Sacroiliac joint dysfunction is an umbrella term used to describe pain in the sacroiliac joint (SIJ). This is usually due to impaired mobility in the joint (i.e. hyper- or hypo-mobility) or improper alignment of the articulating surfaces. SIJ dysfunction is the source of pain in 15-30% of people with mechanical low back pain.
SIJ dysfunction is a condition that is difficult to diagnose and often overlooked by doctors and physical therapists.
- The joint may be hyper- or hypomobile, which can cause pain.
- The pain is localized directly above the affected joint. Patients usually describe the pain as sharp, dull, aching, stabbing or shooting.
- They may also complain of sharp, stabbing and/or shooting pain that radiates down the back of the thigh, usually not below the knee.
- This pain can mimic radicular pain.
- People often complain of pain when sitting, lying ipsilaterally, or climbing stairs.
Clinically Relevant Anatomy
Pelvic ligaments
The sacroiliac joints are located on either side of the spine, between the two pelvic bones, which attach to the sacrum.
You can read more about KPS here.
- Several structures are involved in the maintenance and movement of the SIJ.
- The ligaments that support the SIJ are the anterior and posterior sacroiliac ligaments, the sacrotuberous ligament, the sacrospinous ligament, and the iliopsoas ligament.
- The SIJs are surrounded by some of the most powerful muscles in the body, but none of them have a direct impact on their mobility.
- The main function of the pelvic girdle is to provide shock absorption to the spine and distribute forces between the upper body and lower extremities.
Symptoms of arthrosis
Arthrosis of both the iliosacral and coccygeal-sacral regions is expressed predominantly by pain in the coccyx and sacrum (coccygodynia and sacrodynia). At the initial stage, there are dull and nagging pains that appear during exercise, and in particular static pain, after an uncomfortable position during night rest, or prolonged sitting. Simply rest and the pain will subside.
However, even in a calm state, a person feels discomfort and heaviness. Symptoms may temporarily disappear; exacerbations occur with high load on the sacral region, usually due to injury, hypothermia, or lifting heavy objects. In these cases, acute pain appears that occurs when the position of the body changes.
Like other types of arthrosis, osteoarthritis of the coccygeal-sacral and iliac-sacral region is constantly progressing, although the symptoms increase slowly. The pain becomes more prolonged, intensifying during bending and turning of the lower back.
Stiffness in the pelvic area is caused by muscle spasms, and not changes in the structure of the joints themselves. This area is innervated by the nerve endings of the lumbosacral junction. Therefore, if the disease appears against the background of an inflammatory reaction or is complicated by this condition, then the nerve roots begin to be involved in the process. Moreover, pain begins to radiate to the stomach, lower back, and legs. Very often there is swelling in the area of the lower spine.
If the joint between the coccyx and the sacrum is affected, problems with stool are typical. During iliosacral arthrosis, urination becomes more frequent, and men may experience erectile dysfunction.
Coccydynia and sacrodynia in some cases are caused not only by arthrosis, but also by pathologies near organs, pathogenic processes in soft tissues, and gynecological diseases in women. Pain in the tailbone is often a long-term result of injury. Pathologies and abnormalities in the structure of the lumbar discs can lead to the appearance of pain in the sacrum.
Etiology
It is often difficult to determine what caused the joint damage.
On March 15-20, a seminar by Georgy Temichev “RehabTeam. Block_1 (Lumbar, Thoracic, Pelvis).” Find out more...
- One of the most common causes of problems in the SIJ is injury. The force from this type of injury can damage the ligaments around the joint. A tear in these ligaments is characterized by too much movement in the joint, and over time this can lead to degenerative arthritis.
- Pain may also be caused by an abnormality of the sacrum, which can be seen on x-rays.
- Pregnant women are more likely to develop SIJ syndrome. Female hormones are released during pregnancy, relaxing the sacroiliac ligaments. This stretching causes changes in the SIJ, making it hypermobile. After the fifth decade of life, the SIJ grows together.
Causes of the disease
Movement in tight iliosacral joints is limited. Moreover, they are subject to significant load, since they ensure the natural position of the body. Osteoarthritis of the iliosacral joint can be caused by injury, as well as weakening of the muscles that support the vertebrae.
