Compared to other areas of inflammation, arthritis of the clavicular bone is relatively rare. For every 100 cases of registered joint pathologies, there are only 3 visits to the acromial clavicular ligament.
However, clavicular arthritis (also known as acromioclavicular arthritis) cannot be ignored. If we talk only about damage to the clavicular bone, then we are talking about a specific form of the disease - a form of arthritis that is associated with age-related changes, osteoarthritis.
Causes of the disease
A person can raise his arms up using the upper limb girdle, which consists of the shoulder joints, shoulder blades and collarbones. Together they form mobile, active joints. Thus, at the junction of the semicircular part of the scapula (acromion) and the proximal end of the clavicle, the acromioclavicular joint is formed. It includes cartilage, ligaments, surrounding soft tissue. It is noteworthy that there is very little synovial (intra-articular) fluid in the AC joint capsule.
Specific loads on the upper body cause instability of the ligamentous apparatus of the joint, which in turn leads to a violation of the integrity of the cartilage tissue. At the next stage, pathological growth of bone cells occurs and growths (osteophytes) are formed. The combination of pathogenetic factors leads to an inflammatory, destructive process – AC joint arthrosis.
Experts have identified a category of patients among whom arthrosis of the acromioclavicular joint is most often diagnosed:
- weightlifters working with heavy weights;
- bodybuilders who load the belt of the upper limbs in order to sculpt the muscles of the back, arms, and chest;
- track and field athletes competing on specific apparatus – uneven bars, rings, horizontal bar;
- boxers;
- miners;
- welders;
- movers;
- blacksmiths.
The main factors provoking the onset of degenerative changes are:
- heavy physical labor associated with lifting and carrying heavy objects;
- prolonged forced raising of arms;
- congenital anomalies in the development of bone and cartilage tissue associated with weakness of ligaments, muscles, and improper formation of chondrocytes;
- injuries to the collarbones and shoulder blades;
- surgical interventions in the articulation area
- placing your arm bent at the shoulder under your head while sleeping.
Long-term loads on the acromioclavicular joint lead to the replacement of cartilage tissue with bone. The formation of osteophytes causes a decrease in motor amplitude. The pathological process of arthrosis takes a long time without specific symptoms. The appearance of pain indicates an advanced form of the disease.
If the root cause of acromioclavicular arthrosis is not established, they speak of the primary form of the disease. In this case, the pathological process spreads throughout all osteochondral joints. Primary ACS is most often transmitted genetically.
The secondary type of ACS is spoken of when the main pathogenetic factor of the disease is known:
- pathologies of the endocrine system;
- violation of metabolic processes;
- multiple microtraumas;
- progressive osteoporosis;
- excess weight;
- lesions of the articulation elements, acquired or congenital
RECOVERY AND PREVENTION OF RECURRENCES
The treatment of any arthritis, including pathology of the joints “connected” to the clavicle bone, is based on three directions:
- Medication. Analgesics and anti-inflammatory (non-steroidal) medications will help relieve pain and help you get a good night's sleep.
- Severe pain in the anterior part of the clavicular bone often occurs at night; against the background of fatigue and lack of sleep, the patient may develop psychological instability. To normalize his condition, antidepressants and sedatives are prescribed.
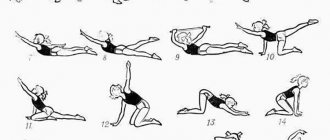
- A set of exercises is recommended both during the treatment of arthritis and during remission. Exercise therapy strengthens the affected area, triggers natural regenerative processes, and restores the mobility of the clavicular bone.
- Advanced clinics practice manual therapy, treatment with warm compresses and exposure to bioactive points for arthritis of the clavicular bone.
- Particularly severe cases require radical treatment with arthroplasty or surgical cleansing of the inflamed areas.
The prognosis for active treatment of arthritis in the case of damage to the clavicular bone is good. To prevent relapse, experienced rheumatologists recommend cryotherapy, swimming and self-care. If arthritis is triggered by frequent microtraumas at work, it is advisable to change jobs.
Signs of acromioclavicular arthrosis
At the beginning of destruction, a person does not notice any unpleasant symptoms of acromioclavicular arthrosis. The clinical picture of the pathology appears years later. Sometimes symptoms appear singly, but very often the problem is signaled by several specific signs:
- Pain syndrome. Pain appears first. At the beginning of the pathological process, it makes itself felt after physical activity and training. The patient experiences short-term pain that goes away on its own. Without therapy, the pain becomes persistent and is not relieved by analgesics.
