Subchondral sclerosis of the joints is not a disease, but a diagnostic sign that is detected during an X-ray examination of the musculoskeletal system. If there are such changes in the image, the doctor needs to find out what kind of joint pathology it is a manifestation of. Only after this can effective treatment be prescribed.
If you are concerned about pain and stiffness in the joints, or a crunch appears when squatting, you should immediately contact the Yusupov Hospital. This may be a sign of degenerative processes of subchondral plasticity of the articular surface, which tend to progress. Doctors at the Yusupov Hospital will find out the cause and stop the progression of the pathological process.
Reasons for the formation of subchondral sclerosis
Bone disease does not develop suddenly, but develops over many years under the influence of causes that directly or indirectly affect the health of the musculoskeletal system. Factors that provoke the development of subchondral osteosclerosis are divided into two groups.
Endogenous (internal) factors include:
- Physiological aging of the body. Disruption of mineral metabolism, changes in the balance between “old” and “new” bone cells and other signs characteristic of an elderly organism lead to osteosclerosis.
- Hereditary nature of development.
- Endocrine disorders such as diabetes mellitus, hyperparathyroidism.
- Metabolic disorders, such as Wilson-Konovalov disease, gout.
- Vascular diseases acquired during life and worsening blood circulation in the extremities.
- Autoimmune diseases in which the body's own immune cells cause damage to the body. These include systemic lupus erythematosus and rheumatoid arthritis.
Exogenous (external) factors include:
- Injuries of the musculoskeletal system. With regard to the development of subchondral osteosclerosis, particularly dangerous injuries include fractures of the articular surfaces.
- Microdamages that occur in dancers, athletes, and military personnel under the influence of prolonged and excessive stress on the feet and knees.
- Excess body weight due to unhealthy lifestyle and overeating is one of the most destructive factors for the musculoskeletal system. It contributes to increased trauma and passive destruction of the skeleton.
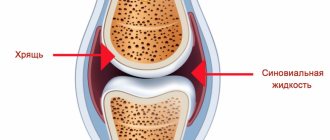
- Restriction of motor activity, which contributes to the weakening of the auxiliary structures of the supporting apparatus, disruption of the outflow or inflow of intra-articular fluid.
Prevention and healthy lifestyle
Of course, not everything is as bad as it might seem at first glance. To avoid trouble, you can simply follow some rules and avoid joint deformities, which in turn lead to loss of mobility.
- It is necessary to lead a healthy lifestyle and forget about your bad habits; in addition, you need to control your body weight.
Avoid possible hypothermia as much as possible.- For preventive purposes, engage in physical therapy or fitness, but do not overwork and do not get injured.
- Switch to proper nutrition, which can fully saturate the body with all useful substances.
- Contact specialists even if the most minor injuries have been sustained in order to begin timely treatment.
- Take preventive courses throughout the year to avoid unpleasant consequences.
That is why, based on all of the above, we can conclude that if even minor complaints from the joints or spine appear, you should immediately consult a doctor.
Stages of development of osteosclerosis
The course of subchondral bone diseases is divided into 4 stages. The transition from the initial stage to the last stage is accompanied by characteristic radiological symptoms.
- The initial stage is characterized by marginal osteophytes that form on the surface of the joints.
- Moderate subchondral sclerosis corresponds to stage 2. The radiograph shows a narrowing of the interarticular space. A focus of sclerosis under the joint is determined in the form of a clearing (negative in the image) against the background of relatively healthy bone tissue.
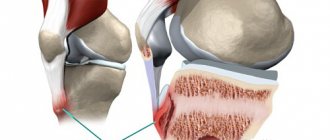
- At stage 3, the joint space is significantly narrowed, osteophytes increase in size, and damage the cartilage due to friction of deformed surfaces. Clinically, this is manifested by pain in the joints during movement and impaired mobility. Often at this stage a “joint mouse” appears - a fragment from an osteophyte or deformed surface that breaks off under the influence of additional traumatic factors. During arthroscopy, cartilage destruction is noticeable.
- The fourth stage is characterized by significant deformations of the joints with the formation of flat, incongruent surfaces. The interarticular space is not defined; osteophytes wedge into the bone, causing chips that are identified in the periarticular space. In the epiphyses of the bone, X-rays show an alternation of extensive foci of osteosclerosis with areas of osteoporosis. During arthroscopy, the cartilage is completely destroyed and is not visualized. A person loses the ability to move independently, feels constant pain, and is also unable to perform active and passive movements.
Treatment
Medication
Reference! Due to the fact that subchondral sclerosis of the knee joints is not independent, but is a symptom and addition to existing diseases that are associated with the spine or joints, treatment should be carried out exclusively in a full complex.
Initially, the specialist must determine what caused everything, and only after that prescribe medication. The course of such treatment must necessarily include anti-inflammatory drugs, antibacterial, hormonal and, if urgently necessary, painkillers.
Surgical intervention
If drug treatment does not bring successful results, experts often tend to take more drastic measures. That is, in case of severe deformities, surgical intervention is necessary in order to further restore the previous functions of the joints.
