Causes of deforming arthrosis of the knee Symptoms of deforming arthrosis of the knee Stages of osteoarthritis of the knee Treatment of deforming arthrosis of the knee Medicines for deforming arthrosis of the knee Nutrition for deforming arthrosis of the knee
Deforming arthrosis of the knee joint
(gonarthrosis, BAV) is a chronic progressive disease of articular cartilage. It is characterized by destruction of articular structures, which is accompanied by pain, inflammation and characteristic curvature of the limb (“wheel legs” or X-shaped deformity).
But deforming arthrosis of the knee, contrary to its name, destroys not only the knee joint. Due to the curvature of the limb and the deterioration of the shock-absorbing properties of the cartilage, the hip, ankle, and intervertebral joints begin to ache, hernias appear, and ligaments and menisci wear out.
Deforming arthrosis of the knee is a progressive disease of the articular cartilage.
This disease is no longer the province of isolated older people. The World Health Organization predicts an increase in the incidence of gonarthrosis in the next 2-3 decades. It can cause disability in every 4th woman and every 8th man. And at the moment, the incidence of BAV among adults already ranges from 13 to 29% in different regions. Among other arthrosis, in terms of frequency of development, it is second only to coxarthrosis (degenerative disease of the hip joint). But how to treat deforming arthrosis of the knee joint?
Causes of deforming arthrosis of the knee
Without normal lubrication, the joint “dries out,” cracks and loses height, exposing the heads of the bones. In this case, the end plate of the articular surface of the bone remains defenseless; overstimulation of the numerous nerve endings that are located in it causes pain and discomfort.
The following factors or a combination of them can cause deforming arthrosis of the knee:
- the presence of joint diseases (and knee diseases in particular) in relatives;
- genetic disorders associated with the formation of abnormal, unstable cartilage cells or their accelerated death;
- congenital and acquired malformations of the musculoskeletal system (flat feet, joint hypermobility, dysplasia, scoliosis, kyphosis and others);
- excessive professional, household or sports stress;
- microtraumas and injuries of the knee joint and meniscus, operations on it, leg fractures;
- blood supply disorders (varicose veins, atherosclerosis, thrombosis and other vascular diseases), their consequences (osteochondritis dissecans), as well as other causes of prolonged spasms in the legs;
- inflammatory diseases of joints and periarticular tissues (synovitis, bursitis, tendonitis, arthritis), incl. autoimmune nature (rheumatoid, psoriatic arthritis);
- metabolic disorders (gout, diabetes);
- age-related processes of aging of joints and leaching of calcium from bones;
- hormonal disruptions and changes in hormonal levels (for example, associated with a lack of estrogen in women);
- hypovitaminosis;
- excess weight (observed in ⅔ patients);
- physical inactivity.
But the main reason that deforming arthrosis of the knee is so common lies in its structure. The knee joint has only one axis (plane) of movement. Therefore, the volume of permissible movements is very limited. One awkward turn can injure the periarticular tissues and trigger arthrosis changes - after all, the sore knee will be subject to daily stress.
The reasons for the development of deforming arthrosis of the knee can be a large number of factors.
Personal manager
Patients of our Clinic can use the “Personal Manager” service free of charge.
A trained employee will be responsible for providing information support to the patient and resolving issues related to the preparatory and rehabilitation stages, consultations and explanations of the progress of the upcoming surgical intervention. Plot in the Good Morning program on Channel One about the treatment of clubfoot at the Constanta Clinic. Guest of the Health program with Elena Malysheva Vavilov Maxim Aleksandrovich Treatment O- and X-shaped legs. Hemiepiphysiodesis. CONSTANTA Clinic through the eyes of a child! Anesthesia for operations in children Treatment of children with the support of the Charitable Foundation
Symptoms of deforming arthrosis of the knee joint
Gradually increasing pain in the knee joint. At first, the pain is noticeable only when moving - for example, when sharply straightening or bending the leg, there is a feeling that “you stepped on your foot unsuccessfully.” In the early stages, pain may be episodic or so weak that it is perceived as discomfort. Then the pain intensifies after physical activity or prolonged stay in the same position. The skin also becomes painful - it reacts sensitively to any touch, incl. and clothes.
