone fraction of alkaline phosphatase, B-crosslaps, pyridinoline, etc.), however, their diagnostic significance is lower than the significance of densitometry.
When examining a patient with a suspected disorder of bone tissue density, important laboratory indicators are also mandatory:
- ionized calcium, parathyroid hormone, 25-hydroxyvitamin D;
- TSH, T4 St. (thyroid hormones);
- for women – sex hormones (estradiol, testosterone, etc.);
- for men – the level of free testosterone in the blood.
When is bone density testing required?
As mentioned above, the development of osteoporosis occurs gradually and with virtually no symptoms. As a result, the first sign is a bone fracture. In this condition, we can already talk about the pronounced course of the pathology. As a result, therapy is difficult.
Such negative consequences can be avoided if bone tissue is examined regularly. To determine its density, various methods and laboratory tests are used. This allows you to identify the problem at an early stage and start therapy in a timely manner.
Treatment of osteoporosis
Currently, we can confidently say that the treatment of osteoporosis
should be carried out in specialized centers with significant experience in managing patients with this pathology. Osteoporosis is a complex multifactorial problem, the development of which is caused by endocrine, age-related, and behavioral factors; therefore, doctors of several specialties (endocrinologist, rheumatologist, cardiologist, neurologist) often take part in the treatment of osteoporosis. At the same time, one doctor must be in charge, must be the “conductor” of this orchestra, must know how to treat osteoporosis and determine examination tactics, as well as decide which specialists should be involved in consultations if necessary. Most often, this doctor is an endocrinologist - it is endocrinologists who most often treat osteoporosis these days.
The North-Western Center for Endocrinology, as a specialized endocrinology center, provides comprehensive diagnosis and treatment of osteoporosis in St. Petersburg, Vyborg and other cities of the Leningrad region. The center's endocrinologists independently perform ultrasound densitometry on patients, which allows them to quickly establish a diagnosis and determine how to treat osteoporosis, as well as objectively evaluate the results of the therapy.
The main goals in the treatment of osteoporosis are increasing bone mass (by increasing the deposition of new bone tissue and reducing the destruction of existing bone tissue), preventing the development of fractures, reducing or completely eliminating pain, and ensuring optimal motor mode for patients.
Treatment of osteoporosis consists of several important and interconnected stages:
- First of all, the main diseases that cause osteoporosis are treated (thyrotoxicosis, hypothyroidism, Itsenko-Cushing syndrome and disease, hypogonadism, etc.);
- therapy aimed at increasing bone mass (calcium preparations, vitamin D, drugs from the bisphosphonate group - Fosamax, Forosa, Fosavance, Zometa, Aklasta, Bonviva, etc.);
- drugs aimed at reducing the intensity of pain.
In this article, we will not dwell in detail on therapy aimed at treating the underlying disease, if any, as this will take too much time. Let's discuss the modern concept of treating osteoporosis, aimed at increasing bone mass.
Currently, combination treatment of osteoporosis using:
- vitamin D preparations (aquadetrim, vigantol), or activated forms of vitamin D (alfacalcidol, alpha D3-Teva, etalfa);
- calcium preparations (containing calcium carbonate or calcium citrate);
- drugs from the bisphosphonate group.
If the first two groups of drugs (vitamin D and calcium) are aimed at increasing the formation of bone tissue by increasing the supply of calcium to the patient’s body, then the second group (bisphosphonates) is aimed at suppressing bone resorption (bone breakdown). The main effect of bisphosphonates is to block the work of osteoclasts, the cells responsible for the destruction of bone tissue. Currently, even very long-term, up to 10 years, use of bisphosphonates is considered safe. The cheapest and most studied drug from this group is sodium alendronate (Fosamax, Forosa), which is taken once a week. Other drugs that appeared later allow you to take them once a month, or once every few months. Bisphosphonates for osteoporosis are the main “strike force” of doctors, due to their effectiveness and safety.
Correctly selected treatment for osteoporosis allows you to increase bone density by 5-10% per year, which greatly reduces the risk of developing fractures. It should only be recalled that this therapy is long-term, designed to last for years of use. You should not think that treatment for one or two months will give any noticeable result.