Currently, medicine has come quite far and therefore a wide variety of techniques are used in this area - from complete prosthetics of the affected joint to partial rehabilitation (everything will directly depend on the degree and neglect of the condition).
Light loads
Reference! The changes that occur against the background of the disease are detected during an x-ray examination and as a result of all this, a conclusion is made about how the inflammatory process proceeds.
If we compare this process with those that occur as a result of injuries or with periodic inflammation, subchondral sclerosis must be treated not only comprehensively, but also stimulating procedures must be used in the rehabilitation process.
Such loads, even at first glance not large, will at least normalize the ongoing processes in the tissues. That is why physical therapy exercises have such a beneficial effect not only on the general condition, but also on the treatment process.
Forms of subchondral osteosclerosis
Based on the prevalence of osteosclerosis in the human skeleton, the following clinical forms can be distinguished:
- The limited form looks like a focus of osteosclerosis against the background of healthy tissue within one anatomical formation.
- Common sclerosis affects more than 1 limb or anatomical area. Diseases that cause the common form include Paget's disease, Lehry's melorheostosis, and malignant neoplasms with metastases.
- Systemic osteosclerosis occurs under the influence of many factors and completely affects the skeleton.
Preventive recommendations
When diagnosing chronic pathology of the musculoskeletal system, it is necessary to undergo preventive treatment of the pathology.
To prevent the development of subchondral sclerosis, it is recommended to lead a healthy lifestyle with sufficient, but not excessive, physical activity. It is important to eat right, avoid stress, hypothermia and possible injuries. It is necessary to get rid of bad habits, and if the slightest signs of inflammation of the joint appear, conduct additional research on the condition and carry out treatment.
Subchondral sclerosis of the spinal column
The most problematic form of the disease is subchondral osteosclerosis of the endplates of the vertebral bodies. The development of sclerosis in one vertebra is often not felt by a person. However, when osteophytes gradually wedge and create pressure on the nerves coming from the spinal cord. Sclerosis of the spinal endplates affects different parts of the bone structure, causing the corresponding symptoms:
- Sclerosis of the endplates of the cervical vertebrae is the most insidious, as it disrupts important body functions. Compression of nerves and blood vessels leads to dizziness and ringing in the ears, vision decreases, deafness progresses, and coordination of purposeful actions is impaired. Bad prognostic signs are respiratory rhythm disturbances, increased heart rate and cardiac pain, decreased memory and attention. At the slightest movement of the neck, a dull or “shooting” pain appears. Subchondral sclerosis of the cervical endplates leads to decreased sensitivity and muscle strength. Severe leads to complete loss of movement in the arms due to compression and destruction of nerve fibers at the level of 4-7 vertebrae of the neck.
- Subchondral sclerosis of the endplates of the thoracic vertebral bodies is manifested by respiratory failure and noticeable distortion of posture. Pain in this area hinders movement.
- Sclerosis of the lumbar spine is manifested by shooting pain when bending and turning the body. As the disease progresses, weakness in the legs appears, due to which a person may lose the ability to move independently.
It is obvious that subchondral sclerosis of the endplates of the vertebral bodies requires timely treatment, without which there is a rapid development of neurological symptoms with severe motor and sensory disorders.
Osteosclerosis
Osteopetrosis
Osteopetrosis (marble disease, Albers-Schönberg disease) has two course options: with early and late manifestation.
Early familial osteopetrosis is inherited in an autosomal dominant manner. At the time of birth, macrocephaly and hydrocephalus are detected. Patients are stunted, the liver and spleen are enlarged. Over time, visual impairment and hearing loss occur due to compression of the cranial nerves. Due to impaired hematopoiesis, anemia develops. Pathological fractures are possible. X-rays reveal generalized osteosclerosis. The bones have a homogeneous structure, the medullary canal is absent. The metaphyses of the long tubular bones are club-shaped. X-rays of the skull reveal sclerosis and decreased pneumatization of the sinuses. Late osteopetrosis is inherited in an autosomal recessive manner and manifests itself with the same symptoms, however, the disease manifests itself at the age of 10 years or later and is characterized by a lower prevalence of osteosclerosis.
Dysosteosclerosis
Inherited in an autosomal recessive manner. The first signs appear in early childhood. Growth retardation, systemic osteosclerosis, impaired dental development caused by enamel hypoplasia, as well as optic nerve atrophy and bulbar palsy due to compression of the cranial nerves are detected. Radiographs of long tubular bones reveal osteosclerosis of the epiphyses and diaphyses with enlarged metaphyses with an unchanged bone structure. X-rays of the spine indicate flattening and sclerosis of the vertebral bodies. Osteosclerosis is also detected in the pelvic bones, skull bones, ribs and collarbones.
Pycnodysostosis
Pycnodysostosis is inherited in an autosomal recessive manner and usually manifests itself at an early age. Significant growth retardation is revealed. The patient's face has a characteristic appearance: the angle of the lower jaw is widened, the frontal tubercles are enlarged, the nose is beak-shaped, and hypertelorism is detected. Dental development is impaired. There is a pronounced shortening of the hands in combination with hypoplasia of the distal phalanges of the fingers. Pathological fractures are often observed. Radiographs reveal widespread osteosclerosis, most pronounced in the distal extremities.
