Anatomy of the Human Knee Joint - information:
Knee joint, art. genus , is the largest and at the same time the most complex of all articulations. This is due to the fact that it is in this place that the longest levers of the lower limb (femur and shin bones), which make the greatest range of movements when walking, articulate. The following are involved in its formation: the distal end of the femur, the proximal end of the tibia and the patella. The articular surfaces of the femoral condyles, articulating with the tibia, are convex in the transverse and sagittal direction and represent segments of an ellipsoid.
Facies articularis superior of the tibia, articulating with the condyles of the femur, consists of two slightly concave articular platforms covered with hyaline cartilage; the latter are supplemented by two intra-articular cartilages, or menisci, meniscus lateralis et medialis, lying between the condyles of the femur and the articular surfaces of the tibia. Each meniscus is a triangular plate bent at the edge, the peripheral thickened edge of which is fused with the articular capsule, and the pointed edge facing the inside of the joint is free. The lateral meniscus is more flexed than the medial one; the latter in its shape rather resembles a crescent, while the lateral one approaches a circle. The ends of both menisci are attached anteriorly and posteriorly to the eminentia intercondylaris. In front, a fibrous bundle called lig stretches between both menisci. transversum genus.
The articular capsule is attached slightly away from the edges of the articular surfaces of the femur, tibia and patella. Therefore, on the thigh it rises upward in front, bypassing the facies patellaris, on the sides it goes between the condyles and epicondyles, leaving the latter outside the capsule for attachment of muscles and ligaments, and in the back it descends to the edges of the articular surfaces of the condyles. In addition, in front, the synovial membrane forms a large volvulus, bursa suprapatellaris, extending high between the femur and the quadriceps femoris muscle. Sometimes the bursa suprapatellaris can be closed and separate from the cavity of the knee joint.
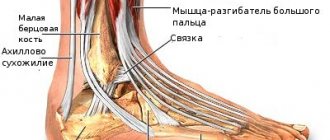
On the tibia, the capsule is attached along the edge of the articular surfaces of the condyles. On the patella, it grows to the edges of its cartilaginous surface, as a result of which it appears to be inserted into the anterior section of the capsule, as if in a frame. On the sides of the joint there are collateral ligaments running perpendicular to the frontal axis: on the medial side, lig. collaterale tibiale (from the epicondylus medialis of the thigh to the edge of the tibiae, fused with the capsule and medial meniscus), and on the lateral side, lig. collaterale fibulare (from epicondylus lateralis to the head of fibulae). On the back side of the capsule of the knee joint there are two ligaments that are woven into the back wall of the capsule - lig. popliteum arcuatum and lig. popliteum obliquum (one of the 3 terminal bundles of the tendon of the m. semimembranosi). On the anterior side of the knee joint is the tendon of the quadriceps femoris muscle, which covers the patella, like a sesamoid bone, and then continues into a thick and strong ligament, lig. patellae, which goes from the top of the patella down and attaches to the tuberositas tibiae. On the sides of the patella, the lateral extensions of the quadriceps tendon form the so-called retinacula patellae (laterale et mediate), consisting of vertical and horizontal bundles; vertical bundles are attached to the condyles of the tibiae, and horizontal bundles are attached to both epicodyli of the femur. These bundles hold the patella in its position during movement.
In addition to the extra-articular ligaments described, the knee joint has two intra-articular ligaments, called cruciate ligaments, ligg. crucidta genus. One of them is the front one, lig. cruciatum anterius, connects the inner surface of the lateral condyle of the femur with the area intercondylaris anterior tibiae. The other is the back, lig. cruciatum posterius, goes from the inner surface of the medial condyle of the femur to the area intercondylaris posterior of the tibia. The synovial membrane lining the inside of the capsule covers the cruciate ligaments protruding into the joint and forms two fat-containing folds, plicae alares, on the anterior wall of the joint below the patella, which adapt to the articular surfaces at each position of the knee, filling the gaps between them. The cruciate ligaments divide the joint cavity into anterior and posterior parts, preventing, in case of inflammation, the penetration of pus from one part to the other until a certain time.