Nikulin B.A., Ph.D., Medical Diagnostic Laboratory “Vera” The significance of the disease in modern society and medicine is determined by its prevalence among the population, the severity of the course and outcomes, the economic losses of the patient, family and society as a whole. Osteoporosis (OP) is a systemic metabolic disease of the skeleton, characterized by a decrease in bone mass and a violation of the microarchitecture of its structure, which reduces bone strength and increases the risk of fractures. According to WHO experts, AP today is one of the most common diseases, which, along with myocardial infarction, stroke, cancer and sudden death, occupies a leading place in the structure of morbidity and mortality of the population.
The results of numerous studies have convincingly proven that bone mass is the main determinant of the mechanical properties of bone tissue and determines 75-80% of its strength. The risk of fractures is directly related to the absolute values of bone mineral density (BMD) of the spine and femoral neck, and bone densitometry is the only reliable method to determine the degree of bone loss . The risk of fracture increases with age, which is mainly associated in older people with low BMD. The risk of hip fracture increases 2-3 times for every one standard deviation decrease in femoral neck BMD according to WHO criteria.
Pathogenesis of osteoporosis.
OP is now widely used as a model for fundamental research in the study of the molecular mechanisms of intercellular interaction. AP is a multifactorial disease, which is based on the processes of impaired bone remodeling with increased bone resorption and decreased bone formation. Bone tissue remodeling begins with resorption, carried out during the process of osteoclastogenesis with the formation of a resorption cavity. Osteoblasts (OB) “attack” the resorption cavity, where they build a new bone matrix for subsequent mineralization. Both processes of bone formation are closely related. Bone formation exceeds resorption during skeletal growth, and vice versa, resorption prevails during the subsequent period of human life. Both processes of bone formation are the result of close cellular interaction between OB and osteoclasts (OC), which originate from the precursors of different cell lines, namely: OB from mesenchial stem cells, OC from macrophage-monocyte blood cells.
Bone is formed by osteoblasts. Their main function is the synthesis of osteoid (protein matrix), which consists of 90-95% type 1 collagen, 5% osteocalcin protein and is subsequently mineralized with calcium and phosphate from the extracellular fluid. OB contain the enzyme alkaline phosphatase, carry receptors for parathyroid hormone (PTH) and calcitriol and are capable of proliferation. The mineral part of the bone consists of hydroxyapatite and amorphous calcium phosphate, which are non-covalently bound to organic matrix proteins
Bone resorption is carried out by osteoclasts. These are mobile cells. By releasing proteolytic enzymes and acid phosphatase, they cause degradation of collagen, destruction of hydroxyapatite and removal of minerals from the matrix. There is a correlation between the activity of tartrate-resistant acid phosphatase in the blood serum and the severity of resorptive processes in the bone.
Normally, both processes – formation and destruction – are balanced.
Timing of physiological bone remodeling.
| Bone resorption phase | 14-30 days |
| Switch-over phase (prostaglandin E2 is responsible for osteclast apoptosis) | 10 days |
| Bone formation phase | 90 days |
| Rest phase | 900 days |
The biological meaning of the phenomenon of bone remodeling is the adaptation of the mechanical properties of bone to constantly changing environmental conditions. The growth and renewal of the skeleton is accompanied by the regeneration of microdamages and maintaining the possibility of the transfer of minerals into the blood and back. In adults, osteoblasts produce slightly less bone tissue than is required. The consequence of this is a negative bone balance, which amounts to 0.5-1% annually. This phenomenon is known as “age-associated osteopenia.”
Significant progress in understanding osteoclastogenesis has been achieved with the recent discovery of new members of the family of tumor necrosis factors, their ligands and receptors (RANKL-RANK-ORG), which play a key role in the formation, differentiation and activity of OCs and may be molecular mediators of many regulators. The molecular basis of intercellular interaction can be presented as follows. RANKL (receptor activation of NF-kappa -ligand) is a transmembrane ligand expressed on the surface of OB. It is produced by osteoblasts and induces the process of differentiation and maturation of TC. RANKL is a major stimulating factor in the formation of mature osteoclasts. Therefore, increased RANKL expression leads to bone resorption and hence bone loss.
OPG-osteoprotegerin is an osteoclastic inhibitory factor , a glycoprotein widely expressed in various tissues, and is a potent inhibitor of bone resorption. OPG acts as an “imaginary” receptor for RANKL, blocks interaction with RANK and thus inhibits the formation of mature OCs, disrupts the process of osteoclastogenesis and bone tissue resorption. The balance between RANKL and OPG actually determines the amount of bone resorbed .