The pain is unstable - it can intensify due to microtraumas, inevitable with arthrosis, but invisible to the patient, and then subside again, sometimes for a long time. Until it becomes permanent in the final stages.
There are 3 types of specific pain in deforming arthrosis of the knee joint:
- starting (lasts 15-30 minutes after the joint leaves a prolonged state of rest);
- mechanical (noticeable during physical activity and goes away after rest);
- blockade (feeling of sharp pinching in the knee).
Rapid fatigue and deterioration of supporting function.
When walking and other everyday activities, the limb quickly gets tired, discomfort and a feeling of tension appear. It becomes difficult to stand for a long time, cramps and muscle spasms are possible. Morning stiffness is observed (up to 30 minutes).
Decreased knee functionality.
When flexing and extending, an unpleasant feeling of pulsation first occurs; at the next stage of the disease, a sensation of physical obstruction or “sand” appears in the joint. Gradually, the range of motion decreases due to the growth of osteophytes, and a dull crunching sound is heard more and more often.
Neurological and metabolic disorders.
They manifest themselves in a feeling of numbness and stiffness, which manifests itself especially quickly and strongly if the patient takes an uncomfortable position (for example, tucks his legs under him), sits or stands for a long time. After this, the patient is forced to “disperse.” Often, patients with arthrosis suffer from seizures. Due to poor nutrition of the limb, fatigue increases and muscle mass decreases.
Limb deformity.
At first, the shape and size of the joint itself changes - it swells and stands out sharply against the background of arthrofing muscles and ligaments. Depending on which part of the bone has undergone greater abrasion, in the later stages of the disease the leg bends outward or inward (valgus or varus deformity), lameness appears, and the patient falls on the affected limb. Even before the deformation becomes noticeable to the naked eye, a change in gait occurs.
Symptoms of deforming arthrosis of the knee, as a rule, increase slowly due to the fact that the disease does not progress quickly. This is the insidiousness of arthrosis - gradually getting used to the discomfort of the disease, the patient “gets used” to the pain, does not notice the worsening and postpones a visit to the doctor.
Knowledge of the main symptoms of deforming arthrosis of the knee will help to recognize the disease in time
2.4. Quality of life assessment
A decrease in the quality of life during the formation of long-term pathological conditions consists of many factors. At the same time, physical suffering is not always the leading one, but persistent psychological disorders come to the fore. Therefore, to assess the quality of life, the SF-36 questionnaire (scale) was used in accordance with the “Instructions for processing data obtained using the SF-36 questionnaire” [1].
“The SF-36 questionnaire (scale) is formed based on the analysis of answers to 36 questions, divided into two large groups - the physical component and the mental component” [2] (see Table 6).
“The 36 questionnaire items are grouped into eight scales: physical functioning, role functioning, bodily pain, general health, vitality, social functioning, emotional state and mental health (see Tables 8 and 9). The scores on each scale range between 0 and 100, with 100 representing full health. The results are presented in the form of scores on 8 scales, compiled in such a way that a higher score indicates a higher level of quality of life.”
The data that was obtained using questionnaires was then grouped into tables to compare the main indicators of treatment effectiveness before and after adjustment.
Stages of knee osteoarthritis
The progression of gonarthrosis is most easily noted after familiarization with the stages of the disease. Timely treatment of deforming arthrosis of the knee and counteracting degenerative processes are extremely important. After all, gonarthrosis can not only make a person disabled, but also reduces immunity, provokes irritability and depression, and leads to general exhaustion.
Deforming arthrosis of the knee joint 1st degree
Pain in grade 1 deforming arthrosis of the knee joint occurs as a result of serious physical exertion and goes away on its own after rest. In the mornings and after a long period of immobility, stiffness and stiffness are observed in the knee, and it is difficult for the joint to return to full movement.