- Crunching in the shoulder joint. In a healthy joint, a crunching sound (crepitus) may occur. With ACS, it occurs along with pain.
- Deformation, swelling. The growth of bone processes entails a change in the shape of the joint. The shoulder swells, the color of the skin over the joint changes, and the local temperature rises.
- Impaired motor function. As the disease progresses, the patient cannot perform the usual movements or move his arm behind his head. Most patients have problems getting dressed.
The patient's general condition is rapidly deteriorating. Due to the inability to take a comfortable position in bed, insomnia develops. The pain intensifies when lying down. Somatic symptoms cause changes in the central nervous system. Patients become irritable and prone to depression.
Results and discussion
Analysis of case histories of patients with purulent arthritis of GCS indicates significant diagnostic difficulties, not only at the early stage of the disease, but also when the inflammatory process spreads to surrounding tissues. The difficulty of diagnosing the disease was determined by two main reasons: the rarity of the disease and the lack of familiarity of specialists with it. In most cases, it was possible to suspect a pathological process in the GCS even during a clinical examination of the patient, and instrumental diagnostic methods such as CT, MRI and osteoscintigraphy make it possible to establish the stage of the disease and the extent of the pathological process to surrounding tissues (Fig. 1). An examination of hospitalized patients showed that such a traditional method of diagnosing diseases of bones and joints as plain radiography is of little information. The method of choice for instrumental diagnosis of RGC lesions was multislice CT with multiplanar and three-dimensional image reconstructions (Fig. 2 , 3)
. The study should be performed immediately upon hospitalization of such patients in the department of purulent surgery. MRI is highly informative in diagnosing this disease.
Rice. 1. Computer tomogram with multiplanar image reconstruction.
Rice. 2. Computer tomogram with multiplanar image reconstruction.
Rice.
3. Computer tomogram with 3D image reconstruction. The inflammatory process in the area of the GCS can go through several stages in its development: serous arthritis, purulent arthritis (often with the formation of periarticular phlegmon), osteoarthritis (with destructive changes in the area of the clavicle and sternum) (Fig. 4).
Rice. 4. Computer tomogram.
The effectiveness of conservative treatment in the form of antibacterial therapy is observed only in the early stages of the disease (serous arthritis). Acute purulent arthritis, which, due to the peculiarities of the anatomical structure of the GCS, is accompanied by a rapid transition of the purulent-inflammatory process to the surrounding tissues, requires emergency surgical intervention. The operation, as a rule, consists of opening and draining paraarticular phlegmon and purulent leaks. Resection of the GCS in the presence of bone-destructive changes in the latter is performed in the second stage after 2-3 months. Patients hospitalized with a picture of chronic osteoarthritis underwent planned resection of the GCS.
Analysis of the bacterial flora most often indicated the presence of Staphylococcus aureus (38.8%), including polyantibiotic-resistant - 16.6% (among all microorganisms of this species). Streptococcus
pneumonia
was identified in 1 (5.5%) patient ; in the remaining cases (38.8%), it was not possible to identify the microflora from the foci of purulent inflammation.
Long-term results of treatment of infectious arthritis with GCS were monitored in 10 patients for up to 6 years. In one patient who had serous inflammation, no relapse of the disease was noted after conservative treatment. In 3 out of 5 patients operated on for panarthritis with periarticular phlegmon, the surgical wound healed by secondary intention, and they had no subsequent complaints. The remaining 2 patients developed purulent fistulas in the paraarticular area, but they decided to refrain from further examination and treatment. In 4 radically operated patients who underwent GCS resection for osteoarthritis, no relapse of the disease was observed. In 2 of them, in the long-term period, there was a restriction of movements of the upper limb on the side of the operation, especially during its abduction.
Thus, infectious arthritis of the sternoclavicular joint is a rare surgical disease characterized by hematogenous infection of the joint predominantly by Staphylococcus aureus. The methods of choice for instrumental diagnostics are CT and MRI. Early diagnosis of the disease at the stage of serous inflammation allows for antibiotic therapy with good results. Given the rather high probability of the presence of multidrug-resistant Staphylococcus aureus, the use of appropriate antibiotics is preferable. With the development of purulent arthritis with the formation of periarticular phlegmon, emergency surgery is required to open and drain the abscess. Resection of the sternoclavicular joint is indicated for the development of osteoarthritis and is performed outside the period of acute inflammation.