Recently, evidence has been obtained that T cells are involved in the regulation of bone metabolism. By inducing interleukin-17 (IL-17), which experimentally induced the expression of COX-2-dependent prostaglandin E2 and RANKL in the OB, the authors concluded that IL-17 is an important cytokine for osteoclastic resorption. However, the most important mediators for the action of various systems in the process of bone tissue remodeling, both normally and in AP, is currently the RANKL-RANK-OPG system .
Factors that play an important role in the pathogenesis of AP and its fractures: genetic, the formation of a low peak bone mass, loss of bone mineral density associated with age and postmenopause, violation of the architectonics of the bone structure, features of bone geometry (hip), injuries and falls, low nutrition calcium and vitamin D content, protein, etc., low physical activity, bad habits (smoking, alcohol). In secondary AP, the listed factors are joined by disease factors and the negative effects of medications (glucocorticosteroids, immunosuppressants, etc.), which cause bone loss and AP.
Reduced bone mass in AP, which is the main factor in its pathogenesis, is now considered as a consequence of the formation of an inappropriately low peak of bone mass in young age and intense age-related bone loss in old age. Genetic factors are the main determinants of peak bone mass. The contribution of genetic factors is 60-80% depending on the research methods (twins, families). Various genes are considered as candidates involved in the complex process of bone remodeling, formation and evolution leading to AP and fractures. Numerous comprehensive studies from various laboratories around the world are aimed at searching for specific genes, studying their polymorphism, function and interaction in the process of bone remodeling and AP.
Primary osteoporosis
Osteoporosis that develops during the postmenopausal belongs to the class of primary osteoporosis. It is known that a decrease in the secretion of sex hormones during menopause has a direct and indirect effect on the state of bone metabolism. A decrease in estrogen levels leads to a disturbance in calcium metabolism, which is accompanied by a decrease in bone mineral density. In addition, there is a suppression of osteoblast activity, which leads to the predominance of resorption over the processes of bone tissue formation. Postmenopausal osteoporosis accounts for 85% of the total number of primary osteoporosis.
Senile osteoporosis is the so-called second type of osteoporosis, in the pathogenesis of which an important role is played by a decrease in the absorption of calcium in the intestine, which is also facilitated by a deficiency of vitamin D caused by a decrease in its intake from food, a slowdown in its formation in the skin from provitamin D. Of greatest importance in the pathogenesis of senile osteoporosis has a deficiency of active vitamin D metabolites due to a decrease in its synthesis in the kidneys. In senile osteoporosis, the development of resistance to vitamin D plays a certain role - i.e. deficiency of 1,25(OH)2D receptors. These factors cause the development of transient hypocalcemia, which leads to increased production of parathyroid hormone. As a result of secondary hyperparathyroidism, bone resorption increases, while bone formation is reduced in old age.
Secondary OP
A serious medical problem is secondary AP, which occurs in various diseases: rheumatological, endocrinological, oncological, obstructive pulmonary diseases and bronchial asthma, diseases of the kidneys, thyroid gland, digestive organs, with immobilization and long-term use of a number of medications (corticosteroids, immunosuppressants, anticonvulsants, thyroid hormones, etc.).
A decrease in BMD in secondary AP often reaches the criterion values for AP (-2.5 SD or more according to the T-criterion) and provides grounds for making a diagnosis.
In postmenopausal patients with rheumatoid arthritis (RA), the development of AP occurred in the lumbar spine and femoral neck in 36%, in the forearm in 40%, and in patients with a preserved menstrual cycle - in 7 and 10%, respectively. The age of patients and the duration of menopause, the presence of risk factors, the activity and duration of the disease, the degree of functional insufficiency of the joints, the therapy performed (especially the prescription of glucocorticoids - GC) influence the amount of BMD loss and the development of osteopenia. When examining patients with endogenous hypercortisolism (Itsenko-Cushing syndrome and disease), AP was found in 91%, fractures of vertebral bodies or ribs - in 58%. AP in patients with bronchial asthma significantly aggravates the course of the underlying disease and increases the cost of treatment. According to Dr. I.A. Baranova, a decrease in BMD was detected in 42.8% of patients with bronchial asthma aged 20-49 years who had not previously received hormonal therapy, and the loss of BMD increased 5 times in moderate cases (53.5%) compared with mild (11%). In young and middle-aged patients who took GC at an average dose of 10.20±5.99 mg/day for 8-14 years, a decrease in BMD was found in 85%, and skeletal fractures were registered in 13%. As a reason for the development of AP in RA, a number of inflammatory diseases, and bronchial asthma, the direct effect of the disease itself on bone tissue is discussed, since a large number of common cytokines are known that are involved in the pathogenesis of the chronic inflammatory process and bone remodeling, as well as GCs, which are most effective for the basic therapy for a number of systemic diseases and at the same time occupying a leading place in the induction of secondary AP. The study of fractures in secondary AP remains an urgent task.
