Osteomalacia (translated from Greek as softening of the bones) is a systemic disease of bone tissue in adults, which is characterized by a violation of the processes of mineralization of the new bone matrix. A similar condition in a child’s body, leading to disruption of the mineralization of cartilage located in the growth zones of bones, and leading to growth retardation and bone deformation, is called rickets.
For a long period of time, osteomalacia was considered a rather rare pathology. However, since the 60s of the last century, more and more research information has begun to appear confirming the increase in the incidence of this disease. Today, among patients with systemic osteoporosis, the number of patients with histologically confirmed osteomalacia is about 14-17%. In women, according to statistics, the disease is diagnosed 10 times more often than in men.
Despite the fact that in early childhood all infants receive vitamin D for preventive purposes, a certain group of children still develop rickets, and subsequently osteomalacia. This fact indicates a genetic defect in the process of bone tissue mineralization. However, along with the genetic factor, long-term adverse effects of the external environment on the human body also play a significant role in the development of osteomalacia.
Causes and mechanisms of development of osteomalacia
Osteomalacia is based on a lack of vitamin D in the body. In addition, surgical interventions on the stomach and intestines, chronic diseases of the pancreas and liver, and cystic fibrosis also lead to a defect in the process of bone mineralization.
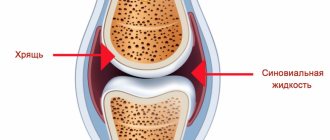
Bone mineralization is the process of saturating bone with calcium and phosphorus. For this process to occur effectively, sufficient levels of calcium and phosphate in the extracellular fluid and good alkaline phosphatase activity are required. If there is a disturbance in one or a number of factors necessary for bone mineralization, osteomalacia develops. The calcium content in the body is directly related to its absorption by the intestinal walls, as well as the reabsorption of calcium and phosphorus in the kidneys.
Depending on which link of phosphorus-calcium homeostasis is disrupted first, calcipenic
and phosphopenic
forms of osteomalacia are distinguished.
The most common causes of the phosphopenic form of osteomalacia include a decrease in the level of phosphorus in the blood due to a lack of vitamin D and secondary hyperparathyroidism, which develops against the background of pathology of the renal tubules with loss of phosphorus. Lack of phosphorus in foods consumed and exposure to toxins can also cause insufficient mineralization of bone tissue.
Disorders of calcium metabolism are most often acquired, and it is associated primarily with impaired metabolism of vitamin D caused by liver diseases, surgical interventions on the stomach and intestines, Crohn's disease, chronic pancreatitis and cholecystitis.
In addition, with chronic renal tubular acidosis, the neutral environment in areas of calcification is disrupted, which also leads to bone defects. The quality of bone calcification may decrease with slow or insufficient mineralization resulting from the influence of environmental factors, namely lack of insolation, abuse of vegetarianism, environmental pollution with heavy metals and aluminum, and taking certain medications (bisphosphonates, fluorides).
Occasionally, the cause of osteomalacia may be the presence of a disease such as hypophosphatasia, in which there is low activity of alkaline phosphatase in the blood and an associated slowdown in bone mineralization.
When should you take calcium during pregnancy?
The fact is that most of the calcium is concentrated in the skeletal system and teeth of the female body. If the concentration of this mineral in the blood decreases, then its gradual “washing out” begins. This causes bones to become more brittle and teeth may suffer from caries. It is as a result of a serious lack of calcium that during pregnancy you may simply have an irresistible desire to eat a piece of chalk.
During pregnancy, additional calcium intake may be needed in the following cases:
- severe and rapid tooth decay begins;
- increased fragility of nails and hair appears;
- there is a risk of premature labor;
- the development of preeclampsia in pregnant women begins, that is, late gestosis;
- early toxicosis manifests itself, which is severe;
- there is a risk of miscarriage;
- concerns about increased nervousness and anxiety;
- cramps appear in the legs;
- muscle tone increases;
- primary weakness of labor is observed.
Symptoms of ostemalacia
Based on the clinical picture, two forms of osteomalacia are distinguished - asymptomatic and manifest. Asymptomatic form of osteomalacia
characterized by the absence of obvious signs and complaints of patients, and disorders in bone tissue are detected by X-ray examination.
For manifest form of osteomalacia
Patient complaints of muscle weakness and bone pain are typical, and objectively it is possible to detect pain on palpation in the areas of bone projections. The most common localization of pain is the heels, pelvis, lumbosacral region, hips, lower legs, ribs. Pain increases with movement, lifting weights and other physical activities. Due to the fact that the volume of the bone matrix increases or completely replaces full-fledged bone tissue, its strength characteristics decrease, deformations, sprains and even tears of the periosteum are observed, which are accompanied by pain of a permanent or, less often, transient nature. With this condition of the bone tissue, slight physical stress, and sometimes even walking, can cause a fracture.
Muscle weakness, characteristic of osteomalacia, is also caused by a deficiency of calcium and phosphorus, which are involved in the transmission of neuromuscular impulses. Due to muscle hypotonia and atrophy, as well as severe pain, the patient’s gait changes - when walking, he sways from side to side (“duck” gait).
A decrease in the mechanical strength of bone tissue leads to the development of bone deformations, such as curvature of the spine, deformations of the chest and pelvis, aggravated by the presence of multiple single or multiple fractures, which most often affect only the periosteum, fuse over a long time and usually affect the neck of the femur, tibia , pelvic bones, carpal bones, metatarsals, etc.