Diagnostic methods
The earlier the diagnosis of acromioclavicular arthrosis is made, the greater the patient’s chances of slowing down the process and maintaining quality of life. To reach a correct conclusion, you will need a set of measures:
- examination by a specialist with mandatory palpation of the joint;
- CT scan is necessary to determine changes in the structure of bone tissue;
- MRI – shows the condition of cartilage, ligaments, bone elements;
- Ultrasound of the shoulder joint;
- radiography - shows a narrowing of the gap between the distal part of the scapula and the collarbone;
- blood test for markers of autoimmune disorders;
Evaluation of the examination results is the basis for prescribing one or another type of treatment and the use of physiotherapeutic methods.
Anatomy of the clavicle joints
The clavicular joint is a joint formed by the clavicular notch and the sternal end of the clavicle. Hyaline cartilage covers the surfaces of the bones, but does not ensure a complete match in the shape of the two elements. This causes the fact that over time, movements become more difficult and sometimes even impossible.
Nature helps solve this problem in ways available to it. An intra-articular disc, located between two bones, is attached to the capsule and divides the joint into two parts, thereby eliminating bone friction and deformation.
The surface of the joint is covered with a dense capsule and is also sealed with fairly strong ligaments:
- sternoclavicular;
- costoclavicular;
- interclavicular.
All ligaments are different in shape and function; they limit the movement of the collarbone in a certain direction.
Stages of disease development
Traumatologists distinguish four stages of acromioclavicular arthrosis:
- Stage I – not accompanied by any symptoms. Patients note discomfort and some pain when pressing on the area of the acromioclavicular joint, when performing sharp swings of the arms. Patients ignore the first symptoms, which is why the cartilage tissue continues to thin out - the pathology begins to progress;
- Stage II – the patient constantly experiences pain in the affected joint. The painful sensations are aching and intensify when dressing, raising your arms up, or moving behind your head. After suffering injuries, a crunching sensation occurs in the joint. The amplitude of hand movements decreases. The patient experiences severe pain when lifting minor weights, at rest;
- Stage III – formed osteophytes injure soft tissues. The affected joint hurts constantly and loses mobility. Painful sensations are difficult to relieve with medications. Patients report a feeling of frozenness in the joint. Spasms of surrounding muscles and contractures are detected;
- Stage IV – develops in the absence of adequate treatment. The pain becomes unbearable due to the destruction of the joint. Most often, patients require joint replacement.
Introduction
Infectious arthritis of the sternoclavicular joint (SJJ) is a rare surgical disease. Its frequency among arthritis of other localizations is less than 1% [1, 2, 10, 16]. Features of the anatomical structure of this area, polymorphism of clinical manifestations, due to the variety of options for the course of the pathological process, often become the cause of diagnostic errors [2, 5, 7, 16]. Another reason for frequent diagnostic difficulties is the lack of awareness of surgeons about this disease and the peculiarities of its course [23, 28]. When a patient first seeks medical help, especially in the subacute course of the process, the differential diagnostic list most often includes non-surgical diseases, such as Tietze syndrome (a disease from the group of chondropathy, accompanied by aseptic inflammation of the upper costal cartilages), rheumatoid arthritis, osteoarthritis, metastatic tumor lesion of the joint [1, 2, 7, 18]. Among the surgical diseases under the guise of which infectious arthritis of the GCS can occur, the most common are cervical or supraclavicular lymphadenitis, phlegmon or neck cyst [1, 2, 27]. Delayed diagnosis can lead to progression of the disease with involvement in the pathological process of the first costosternal joint, mediastinum, and cellular spaces of the neck [1, 17, 23].
Infection of GCS most often occurs hematogenously, and GCS arthritis is often observed in patients with transient or permanent immunodeficiency, for example due to cancer, diabetes mellitus, long-term use of corticosteroids, HIV infection [6, 11, 13, 15]. In some cases, the development of the inflammatory process is preceded by minor trauma, hypothermia, catheterization of the subclavian vein, and the injection of narcotic drugs into the veins of the upper limb by drug addicts [4, 12, 20, 21]. Quite rarely, the cause of the inflammatory process in the GCS is specific infections: syphilis, tuberculosis, salmonellosis, brucellosis [2, 6, 9, 19]. Purulent inflammation of the GCS can occur during sepsis [6, 23]. Isolated observations of the development of GCS arthritis are also described in chronic autoimmune diseases with skin lesions [4, 26]. Sometimes the disease develops spontaneously against the background of complete well-being [10, 11, 16, 22].
