On X-rays, the anatomy of the hip joint looks simple and understandable even to people far from medicine, however, everything is not as banal as it seems at first glance. Although the joint consists of only two bones and visually resembles a regular hinge, its full operation includes much more than simple rotation within a strictly limited radius. The joint provides full walking, supports the body in an upright position and helps the lower limbs cope with high loads. What are the anatomical features of the hip joint, what does the normal physiology of the joint depend on and how does it change with age? Let's look at the complex issues of orthopedic anatomy more clearly and consistently.
Basic anatomy of the hip joint: bones that form the joint
The human hip joint is formed by two bones, the surfaces of which ideally coincide, like pieces of a puzzle. The acetabulum on the surface of the ilium plays the role of a kind of pocket into which the spherical process of the femur is immersed - the head, completely covered with durable and elastic cartilage. Such a complex resembles a hinge, the rotation of which is achieved due to the harmonious coincidence of the sizes and shapes of the adjacent osteochondral structures.
Soft and painless sliding between two fairly tightly adjacent bones is achieved due to the special structure of cartilaginous tissue. The combination of collagen and elastin fibers allows you to maintain a rigid and at the same time elastic structure of cartilage, and proteoglycan molecules and the water included in the composition guarantee the necessary pliability and elasticity. In addition, it is these substances that are responsible for the timely release of the optimal amount of joint fluid, which serves as a shock absorber during movement, protecting sensitive cartilage from abrasion.
The joint cavity is limited by a special capsule, the basis of which is fibrous fibers. These molecules are characterized by increased strength, so that even under great pressure the joint retains its integrity and original shape. However, this reserve is not unlimited, and, unfortunately, it is impossible to guarantee 100% the impossibility of dislocation: with inadequate loads, strong external pressure or a sharp displacement in space, such an atypical injury is quite real.
Large and small pelvis
There are large and small pelvises. The boundary line separating them runs along the inner surface of the pelvic bones from the protrusion on the spine - the promontory (the junction of the last lumbar vertebra with the sacrum) to the upper edge of the pubic symphysis.
Large pelvis The large pelvis is the upper section of the pelvis, formed by the unfolded wings of the ilium. It is the lower wall of the abdominal cavity and serves as a support for the internal organs.
Small pelvis The small pelvis is located below the large pelvis and is limited from behind by the sacrum and coccyx, in front and from the sides by the ischial and pubic bones. It distinguishes between entrance, exit and cavity. The pelvic cavity contains the bladder, rectum and internal genital organs (ovaries, fallopian tubes, uterus and vagina, prostate, seminal vesicles and vas deferens). The entrance to the small pelvis is open to the abdominal cavity and corresponds to the border line with the large pelvis. The exit from the pelvic cavity is closed by the muscles that form the pelvic diaphragm, through which the urethra and rectum pass in men, and the urethra, rectum and vagina in women. From the outside, this area of the body stands out as the perineum.
The pelvic organs differ from the abdominal organs in that they can significantly change their volume: the bladder and rectum periodically fill and empty, the uterus enlarges and moves during pregnancy. This affects the functioning of other organs and blood supply.
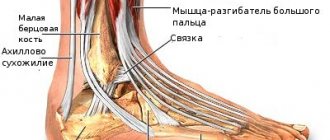
Hip joint: anatomy of the ligamentous apparatus
Ligaments play a very important role in the functionality of the hip joint. It is these super-strong fibers that maintain the optimal shape of the joint, ensure adequate mobility and activity of the joint, and protect against injury and deformation. The ligamentous apparatus of the hip joint is represented by the most powerful fibers:
- The iliofemoral ligament is the most powerful and durable ligament in the human body, capable of withstanding incredible loads without tears or sprains. Experimental experiments have shown that its fibers are capable of withstanding a load comparable to the weight of 3 centners. It is thanks to this that the joint remains protected during intense training, unsuccessful movements and other unpleasant surprises that affect the mobility of the femoral joint.
- The ischiofemoral ligament is a much thinner and softer ligament that controls the degree of pronation of the femur. It is, as it were, woven into the articular capsule, located from the ischium all the way to the trochanteric fossa.
- The pubofemoral ligament is responsible for the abduction angle of the free femur of the lower limb. Its fibers, like the ischiofemoral ligament, penetrate into the articular capsule, however, they originate not at the ischium, but at the pubic joint.
- The circular ligament does not leave the joint capsule. As the name suggests, it is located in a circle, encircling the head and neck of the femur in a tight loop and secured to the anterior surface of the lower bone.
- The ligament of the femoral head is the most original in the anatomy of the hip joint. Unlike its “colleagues”, it does not directly protect the joint and does not control its mobility; the functions of this ligament are to preserve the blood vessels with which it is penetrated. This feature is explained by its location, which coincides with the trajectory of the vessels: the ligament begins at the acetabulum and ends at the head of the femur.