Steroid osteoporosis also belongs to the class of secondary osteoporosis and is caused by a pathological increase in the endogenous production of glucocorticoids by the adrenal glands or occurs with the introduction of synthetic analogues of corticosteroids used for the treatment of rheumatological, allergic, hematological, eye diseases, skin diseases, gastrointestinal tract (GIT), kidneys, liver . Steroid osteoporosis occurs in diseases characterized by increased secretion of corticosteroids by the adrenal glands (Itsenko-Cushing).
Biochemical markers of bone metabolism
They are studied to assess the rate of bone remodeling processes and diagnose osteoporosis with a high or low rate of bone turnover, disconnection or imbalance of its components: bone resorption and bone formation. The division of indicators into markers of bone formation and bone resorption is conditional. Together they reflect the resulting changes in resorption and bone formation, directed in one direction or another.
The most accurate markers of bone formation are currently recognized to be the study of the content of osteocalcin, type 1 collagen, osteoprotegerin ( OPG ), and Interleukin 17 in the blood.
of bone tissue resorption include urinary excretion of hydroxyproline, determination of pyridinoline, deoxypyridinoline and N-terminal telopeptide in fasting urine, activity of acid tartrate-resistant phosphatase, as well as determination of type 1 collagen degradation products ( Cross - Laps ) and RANKL (receptor activation of NF -kappa -ligand) in the blood.
The study of bone remodeling markers is useful for:
1. Dynamic assessment of bone metabolism;
2. Prognosis of bone loss (secondary prevention in case of detected osteopenia);
3. Prognosis of bone fracture;
4. Selection of patients for therapy;
5. Rapid monitoring of therapy.
The process of bone remodeling is regulated by many systemic hormones, cytokines, growth factors, and many local factors of bone remodeling have been identified. When studying OP, it is important to assess the parameters of mineral calcium-phosphorus-magnesium metabolism (the level of total and ionized calcium, phosphorus, magnesium, copper, zinc, vitamins C and K), which are involved in the process of bone formation.
Hormonal regulation of calcium levels in bone.
- parathyroid hormone - stimulates bone resorption by indirectly affecting osteoclasts;
— calcitonin – reduces the number of osteoclasts and inhibits their activity;
- estrogens - suppress the activity of osteoclasts;
— androgens – stimulate the proliferation of osteocytes and enhance the processes of bone synthesis;
- growth hormone and insulin-like growth factor 1 (somatomedin-C) - activate the process of bone synthesis by stimulating osteoblasts;
— insulin – stimulates the synthesis of bone matrix;
— thyroxine – stimulates osteoclasts, increasing bone resorption;
- corticosteroids - slow down the synthesis of collagen in bone tissue;
From the above it follows that studying the level of these hormones and bone remodeling markers at the early stage of osteopenia development, especially in secondary AP, will make it possible to predict and assess the likelihood of further bone resorption, prevent AP, and prescribe treatment.
Algorithm for laboratory assessment of bone remodeling.
| Index | Norm | Unit change | Is there osteoporosis (?!) | |
| Blood | ||||
| Parathyroid hormone | 7,0-53,0 | Pg\ml | >60 | |
| Calcitonin | 3,0-13,0 | Pg\ml | <3,0 >15,0 | |
| Calcitriol | 60,0-108,0 | pmol\l | < 60,0 | |
| Osteocalcin | 3,1-13,7 | ng\ml | < 3,0 >22,0 | |
| Alkaline phosphatase | 39-117 | Chalk | < 25,0 | |
| Tartrate-resistant acid phosphatase | 0-6,5 | Chalk | > 6,5 | |
| Total calcium | 2,12-2,65 | mmol\l | <� 2,00 | |
| Ionized calcium | 1,15-1,27 | mmol\l | < 1,0 | |
| Phosphorus | 0,9-1,32 | mmol\l | > 1,7 | |
| Magnesium | 0,7-1,15 | mmol\l | < 0,65 | |
| Albumen | 35-55 | g\l | < 30,0 | |
| Cross Laps | 0,1-0,6 | ng/ml | > 0,7 | |
| Collagen type 1 P1NP | 15,2-50,0 | ng/ml | < 10 > 100 | |
| Osteoprotegerin | M –165+/-5W –184+/-5 | Pg/ml | < 140< 160 | |
| Necrotic factor activator ligand RANKL | M –1.66-2.18W – 2.78-3.29 | Pmol/l | >2,5>3,5 | |
| Urine | ||||
| Total calcium | 2,5-7,5 | mmol\day | >10,0 | |
What diet is necessary for osteoporosis?