Increased load on the joint, endocrine and metabolic disorders, inflammation, and age-related changes can also cause symptoms of arthrosis of the sacrococcygeal joint. The sacrococcygeal joint is supported by four ligaments. It is due to this joint that in women during childbirth the tailbone moves back. In its normal state it is almost motionless. However, it is here that arthrosis of the sacrococcygeal region can develop. This disease can be caused by:
- abnormal development of the spine (appearance of clefts, lumbar lumbarization, sacralization) or scoliosis;
- injuries of the sacral region, usually bruises;
- excessive load on the sacrococcygeal region due to pregnancy, significant weight, and inactive lifestyle;
- destruction of joint tissue during autoimmune pathologies;
- inflammatory reaction against the background of viral diseases.
Epidemiology
Approximately 90% of the population will suffer or complain of some form of low back pain at some point. It is estimated that 10 to 25% of these patients experience SIJ pain. Most SIJ pathologies affect the adult patient population.
- The posterior sacral branch innervates the SIJ, and when compressed or inflamed, it is a source of intense pain.
- Most people suffering from SIJ pain are adults. This disorder most often occurs in people who lead a sedentary lifestyle.
- In general, obese patients are more likely to suffer from SIJ pain.
- This disorder occurs in both men and women.
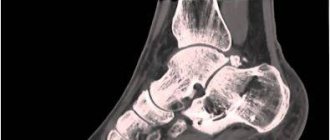
Preparing for MRI of the sacroiliac joints
Before examining the sacroiliac joints, you can adhere to your usual diet and physical activity, and lead your usual lifestyle. There is a small exception to this rule if a study involves the use of a contrast agent.
Sometimes the administration of the drug is accompanied by autonomic reactions (nausea, vomiting) that occur with a full stomach or on an empty stomach. On the day of the procedure, you should not overeat, and 30-40 minutes before the examination it is recommended to have a snack of fruit or a sandwich.
Extremely rarely, gadolinium (the substance on which the contrast agent is made) can cause allergic reactions. You need to tell your radiologist in detail about any drug intolerances you have. According to indications, an allergy test for gadolinium is prescribed. In people with underlying severe renal failure, the drug may worsen the course of the disease.
Therefore, in the presence of this pathology, preparation for MRI of the sacroiliac joints using amplification includes a study of blood creatinine levels.
Contraindications to performing MRI with a contrast agent are:
- enhancement study performed less than 36 hours ago;
- allergic reactions to gadolinium;
- chronic renal failure stage IV-V;
- severe bronchial asthma
- history of polyvalent drug intolerance.
It is necessary to bring medical documentation related to the disease of the sacroiliac joints to the examination:
- referral from the attending physician;
- discharge from hospital;
- data from previous studies, such as MRI, CT, if they were performed in another medical institution.
This will help the doctor make the right conclusions. If metal structures or artificial joints are installed in the body, you must submit a certificate from the hospital where the surgery was performed indicating the material from which the structure was made or stating that there are no contraindications for MRI. The restriction does not apply to dental braces and implants.
It is strictly forbidden to bring into the room where tomography is performed:
- watch;
- Hearing Aids;
- credit cards (they are damaged by magnetic fields), etc.
The MRI machine makes loud noises when operating, so don't be alarmed. You should use headphones to reduce the noise level. At the end of the procedure, you can immediately return to normal life if sedatives were not used due to claustrophobia. Do not drive while using sedatives. To find out how long you need to refrain from driving, consult your doctor.
A modern high-field tomograph is the key to high-quality research results.
Clinical picture
Symptoms of SIJ syndrome are often difficult to distinguish from other types of low back pain. The most common symptoms include:
- Lower back pain.
- Pain in the hips.
- Discomfort when sitting for long periods of time.
- Local tenderness of the posterior surface of the SIJ (next to the posterior superior iliac spine).
- Pain occurs when there is mechanical stress on the joint, for example, when bending forward.
- No signs of neurological deficits/nerve root tension.
- Aberrant movements of the SIJ.
- The joint may be hyper- or hypomobile, which can cause pain.
- The pain is usually localized directly above the SIJ.
- Patients may complain of sharp, stabbing and/or shooting pain that extends down the back of the thigh, not below the knee.