GCS is characterized by a number of anatomical features that largely determine the clinical course of the disease. The articular cavity of the GJ is quite small and surrounded by dense ligaments; the joint capsule has little ability to stretch [1, 14]. All this contributes to the relatively rapid spread of infection beyond the joint, leading to the formation of periarticular phlegmon and involvement in the pathological process of the sternum, the first sternocostal joint, and the mediastinum, located in close proximity to the primary focus of infection [1, 2, 14, 25].
As a rule, damage to the RGC is a unilateral process, but in 2-5% of cases bilateral damage occurs [8, 21, 24].
Both gram-positive and gram-negative flora can be involved in the development of infectious arthritis of the GCS; Staphylococcus aureus is the most common [3, 6, 20, 24].
Treatment
An arthrologist treats this pathology. Not every clinic has a specialist in this very narrow profile, so orthopedists, surgeons, and rheumatologists help solve this problem.
Treatment of arthrosis of the acromioclavicular joint can be either medicinal or surgical, which is directly dependent on the patient’s condition, the severity of the disease and the patient’s wishes. If a conservative path of therapy is chosen, then massage, gymnastics, physiotherapy, the use of medications and the prescription of exercise therapy are considered justified.
Drug treatment
For drug therapy, the following groups of drugs are most often prescribed:
- chondoprotectors that can partially or completely restore damaged cartilage (Glucosamine, Artra, Alflutop, Structum);
- anti-inflammatory drugs (non-steroidal), which relieve pain and eliminate inflammation (Diclofenac, Aceclofenac, Naklofen, Naproxen, Indomethacin);
- muscle relaxants (Mydocalm, Sirdalud);
- medications that improve blood circulation in damaged tissues (Tental, Nikoshpan, No-shpa).
Any conservative effect is usually supplemented with physiotherapeutic procedures: massage, cryotherapy, laser therapy.
Clavicle massage
The choice of treatment method is carried out, first of all, based on the stage of development of the disease. For grade 1 arthrosis, drug therapy is sufficient. In grade 2, medicinal treatment of the affected area is indicated, and only in some cases is surgical intervention justified. With grade 3, most often, medical treatment is ineffective, so the main route of treatment is surgery. During the manipulation, a replacement (both complete and partial) of the shoulder joint occurs.
Important! In the later stages of development of the described pathology, drug therapy is very rarely helpful. This means that a visit to a doctor should be made immediately as soon as the patient notices the first signs of illness and limited mobility in the chest.
The processes that occur in the body during the development of arthrosis cannot be reversed. The consequence of the disease is the development of pathological processes in other organs and systems of the body, disruption of the patient’s motor activity, and a decrease in the quality of his life.
- The main methods of treating arthrosis of the sternoclavicular joint, symptoms and prevention
ethnoscience
Traditional medicine is used as an auxiliary method of treating ACL of the shoulder joint. This is justified when prescribing conservative treatment to a patient, as well as as an aid in rehabilitation after surgery. The following substances and plants have proven themselves to be excellent:
- beeswax mixed with rendered lard and rubbed into the joint until completely absorbed;
- white cabbage leaves, which relieve pain and inflammation;
- lingonberries in the form of a decoction, taken two tablespoons per day;
- corn silk, prepared as a tincture and taken 4-5 times a day in the amount of one teaspoon;
- horseradish root, used as a compress, which is applied to the affected area;
- elecampane root infused with vodka and applied to the inflamed area until the pain disappears.
Arthritis of the clavicle is an unpleasant disease both from the point of view of sensations and from the point of view of the prognosis for restoration of the connection. All people at risk should take chondoprotectors that improve metabolic processes in cartilage tissue and the production of synovial fluid. The prescription of such drugs is the responsibility of the attending physician.
It is necessary to seek help not only when the pain becomes unbearable, but also at the moment of the first suspicion of problems with joint mobility. Patients who are overweight and have diabetes, as well as older citizens and professional athletes are especially susceptible to this type of inflammation.
2018.11.26223 Degenerative lesions - Arthrosis
Our quality of life also depends on the mobility of our joints. And it is worth taking care not only of the knee joints, which experience maximum stress. Other joints, such as the sternoclavicular joint, are also prone to wear. Diseases affecting the joint can lead to severe pain and make it difficult to use the hands with minimal daily activities. One of these ailments is arthrosis of the sternoclavicular joint (ICD-10 code - 19), which is faced not only by elderly patients, but also by young people.