Causes of weakened pelvic floor muscles
Obvious factors that lead to weakened muscles and sprains include pregnancy and being overweight. This is basic physics: growing weight during pregnancy, as well as fat mass, increases pressure on muscles and ligaments.
Professional sports and fitness are not obvious risk factors. People started talking about this problem relatively recently: in January 2021, an article was published in which experts called the problem of the pelvic floor a real epidemic, especially among female runners.
Power training
When it comes to strength training, it doesn't matter at all whether you're doing barbell deadlifts, doing heavy abs, or unloading wagons. All these actions lead to a sharp increase in intra-abdominal pressure. If you perform exercises without engaging the deep muscles, the increasing pressure will gradually push through the pelvic floor muscles and stretch the ligaments.
Cardio loads
In the 2021 article mentioned above, experts say that pelvic floor dysfunction affects more than 30% of women. Among female athletes, this percentage is even higher.
At risk are runners, cyclists, gymnasts, track and field athletes, those who exercise on trampolines and participate in ball sports. This is due to the so-called “high-return effect.”
The higher the impact of the load in sports, the stronger the impact will be on the muscles and ligaments of the pelvic floor. To reduce the risk of such problems, you need to carefully consider your training system.
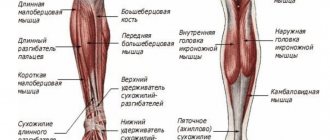
Anatomical features and functions of the muscular frame
The musculature of the hip joint is represented by fibers of various types and functionality. This is primarily due to the varied trajectory of movement that the hip can perform. So, if we classify muscle fibers into groups according to function, in the anatomy of the hip joint we should highlight:
- The transverse, or frontal, muscle group, which is responsible for flexion and extension of the lower limb in the pelvic area. Among them are the flexor muscles (sartorius, iliopsoas, pectineus, rectus, tensor fascia lata) and hip extensor muscles (gluteus maximus, adductor magnus, semitendinosus, semimembranosus and biceps). Thanks to their coordinated work, a person can sit down and stand up, squat down and take a vertical position, pull his legs to his chest and straighten up.
- The anteroposterior, or sagittal, muscles regulate the adduction and abduction of the leg. This group includes adductors (major, short and long adductors, gracilis and pectineus) and abductors (obturator internus, tensor fascia lata, twin, piriformis, gluteus medius and minimus) muscle fibers.
- The longitudinal muscle group coordinates the rotation of the hip. Here the supinator muscles are distinguished (gemini, piriformis, iliopsoas, quadratus, sartorius, obturator, gluteus maximus and posterior groups of the middle and small gluteal fibers) and pronators (tensor fascia lata, semitendinosus, semimembranosus, anterior group of the middle and small gluteal fibers) .
Each of the muscles represented in the anatomy of the hip joint performs not only a motor function: powerful fibers take on part of the load during movements. And the more trained they are, the better they cope with pressure, thereby unloading the joint and performing a shock-absorbing function. Thanks to this, the likelihood of injury due to unsuccessful movements is also reduced, since the muscles are more mobile and extensible than the tissues of the joint.
Nerve fibers adjacent to the hip joint
Like any joint of the human body, the hip joint is not distinguished by a high organization of the nervous system: the endings localized in this area mainly innervate the muscle fibers, regulating the degree of sensitivity and coordinated work of each muscle group in response to external influences. Conventionally, all nerve fibers of the hip region can be divided into 3 groups:
- anterior external, which includes branches of the femoral nerve;
- anterior internal - branches of the obturator nerve;
- posterior - branches of the sciatic nerve.
Each group is localized in a specific area of the thigh, for which it is responsible in the complex structure of the nervous system of the body in general and the lower extremities in particular.
Blood circulation of the tissues of the hip joint: anatomy of the arteriovenous bed
The round ligament artery, the ascending branch of the lateral and deep branch of the medial circumflex femoral arteries, as well as certain branches of the external iliac, inferior hypogastric, superior and inferior gluteal arteries take part in the nutrition and supply of oxygen to the tissues of the hip joint. Moreover, the importance of each of these vessels is not the same and can change with age: if in youth the vessels of the round ligament carry a noticeable amount of blood to the femoral head, then over the years this volume decreases to approximately 20-30%, giving way to the medial circumflex artery.
Physiological capabilities of the hip joint
The hip joint can perform movements in three planes at once - frontal, sagittal and vertical. Thanks to the structure of the joint, thought out by nature, a person can easily bend and straighten the hip, move it to the side and bring it to its original position, rotate it in all directions, and at a fairly noticeable angle, the magnitude of which can vary depending on the anatomical features and training of the ligamentous apparatus. But that’s not all: the hip joint is one of the few joints that can move from the frontal to the sagittal axis, providing the free limb with full circular motion. It is on this ability that a person’s mobility, his physical characteristics and abilities for certain sports (for example, gymnastics, athletics, aerobics, etc.) primarily depend.