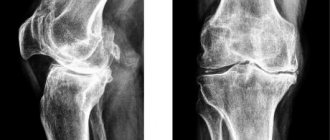
At this stage, treatment of deforming arthrosis of the knee is especially effective, but patients rarely notice changes in their condition. Damage to the joint is also hardly noticeable on x-rays and other diagnostic examinations.
Deforming arthrosis of the knee joint, grade 2
Pain occurs during the patient’s daily activity, but begins to annoy him even at rest. The pain syndrome intensifies with changes in weather and hypothermia. Movements in the joint are accompanied by a rough crunching sound, which is repeated over and over again. Contractures begin to appear - persistent restrictions on mobility in the joint, which are still reversible, but already interfere with the performance of certain types of work. The gait also changes. With grade 2 deforming arthrosis of the knee joint, the knee is almost always edematous, swollen, and often hot. Patients complain of chronic fatigue in their legs. Gradual deformation of the affected limb begins. If the knee joint is affected only on one side, the second also begins to wear out rapidly due to decompensated load. Therefore, the lack of treatment for deforming arthrosis of the knee at this stage can lead to disability.
At stage 2 of the disease, the x-ray shows obvious signs of arthrosis: narrowing of the joint space, osteophytes, focal erosions and cystic cavities.
Deforming arthrosis of the knee joint, grade 3
At this stage, gonarthrosis turns the patient into a disabled person who cannot do without outside help, constant therapy or surgery. The patient is incapacitated. The pain syndrome is continuous and interferes with sleep. The patient suffers from severe pain day and night, regardless of the load on the joint. The joints crunch loudly with every movement and show signs of chronic inflammation. Walking is difficult and is only possible with aids (crutches, walking sticks). The shape of the joints is changed, as is the shape of the limbs (in the shape of the letter O or X), and one of the legs may become shorter than the other. The muscles around the knee are atrophied and are in chronic spasm. Movements in the joint are severely limited or impossible at all due to the blockade of the knee. Treatment of deforming arthrosis of the knee is now purely surgical.
On an x-ray, the joint space has practically no clearance, massive growths are visible on the edges of the bone, the heads of the bones are erased. Destruction of synovial cartilage, ligaments, and meniscus is also diagnosed.
Diagnostics
A preliminary diagnosis is made after an examination, during which the doctor assesses the degree of curvature of the limbs.
X-rays are taken to confirm the diagnosis. They make it possible to identify insufficient ossification, underdevelopment or deformation of the child’s bones, and signs of joint destruction in adults.
Preoperative X-ray, patient with third degree hallux valgus deformity
Treatment of deforming arthrosis of the knee joint
Treatment of deforming arthrosis of the knee joint consists of the complex use of medications, dosed loads on the joint, physiotherapeutic procedures and the use of orthopedic devices.
During the treatment process, it is extremely important to alternate loading and unloading, and to avoid static loading of the knee. Orthopedic insoles, specialized shoes, canes, crutches, walkers, and ergonomic chairs for work and rest also help slow down the disease. Particularly effective are orthoses with variable stiffeners, which allow one to simulate the physiological axis of the leg and compensate for deformation.
In the early stages of deforming arthrosis of the knee, the goal of treatment is to restore the damaged joint and ligamentous apparatus, relieve pain and increase the range of voluntary movements. In the later stages, it helps to alleviate the patient’s condition. For this purpose, sanitation arthroscopy (washing with antiseptics) when a piece of osteophyte is broken off, corrective osteotomy (correction of a curved bone), and endoprosthetics (replacement) of the joint.
In addition to the orthopedist, physiotherapists and chiropractors, specialists in exercise therapy and therapeutic massage, and surgeons will tell you how to treat deforming arthrosis of the knee joint.
Treatment of deforming arthrosis of the joints is a complex and long process that requires an integrated approach.