A number of synovial bursae lie adjacent to the joint; some of them communicate with the joint. On the anterior surface of the patella there are bags, the number of which can reach up to three: under the skin - bursa prepatellaris subcutanea, deeper under the fascia - bursa subfascialis prepatellaris, and finally, under the aponeurotic stretch of m. quadricipitis - bursa subtendinea prepatellaris. At the place of lower attachment of lig. patellae, between this ligament and the tibia, there is a permanent synovial bursa, bursa infrapatellaris profunda, not communicating with the joint. In the posterior region of the joint, bursae are found under the attachment points of almost all muscles.
The following movements are possible in the knee joint: flexion, extension, rotation. By its nature it is a condylar joint. When extended, the menisci contract, ligg. collateralia et cruciata are strongly stretched, and the lower leg together with the thigh turns into one motionless whole. When flexed, the menisci straighten, a ligg. collateralia, due to the convergence of their attachment points, relax, as a result of which, when the knee is bent, it becomes possible to rotate around a vertical axis. When the lower leg rotates inward, the cruciate ligaments inhibit the movement. When rotating outward, the cruciate ligaments, on the contrary, relax. In this case, movement is limited by the lateral ligaments. The structure and location of the ligaments of the knee joint in a person contributes to his long stay in an upright position. (In monkeys, the ligaments of the knee joint, on the contrary, make it difficult to stand vertically and make squatting easier).
X-rays of the knee joint area simultaneously image the distal femur, proximal tibia, patella, and artculatio tibiofibularis. The “X-ray joint space” articulatio genus is the widest in the entire human osteoarticular apparatus, since it corresponds, in addition to the true anatomical joint space and articular cartilage, also to the cartilaginous menisci. On the x-ray, all the anatomical details of the distal femur and proximal tibia are visible. In lateral photographs, the picture of the knee joint is presented in profile; As a result, a projection layering of the epicondyles and condyles of the femur and tibia occurs on top of each other.
The knee joint receives nutrition from the rete articulare, which is formed by aa. genus superiores medialis et lateralis, aa. genus ihferiores medialis et lateralis, a. genus media (from a. poplitea), a. geniis descendens (from a. femoralis), aa. recurrentes tibiales anterior et posterior (from a. tibialis anterior). Venous outflow occurs through the veins of the same name into the deep veins of the lower limb - vv. Tibiales anteriores, v. poplitea, v. femoralis. The outflow of lymph occurs through deep lymphatic vessels in the nodi lymphatici poplitei. The joint capsule is innervated from the nn. tibialis et peroneus communis.
Types of cruciate ligament injuries.
There are three degrees of rupture of the joint:
- First. This stage is characterized by the appearance of micro-fractures. In this case, a diagnosis of “sprain” is made. Symptoms of injury are expressed by severe pain, swelling and impaired motor abilities. The joint part remains stable.
- Second. Partial rupture of the joint. The symptoms are practically no different from the symptoms of first-degree damage, but they are more pronounced and lasting. Any, even the smallest load in this case can lead to re-injury.
- Third. Complete rupture, accompanied by a specific crack. It is characterized by acute pain and lack of stability of the knee, severe swelling, and hemorrhage into the joint capsule. It is almost impossible to step on your foot.
Diagnostics
During a consultation with a surgeon or orthopedist, the doctor will ask the patient about the course of the pathology, conduct a visual examination and palpation. Additional laboratory and instrumental examinations provide assistance in making a diagnosis and selecting therapy:
Puncture sampling is an important study necessary to make a correct diagnosis.
- Puncture of intra-articular fluid allows you to assess its quantity, macro- and microscopic features, and the presence of specific markers of diseases.
- X-ray. Radiation diagnostics of joints in the anterior and lateral projection confirms fractures and destruction. X-rays examine the height of the patella to assess the condition of the ligaments.
- An ultrasound is performed to confirm fluid accumulation.
- Duplex scanning evaluates the circulatory network of the knee.
- A digital CT scan is performed if soft tissue damage is suspected.
- The structure of the bones is studied using MRI.
- To assess the nerve conduction of muscle function, electromyography is prescribed.
- In rare cases, the joint is examined during arthroscopy.
- If malignancy is suspected, tissue is taken for a biopsy.