- The pain may mimic radicular pain and therefore be misdiagnosed as radicular pain.
- Patients often complain of pain when sitting, lying ipsilaterally, or climbing stairs.
Differential diagnosis
SIJ syndrome is a controversial diagnosis, so SIJ pain and injury are commonly overlooked. This condition is often defined as dysfunction (a term that serves as an umbrella term for various conditions).
Differential diagnosis should include:
- Radicular pain.
- Piriformis syndrome.
- Ankylosing spondylitis.
- Lumbar facet syndrome.
- Spondyloatropathy.
- Greater trochanteric bursitis.
- Fracture of the femur.
- Hip overload syndrome.
Symptoms of arthrosis
- abnormal development of the spine (appearance of clefts, lumbar lumbarization, sacralization) or scoliosis;
- injuries of the sacral region, usually bruises;
- excessive load on the sacrococcygeal region due to pregnancy, significant weight, and inactive lifestyle;
- destruction of joint tissue during autoimmune pathologies;
- inflammatory reaction against the background of viral diseases.
Diagnostic procedures
To identify SIJ dysfunction, it is necessary to conduct a comprehensive study.
- The hip joints (including range of motion) should be assessed for symptoms. This also includes performing a Trendelenburg test. Palpation over the SIJ often causes discomfort. Differences in leg length may also be a cause of SI joint pain (leg length should be measured in all patients with suspected SI joint dysfunction).
Physical therapists use a variety of orthopedic provocation tests.
- Gaenslen test.
- Sacral trust test.
- Thigh trust test.
- Distraction test.
- FABER test.
- Yeoman test. The patient lies in a prone position with the knee bent 90° degrees. The examiner lifts the bent leg by hyperextending the hip. This test places stress on the posterior structures and anterior sacroiliac ligaments. Pain indicates a positive test.
- Gillette test. The patient is standing. The examiner's thumbs are placed under the posterior superior iliac spine and S2 (fingers parallel to each other). Then the subject should bend one leg at the knee and hip joints 90 degrees. If the VEPO on the side of the bent leg moves upward, then the test is considered positive.
- SIJ compression test. The patient is positioned in a supine position. The examiner applies pressure to the wings of the ilium with both hands. With the arms crossed, the examiner can add lateral compression. Pain is a sign of strain in the anterior sacroiliac ligaments.
Laslett cluster of tests
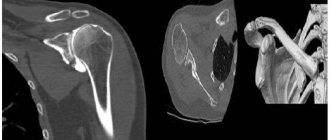
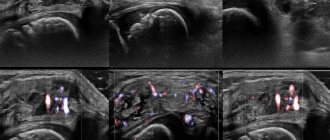
CT and MRI are often used to confirm the diagnosis. Ultrasound-guided anesthetic injections are a good tool in diagnosing SIJ pathologies.
Physical therapy
The goal of the first stage of treatment is to reduce inflammation with ice packs and anti-inflammatory medications.
The second goal is to improve mobility through mobilizations, manipulations, or exercise therapy.
If there are complaints of instability, it may be helpful to use a sacroiliac belt for temporary pelvic support, as well as progressive stabilization training to improve motor control and stability.
If the SIJ is severely inflamed, a sacroiliac belt can also be used.
Postural and ergonomic recommendations will help the patient reduce the risk of re-injury.
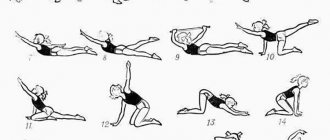
Core stability
Exercise is a core component of a SIJ pain management program. Exercises that focus on improving core stability have been shown to be effective in this case.
Stabilization exercises
- In order to concentrate on contracting the local muscles of the lower back (without involving the global muscles), it is necessary to improve proprioception and motor control. It is also necessary to work in an isometric mode with two main stabilizers - the transverse abdominis and multifidus lumbar muscles. These muscles need to be trained at low levels of maximal voluntary isometric contraction. It is important to maintain controlled breathing and neutral lordosis during resistance exercise. The following principles must be followed: inhale and exhale, pull the lower abdomen below the navel carefully and slowly, without moving the upper abdomen, back or pelvis. In addition, the physical therapist may palpate the multifidus muscles. This is necessary to ensure effective muscle activation.