Physiotherapy
Among other physiotherapeutic techniques for the treatment of deforming arthrosis of the knee joint, the following are used:
- laser and magnetic therapy;
- microwave therapy;
- shock wave therapy;
- amplipulse;
- ultrasound therapy;
- electrophoresis with analgin, novocaine, chymotrypsin, etc.;
- phonophoresis with glucocorticoids;
- paraffin and ozokerite applications;
- cryotherapy;
- acupuncture;
- joint traction and kinesitherapy;
- balneotherapy.
Massage for deforming arthrosis of the knee joint
Therapeutic and lymphatic drainage massage for deforming arthrosis of the knee joint, as well as manual therapy, are carried out by a specialist after the inflammation in the joint has been relieved. For self-massage at home, stroking and rubbing are recommended, as well as movements aimed at stretching muscles and ligaments, and a deep warm-up (carried out last, after the warming effect). Self-massage goes well with local irritants and essential oils. Remember that with deforming arthrosis of the knee joint, massage is performed on both joints, even if only one of them is affected.
Exercises for deforming arthrosis of the knee joints
Therapeutic gymnastics (physical therapy) for deforming osteoarthritis of the knee joint is carried out in a sitting or lying position; water aerobics is also effective. An individual set of exercises for deforming osteoarthritis of the knee joint is prepared by an instructor. Below we offer a short warm-up aimed at strengthening the leg muscles.
- Sit on the floor, legs straight, resting on your hands behind your back. Bend and straighten your toes.
- The starting position is the same, slowly bend your leg, resting your toe on the floor at the end of the movement. Repeat, placing your foot behind the other leg.
- Continue in the same starting position, raising your outstretched leg in front of you, toes towards you.
- Without changing the starting position, we stretch our hands to the toes of our straight legs.
- While sitting on the floor, hug your bent knee and try to lift your other leg off the floor.
- Sitting on the floor, spread your legs shoulder-width apart. Rotate your legs one at a time so that your toes move 180 degrees.
- Sitting on the floor, legs bent. Roll your foot from heel to toe, feeling the work in the back of your thighs.
Great! Perform exercises for deforming osteoarthritis of the knee joint at least 3-6 times a day.
2.3. Assessment of the position of reference lines and the angles they form
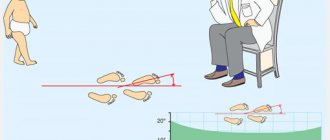
Valgus deformity of the lower extremities is caused by deviation of certain axes of the segments from the normal (or average) position. Therefore, to assess the magnitude of deformation and control recovery, it is necessary to know the normal boundaries of the location of the axes of the entire lower limb, individual segments, as well as the normal values of the angles formed by them. L.N. Solomin calls them reference lines and angles (RLU). They are assessed in both frontal and lateral projections.
Figures 6 and 7 show the mechanical axes of the femur and tibia, the orientation lines of the joints and the angles they form in frontal and lateral projections. Only some of them are used in practical work (they are highlighted in white in the figure). Those lines and angles, the position and magnitude of which were assessed in this study, are presented in Table 7.
Figure 6 - Mechanical axes of the femur and tibia, joint orientation lines and the angles they form in the frontal projection (left) and lateral projection (right). The most commonly used angles are highlighted in white.
Figure 7 – Scheme of the location of the mechanical axis of the lower limb (left) and the formation of the anatomic tibiofemoral angle [102]
Table 7 - Main reference lines and angles determined from radiographs
| English abbreviation | English name | Russian name | Average value is normal |
| MAD | Mechanical axis deviation | Mechanical axis deviation | 9.7±6.8 mm |
| ATFA | Anatomic tibiofemoral angle | Angle of intersection of the mechanical axes of the femur and tibia | 6,85+1,4° |
| aLDFA | Anatomic lateral distal femoral angle | Lateral distal angle of orientation of the articular surface of the femur to the mechanical axis | 79–83° |
| MPTA | Medial proximal tibial angle | Medial proximal angle of orientation of the articular surface of the tibia to the mechanical axis | 85–90° |
| aPPTA | Anatomic posterior proximal tibial angle | Tibial plateau angle | 77–84° |
RLU was assessed either manually or automatically using the PacsViewer program ( Figure 8 ).