The diet for osteoporosis has no special secrets - you just need to ensure sufficient intake of vitamin D and calcium into the body, which are necessary for the formation of new bone tissue. The richest foods in calcium are dairy products, fish, cabbage (including broccoli), and various nuts. The main source of vitamin D in the body is fish (or fish oil). Significant amounts of vitamin D are produced in the skin when exposed to sunlight.
At the same time, when planning nutrition for osteoporosis,
It should be remembered that dietary “exercises” alone are not able to eliminate either calcium deficiency or vitamin D deficiency. In the vast majority of cases, diet is only one element of the treatment of osteoporosis and must be accompanied by taking calcium and vitamin D supplements in the form of tablets - this is the only way eliminate long-term chronic vitamin D deficiency.
Preparing for the study
For analysis, blood is taken from a vein. It must be submitted in the morning. You should not have breakfast before the examination. Dinner should be light: no fatty foods and alcohol.
You should also refrain from tea, coffee, juice, and milk for 12 hours. You should not exercise the day before the test. For reliable results, you need to spend 48 hours before the test as calmly as possible.
Tell your doctor if you have a chronic illness or if you are taking any medications. Many medications can affect PTH levels, and the doctor must be aware of the full picture in order to correctly evaluate the results of the study.
Complications of osteoporosis
The main and most dangerous complication of osteoporosis is fractures. The most dangerous fractures are fractures of the vertebrae and femoral neck. At the moment, it is “thanks to” hip fractures that osteoporosis is in fourth place among the causes of death in the world (second only to vascular diseases, oncology, and diabetes mellitus). Osteoporosis of the spine leads to the development of compression fractures even when exposed to minor loads (for example, when falling from your own height, or when landing after a jump). It is important to understand that immobility following a fracture of the spine or femoral neck in a significant number of cases ends in bedsores, congestive pneumonia, infectious complications, and thrombosis. Only early surgical treatment can reduce mortality from hip fractures, but, unfortunately, it cannot be performed in many elderly patients due to the presence of severe concomitant pathology. Osteoporosis of the spine cannot be corrected by surgery at all. That is why the only effective method of treating osteoporosis is early diagnosis and combined conservative therapy - this is the only way to avoid the development of fractures.
How to identify osteoporosis
Diagnosing osteoporosis can sometimes be difficult because in most cases the disease is asymptomatic and patients do not seek medical help. The most constant symptom of osteoporosis is pain in the sacral and lumbar spine, in the hip joints. Patients sometimes complain of pain in the ankle joints, pelvic bones, and ribs. Pain syndrome. intensifies with changes in weather and atmospheric pressure, and physical activity.
In the future, the pain becomes constant due to overstrain of the spinal ligaments and back muscles. During the period of a fracture of ribs or vertebrae, acute pain is localized at the site of the fracture. If these symptoms are present, doctors at the Yusupov Hospital conduct an examination for osteoporosis using densitometry.
The clinical picture of osteoporosis is characterized by the following features:
- Feeling of heaviness in the interscapular area, general muscle weakness;
- Decreased growth;
- Pain during palpation and tapping of the spine, tension in the long back muscles;
- Changes in the patient’s posture (appearance of stoop, “petitioner’s posture”, increased lumbar lordosis);
- A decrease in the distance between the lower ribs and the iliac crest and the appearance of small skin folds on the sides of the abdomen.
The most obvious symptom of osteoporosis is bone fracture. In postmenopausal osteoporosis, spongy bone loss occurs predominantly. Fractures of the vertebral bodies are extremely common. Traumatologists make a diagnosis of a vertebral body fracture based on the appearance of acute pain in the corresponding part of the spine, which sharply intensifies with movements and tapping on the spine, and X-ray data of the spine in two projections.