Description of the disease
The essence of osteomalacia is as follows: during the formation of new bone tissue, its flexible base of collagen fibers (osteoid) is formed, but its mineralization, that is, strengthening with calcium (Ca) and phosphates, does not occur. The volume of bone tissue does not decrease, as with osteoporosis, but it cannot fully perform its function: under load, soft bones are deformed, and multiple fractures occur for no particular reason. The disease begins a chain reaction:
- The process of destruction of old and formation of new tissue is distorted;
- Due to the curvature of the bones, internal organs are displaced and compressed, which leads to disruption of their function.
Osteomalacia is found in 14% - 17% of patients with systemic osteoporosis.
Women are predominantly affected: for every 10 patients there is only one man. This is explained by a lack of Ca and vitamin D during pregnancy and reduced secretion of the hormone estrogen (participates in calcium metabolism) during menopause. Of the age groups, children and the elderly are most susceptible to the disease. Accordingly, there are four types of osteomalacia:
- Children's (youth);
- Puerperal (during pregnancy or breastfeeding);
- Menopausal;
- Senile.
The following parts of the skeleton are most often affected:
- Spine - in the elderly;
- Limbs - in children;
- Pelvic bones - in pregnant women:.
The childhood disease rickets is close to osteomalacia: with it, mineralization of cartilage in the bone growth zone does not occur.
Diagnosis of osteomalacia
Diagnosis of the disease consists of analyzing data from anamnestic, physical, laboratory and instrumental research methods. When collecting anamnesis from a patient, the specialist pays special attention to the duration of the disease, the presence of fractures of ribs, vertebrae, and long tubular bones that are not associated with significant trauma. When examining a patient by palpation, pain in the projection area of individual bones, curvature of the spine, deformation of the chest and pelvis, muscle weakness and muscle atrophy are revealed.
When analyzing laboratory data, depending on the results, one or another form of osteomalacia can be assumed. For example, when the level of phosphates in the blood decreases below normal, the concentration of calcidiol decreases and parathyroid hormone increases, it can be assumed that the root cause of osteomalacia is vitamin D deficiency, which can be nutritional or result from a violation of its absorption in the digestive tract. If the amount of phosphate in the blood is reduced along with increased phosphate clearance, primary phosphate loss or Fanconi syndrome can be suspected.
If osteomalacia is due to proximal renal tubular acidosis, the blood will show elevated levels of chloride compounds and hypophosphatemia, and subsequently hypercalciuria caused by the acidosis. With axial osteomalacia and fibrinogenesis imperfecta, none of the indicators of calcium, phosphorus and alkaline phosphatase are outside the normal range.
The most informative of the instrumental research methods is radiography. X-rays of adults show widening of the medullary canal and thinning of the periosteum of long tubular bones. In the metaphyses of the bones, instead of large bone cells, there are areas of a fine-mesh pattern. The vertebral bodies have a biconcave shape, and the discs are enlarged and have a double-contour pattern - “fish vertebrae”.
One of the most characteristic radiological symptoms of osteomalacia are cracks with sclerotically modified edges up to 5 mm wide, which are located symmetrically and perpendicular to the periosteum. These are the so-called Looser pseudofractures. They are usually located in the diaphysis of long bones, in the pelvic bones, shoulder blades, clavicles, and ribs. When scanned, they are identified as “hot” spots.
In secondary hyperparathyroidism, characteristic radiological signs are subperiosteal resorption of the terminal phalanges and terminal sections of tubular bones, bone cysts.
Due to the similarity of radiological signs, osteomalacia should be differentiated from systemic osteoporosis, which is more characterized by the presence of compression fractures. Before signs appear on an x-ray, a defect in bone mineralization can be detected using monophoton absorptiometry, which allows for a quantitative assessment of the calcium and phosphorus content in the bones of the leg and forearm. To conduct such a study, two-photon absorptiometry is performed in the vertebrae and necks of the femurs. In osteomalacia, the decrease in the amount of minerals does not depend on the age or gender of the patients, as well as on the form of osteomalacia.
The rate of bone formation and calcification can be assessed by histomorphometry using a double tetracycline label.
Treatment of osteomalacia
The main task in the treatment of osteomalacia is to eliminate the lack of vitamin D, phosphorus and calcium compounds, which in turn will help reduce bone damage, normalize their growth rate and correct existing deformities. Intramuscular or oral administration of vitamin D, especially its active metabolites and analogues - alfacalcidol or calcitriol, is considered effective in the treatment of osteomalacia of any form. The dosage of the drug is selected individually, taking into account laboratory data on the content of phosphates and calcium in the blood, and also depends on the cause that led to the development of osteomalacia. To correct calcium malabsorption in the gastrointestinal tract or in the renal tubules, calcium infusions are prescribed.
Treatment of osteomalacia is carried out throughout the patient’s life, however, the dosage of the drug is constantly adjusted downward. Experts recommend additionally prescribing vitamins B and C, which enhance the activity of vitamin D metabolites.
In addition, the diet of patients with osteomalacia must include foods containing sufficient amounts of calcium and phosphorus. Therefore, the daily menu must include milk and dairy products (kefir, fermented baked milk, cheese, cottage cheese). In addition, it is necessary to include a balanced amount of vegetables, fruits, meat and fish in the diet.
If conservative treatment carried out over 1.5-2 years does not restore the impaired mineralization process, surgical treatment of bone deformities is resorted to. Moreover, in the postoperative period, you should continue to take medications, in particular vitamin D replacement therapy, in order to avoid recurrence of bone fractures, the formation of false joints and other bone deformities.
In the vast majority of cases, when correcting the disease with vitamin D metabolites, calcium, vitamin C and group B preparations, a lasting therapeutic effect is achieved.