Rotational deformity, when localized to the lower leg in thin patients, was determined clinically, as shown in Figure 9 .
Figure 8 – Radiographs of a 47-year-old patient with the main lymph nodes identified in the PacsViewer program
Figure 9 – Scheme for determining the tibia torsion angle based on a clinical examination
If rotational deformity was detected (or if it was suspected), CT was performed. Based on the obtained images, rotational deformation was determined according to the scheme presented in Figure 10 .
Figure 10 – Scheme for determining the torsion of the thigh (left) and tibia (right) based on CT examination
This chapter presents the general principles of x-ray examination of such patients. Due to the introduction of new types of X-ray equipment and the expansion of their diagnostic capabilities, some elements and features of X-ray diagnostics are new and are described in more detail in the next chapter.
Medicines for deforming arthrosis of the knee
Drug treatment of deforming arthrosis of the knee joint allows you to quickly relieve acute pain, reduce inflammation and swelling, and improve nutrition of the joint. Therefore, medications are used at all stages of the disease and help restore mobility to the knee.
Chondroprotectors
Chondroprotectors in the form of tablets, capsules, sachets and injections are used for the regeneration and maintenance of synovial cartilage.
The most effective chondroprotectors include artracam, dona, teraflex, structum, movex, artron, alflutop.
Anti-inflammatory
Steroid and non-steroidal anti-inflammatory drugs are used to treat deforming arthrosis of the knee joint. They are prescribed in the form of tablets, injections, sachets, creams, ointments and other products for external and internal use.
Nonsteroidal drugs (NSAIDs) include: artradoldiclofenac, nimesulide, paracetamol, meloxicam, indomethacin, ketorolac, ibuprofen, piroxicam and others.
Steroids: hydrocortisone, prednisolone, dexamethasone, kenalog, flosterone, methylprednisolone.
Anti-inflammatory drugs can be used in conjunction with anesthetics (novocaine, lidocaine, trimecaine), which are injected into the joint cavity as a blockade.
Antispasmodics
Relieving spasm is necessary for the patient to return to normal activity and the normal flow of nutrients into the tissues. For this purpose, buscopan, pentalgin, papaverine, drotaverine (no-shpa), spasmalgon, halidor, novigan and others are used.
Angioprotectors
For deforming arthrosis of the knee joint, troxevasin and troxerutin, pentoxifylline, drugs based on horse chestnut, detralex, trental, cinnarizine and others are used.
Warming agents
Among the warming agents, it is worth highlighting preparations based on natural ingredients: snake and bee venom, hot pepper, mustard. For example, capsicam, viprosal, apizartron.
Voltaren, Dolobene, Fastum, Finalgon and Nicoflex are also used. All these drugs improve blood supply to tissues and distract from pain.
Nutrition for deforming arthrosis of the knee
A healthy diet for deforming arthrosis of the knee joint includes dishes with a reduced content of trans fats and “fast” carbohydrates. Preference should be given to lean meat and fish, seafood and vegetables, steamed, wrapped in foil or stewed under a lid. Also useful are fruits, berries and drinks rich in antioxidants - wild plants, blueberries, lingonberries, cranberries, high-quality green tea and coffee. You can also eat whole grain porridge and legumes. But potatoes, white bread, sweets, processed foods, fast food and alcohol should be excluded.
If you are overweight with deforming arthrosis of the knee joint, consider low-carbohydrate diet options.
Three degrees of illness
Hallux valgus deformity has several stages:
| Degree | Signs |
| Lightweight | The knee joint is at the top of an angle that opens outward (it is formed by the femur of the leg and the bones of the lower leg, called the external angle of deviation) Normally, the angle between the bones of the leg and the thigh is no more than 5–7 degrees; with mild disease, it increases to 10–15 degrees. |
| Average | The deflection angle is 15–20 degrees |
| Heavy | The angle of deviation of the shin outward is more than 20 degrees |
Three stages of hallux valgus. Click on photo to enlarge