In women over 45 years of age, radial fractures also occur in a typical location. In later stages of osteoporosis, femoral neck fractures occur. Multiple rib fractures often occur with osteoporosis, which has developed as a result of long-term use of glucocorticoids.
Patients with age-related osteoporosis experience loss of both cancellous and cortical bone mass. Cervical fractures associated with cortical osteoporosis and intertrochanteric fractures due to loss of cancellous substance occur. In this case, the diagnosis of osteoporosis is made during X-ray examinations.
How is osteoporosis prevented?
Prevention should include several areas aimed at eliminating the previously listed risk factors for osteoporosis.
It is important to ensure sufficient intake of calcium and vitamin D from food - for this you should eat dairy and other calcium-rich foods listed above. You should reduce your consumption of alcohol and caffeine-containing drinks and foods.
There are a number of scientific studies showing that long-term use of calcium and vitamin D supplements for the purpose of prevention can reduce the risk of developing osteoporosis. Taking moderate doses of calcium with vitamin D for 3-4 years does not lead to side effects, but can improve bone density. It is enough to take calcium carbonate in a dose of 500 mg with 200 IU of vitamin D twice a day (for example, calcium D3 Nycomed, 1 tablet 2 times a day; or Calcemin-Advance, also 1 tablet 2 times a day). Taking calcium and vitamin D supplements is safe even if you have urolithiasis. However, the issue of preventive therapy should still be decided after consulting an endocrinologist.
Physical activity is the next factor to prevent the development of osteoporosis. Prevention using physical activity can increase the load on the bone and stimulate its strengthening.
For women during menopause, an important factor in the prevention of osteoporosis is the use of hormone replacement therapy, which allows them to “imitate” normal ovarian function for a long time and reduce the risks associated with the extinction of the natural hormonal function of the ovaries. Such therapy is also an effective factor in the treatment of osteoporosis, if it has already occurred. Of course, the selection of treatment is carried out by an endocrinologist.
One should not forget about the need to monitor thyroid function if the development of osteoporosis is suspected. To do this, it is enough to perform an ultrasound of the thyroid gland and pass a basic set of tests (usually for the first examination it is enough to donate blood for TSH, T4 free, and antibodies to thyroid peroxidase). When taking tests, do not forget about the need to monitor the level of ionized calcium annually! Timely detection of an increase or decrease in blood calcium levels greatly facilitates treatment.
Indications for testing for osteoporosis
Indications for diagnosis are any symptoms characteristic of the disease.
At the clinical examination stage, a specialist can identify a group that has an increased risk of osteoporosis. Symptoms may include kyphotic deformity in the thoracic spine and a clear decrease in the patient’s height compared to the previous visit. Also an indication for diagnosis is regular back pain.
Pay attention to who needs to be tested for osteoporosis. The following categories of people have a chance to get an appointment for diagnosis:
- Women with premature menopause.
- People genetically prone to osteoporosis.
- Frequent fractures in people under 45 years of age.
- Those who have diseases that provoke secondary osteoporosis.
- Those who have used certain drugs.
- Excessive thinness - exhaustion, anorexia, congenital thinness.
If you have two or more risk factors, the likelihood of osteoporosis increases by a third, regardless of age.
Useful video
Watch the video about the symptoms and treatment of osteoporosis:
Similar articles
- Prescribing a blood test for calcitonin...
The calcitonin hormone plays a rather important role, especially in children. It is no less important for women and men, because its functions are the production and proper removal of calcium, as well as other elements. What is the normal blood level? What if it's elevated? Read more - AT TPO analysis: why is it needed for adults, the norm...
A TPO AT test is performed to identify thyroid diseases. It is performed for both women and children. Deciphering the indicators, if it is elevated, will help identify pathologies. The norm for adults may vary even depending on training. Read more
- Indications for taking a blood test from a vein
The hormone cortisol plays an important role in protecting the body; it is also called the stress hormone. In women, men and children, it is responsible for the body’s response to external negative influences. If it is elevated or decreased, then it is worth talking about the disease. Read more
- Blood test for male sex hormones...
The androgen hormone plays a fairly significant role in the body. It affects sexual function and physique, as well as glucose absorption in women and men, although it is considered a male hormone. What hormones are classified as andrenogens? Why are the numbers increased? Read more
- Renin: blood test to determine levels in men...
In some situations, it is important to determine aldosterone and renin in men and women; a blood test will help with this. Preparation is important. What is the normal level of renin in the blood? What are the reasons for increased activity, how to reduce activity? Read more