Return to contents
Most common knee injuries
The structure of the human knee makes it a complex joint. Consequently, it can be susceptible to injury and various types of dysfunction. The most common injuries include:
- inflammation of the patellofemoral joint, also known as cinephile knee;
- rupture of the anterior cruciate ligament in the knee, for example, when skiing;
- knee sprain associated with placing the foot on an unstable surface;
- tendinitis associated with improper running technique;
- meniscus injury caused by knee extension in full flexion and rotation;
- luxation of the patella and fracture of the patella;
- rupture of the medial collateral ligament;
- inflammation of the goosefoot;
- Baker's cyst.
Anatomical defects in the structure of the knee joint also contribute to injuries. Excess weight and too much stress during activity are also factors that predispose to knee pain.
Causes of knee pain
Knee pain is a problem that can occur at any age. Some of the most common causes of knee discomfort include:
- rupture of the anterior cruciate ligament;
- fractures and sprains of the bones that make up the knee joint (including dislocation of the patella);
- meniscus tear;
- bursitis;
- inflammation of the knee joint;
- enthesopathy;
- jumper's knee, runner's knee;
- lateralization of the patella;
- chondromalacia patella;
- patellofemoral conflict;
- tendinopathy.
In addition, the cause of the ailments may be incorrect architecture of the lower limb, obesity or iliotibial band syndrome.
Synovial bursae
Synovial bursae (bursae) are small cavities located between bone and soft tissue. They are formed by connective tissue, lined inside with synovial membrane and filled with synovial fluid. Their main function is to reduce friction between bones and soft tissues. There are about 15 synovial bursae located in the area of the knee joint. The bursae help the muscles and tendons glide freely when moving the knee joint.
You can read more about the bursa of the knee joint here.
In addition to the synovial bursae, the soft tissue auxiliary apparatus of the joint also includes fatty bodies. By filling the free spaces, fat deposits play an important role and, together with other structures, ensure proper functioning of the joint. You can read more about fat bodies here.
Epiphyses and hyaline cartilage
If we look at the joint in more detail, its hardest part is the epiphyses. That is, the ends of articulated bones. They bear the heaviest load.
The epiphyses of bones, as a rule, have the following shape. One of them is convex and the other is concave.
The first is called the articular head, and the second is the glenoid cavity. They do not fit together perfectly, and the head, for example, may be more crooked than the cavity.
Each bone in the epiphysis zone is covered by hyaline cartilage, which is tightly adjacent to it, the thickness of which is from 0.5 mm to 2 mm.
Articular cartilage has two functions: it serves as a shock absorber in weight-bearing joints. In addition, it helps the ends of the bone fit tightly against each other during movement.
The destruction of articular cartilage triggers the process of deformation of the bones that form the joint and leads to the appearance of deforming osteoarthritis.
Technique
The operation is performed under anesthesia, which is selected taking into account the patient’s sensitivity to drugs, indications and time of operation. Epidural, local anesthesia and general anesthesia are used. Under normal conditions, the operation lasts about 1 hour.
- A tourniquet is placed on the patient's thigh to reduce blood flow to the joint.
- In the knee area, 3 incisions of 4-7 mm are made to insert instruments.
- Perform cleaning and rinsing.
- Remove the instruments and pump out the saline solution.
- If necessary, a solution of antibiotics and anti-inflammatory drugs is administered.
- Sterile dressings are applied to the incisions, which are removed after three days and covered with a plaster.
- A pressure bandage is applied to the knee and ice is applied.
The advantages of knee lavage and debridement include a short period of restoration of joint function, the absence of long-term immobilization with plaster, and a short duration of painkillers. The operation can be performed under local anesthesia. With high efficiency, the cost of surgical intervention is lower than open surgery.
Anatomical terms
First, it is necessary to clarify some anatomical terms.
Many body parts have duplicates. Often, to describe their position, an imaginary line drawn through the middle of the body is used. For example, “medial” means “located closer to the midline.” Or the medial side of the knee is the inner side that is closer to the other knee. The structures on the medial side also contain the word “medial” in their name. For example, the medial meniscus.
The opposite side to the medial side is lateral, that is, external.
Two other terms have the same meaning - proximal (indicating the location of an organ or part of it closer to the center of the body or to its median plane) and distal (a part of the body more distant from its center or median plane).
The term "anterior" refers to the front of the knee. The term "back" refers to the back.