Sclerosteosis
It is inherited in an autosomal recessive manner and manifests itself in early childhood. Characteristic symptoms are flattening of the face, hypertelorism, prognathia and flattening of the bridge of the nose. Cutaneous syndactyly is often observed in combination with nail dysplasia. Osteosclerosis is revealed on x-rays of the lower jaw, x-rays of the clavicles and the base of the skull. The long tubular bones are slightly changed: the medullary canal is preserved, the zone of osteosclerosis is clearly visible only in the area of the cortical layer.
Osteosclerosis of the joints of the upper limb
Subchondral osteosclerosis of the articular surfaces of the bones of the upper limb at the initial stage of the degenerative process is manifested by a crunching sound when flexing and extending the arm, which is not accompanied by pain. After a short period of time, a person experiences a sensation of a foreign body that interferes with normal movement in the elbow joint.
With severe deformation of the articular surface, the arm cannot be straightened, and any attempt to straighten the arm is accompanied by severe pain.
Treatment of osteosclerosis of the articular surfaces of the bone
Conservative treatment of osteosclerosis of the hip joint is possible only at the first and second stages. In the future, a series of surgical operations will be required to restore mobility. The situation is similar for the knee and ankle joints. But with the large joints of the bones of the upper shoulder girdle, everything is a little simpler. Here, treatment without surgery can bring positive results even at the beginning of the third stage of bone tissue destruction.
Modern methods of treating bone osteosclerosis are based on the principles of manual therapy. They include:
- reflexology, which triggers the process of regeneration of damaged tissues by influencing biologically active points located on the human body;
- massage and osteopathy, increasing blood supply and oxygen saturation of all tissues;
- kinesitherapy and therapeutic exercises, strengthening the muscular system and accelerating the recovery process.
In addition, physiotherapy, laser therapy and much more can be used. If you require treatment for osteosclerosis of the articular surfaces, we suggest that you sign up right now for a free initial consultation with our orthopedist. The doctor will conduct an examination and prescribe effective and safe treatment.
Osteosclerosis of the joints of the lower limb
Subchondral sclerosis of the hip joint is the most unfavorable localization of the degenerative process in old people. The development of osteosclerosis in this localization significantly increases the risk of hip fracture. If deformation occurs on the side of the acetabular surfaces, the patient experiences aching pain in the lumbar and pelvic area. When the pathological focus is localized in the femur, the sensation of pain occurs on the outside of the anatomical region of the same name. At first, the disease resembles subchondral sclerosis of the spine, but later signs of movement disorders in the hip joint appear, which confirms the true localization of the pathology.
Osteosclerosis of the knee joint begins with the appearance of characteristic “clicks” when moving fully. Pain is often caused by ligament sprains. The process of walking becomes more complicated, it is almost impossible to bend the leg and the person begins to walk on “straight” legs or limps. Sclerosis of the articular surfaces of the knee without treatment leads to a wheelchair.
Etiology and pathogenesis of subchondral sclerosis of articular surfaces
The main cause of joint sclerosis is age-related changes. It develops in the case of endocrine and immunological diseases, after injuries and due to congenital anomalies. When the cartilage, under which there is a strong plate, is injured or inflamed, bone tissue cells begin to rapidly divide, from which growths - osteophytes - are formed. If small formations are located at the edges, then the function of the joint is preserved. However, marginal growths can penetrate deep into the joint, narrowing its gap and preventing movement. Radiologists distinguish 4 main stages of subchondral sclerosis of articular surfaces:
- the first stage, in which only marginal growth of bone tissue occurs, and the joint space is not narrowed;
- the second stage, in which there are pronounced osteophytes and narrowing of the joint space;
- the third stage is characterized by the presence of outlined large growths, the gap is barely visible;
- the fourth stage, which is characterized by the presence of very large osteophytes, flattened bone surfaces, and a deformed gap.
Diagnosis of subchondral osteosclerosis
In diseases of the musculoskeletal system, methods that visualize the structure of the bone and joint are of particular importance. These include:
- Radiography. The simplest and most accessible method is widely used to diagnose subchondral sclerosis.
- Magnetic resonance imaging (MRI). Despite the general approval of this method in the study of the nervous system and parenchymal organs for the musculoskeletal system, the method is of less value. This is due to the fact that MRI visualization of soft tissues is better than hard ones, and therefore less informative for the study of bones.
- CT scan. For studying the musculoskeletal system, the method is informative. On CT, the hard tissue of the bone and joint is clearly visible and allows almost without errors to identify the area of subchondral osteosclerosis.
Laboratory tests and other methods are used to make a differential diagnosis with other diseases or in the case of an unclear clinical case.
Osteosclerosis of the elbow joint
In most cases, osteosclerosis of the elbow joint is an occupational disease for representatives of certain professions. These are painters, builders, tennis players, finishers, hairdressers and other people engaged in work associated with constant tension in the muscles of the forearm. At the muscle attachment points, the fascia becomes inflamed, which leads to disruption of blood microcirculation in the periosteum area.
Elbow osteosclerosis rarely leads to disability and can be treated quite successfully using conservative methods.