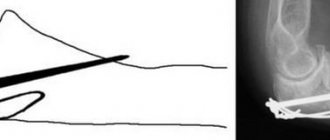
The other side of the coin is the rapid wear and tear of the cartilaginous surfaces of the hip joint. The pelvic and femur bones bear the maximum load during walking, running and other types of physical activity, respectively, this pressure is transferred to the joints. The situation can be aggravated by excessively high weight, too intense physical activity, or, conversely, a passive lifestyle in which the muscular system practically does not protect the joint from deformation. As a result, the cartilage surfaces begin to wear out, become inflamed and become thinner, pain appears, and the trajectory of movement is significantly limited. Even the slightest deviation in the condition of the muscles, ligaments or bones of the hip joint can lead to serious pathology, which subsequently requires long-term and intensive treatment.
However, restoration of the full function of the joint is not always possible: in some cases, surgical intervention is required, in which the affected tissue is replaced with a prosthesis. To prevent this from happening, it is worth monitoring the condition of the musculoskeletal system from a young age, strengthening joints, training the muscle frame wisely and moderately, and taking care of proper and nutritious nutrition of the body. Only in this way can you protect your joints from destruction, and yourself from pain, stiffness of movement and tedious treatment!
conclusions
Even if you have been involved in sports for a long time and are sure that everything is in order, you should make sure that there really are no problems. This can be done by contacting specialists:
- urogynecologist;
- gynecologist/obstetrician-gynecologist;
- Women's Physiotherapist/Physiotherapist;
- Applied Functional Science Specialist (a physician, physical therapist, or personal fitness trainer who has specialized, certified training and knowledge of the functional and muscular relationships in the body).
Prolapse of internal organs and other problems with the pelvic floor do not occur instantly; the likelihood and speed of their manifestations depends on a combination of many factors: the genetic strength of the connective tissue, the number of pregnancies, births and injuries in them, the load that falls on the body, etc.
Unfortunately, few people know about this, think about it or are involved in prevention. We really want you to take care of your health and always adequately assess the risks associated with this or that type of physical activity. It is important that you know what to do, and then problems will not affect you.
Training the pelvic floor muscles is a proven effective method of preventing its incompetence and its consequences: urinary incontinence and organ prolapse. Arnold Kegel exercises, like other similar techniques, can and should be performed before, during and after pregnancy, as well as as a preventive measure when playing sports or fitness.
Authors: Olga Rebrova, certified Pilates trainer, senior specialist in the #Sekta training department; Daria Knyazeva, group program instructor, head of the training department #Sekta
Literature
1. REVIEW: “Functional anatomy of the pelvic floor”, Salvatore Rocca Rossetti, Professor of Urology, University of Torino, Torino, Italy 2. Principles of core stability in the training and in the rehabilitation: review of literature Larissa Neves Pavin1, Claus Gonçalves2 1 Physiotherapist, São José do Rio Preto-SP, Brazil; 2 Physiotherapy School, University Paulista, São José do Rio Preto-SP, Brazil. Received October 14, 2009 Accepted December 7, 2009 3. Johnson, Joshua, “Functional Rehabilitation of Low Back Pain With Core Stabilization Exercises: Suggestions for Exercises and Progressions in Athletes" (2012). All Graduate Plan B and other Reports. Paper 170. 4. Pool-Goudzwaard A, Slieker ten Hove M, Stoeckart R, et al. Relations between pregnancy-related low back pain, pelvic floor activity and pelvic floor dysfunction. International Urogynecology Journal And Pelvic Floor Dysfunction. November 2005;16(6):468-474 5. Arab A, Behbahani R, Lorestani L, Azari A. Assessment of pelvic floor muscle function in women with and without low back pain using transabdominal ultrasound. Manual Therapy. June 2010;15(3):235-239 6. Christie C, Colosi R. Paving the way for a healthy pelvic floor. IDEA Fitness Journal. May 2009;6(5):42-49 7. Thomas W. Myers. Anatomical trains. Myofascial meridians for manual and sports medicine, Publishing house: Meridian-S, 2010 8. Nicole Radziszewski, “Help for Pelvic-Floor Dysfunction” 9. Running, Sue Croft, Physiotherapist with a special interest in pelvic floor dysfunction including urinary incontinence, prolapse conditions, bowel management and pelvic pain for women, men and children 10. Pelvic floor muscle function in women with pelvic floor dysfunction: a retrospective chart review, 1992-2008. Department of Physiotherapy and Occupational Therapy, Copenhagen University Hospital Glostrup, Glostrup, Denmark 11. Bø K. Urinary incontinence, pelvic floor dysfunction, exercise and sport. The Norwegian University of Sport and Physical Education, Oslo 12. DeLancey JO, “What's new in the functional anatomy of pelvic organ prolapse?” Norman F. Miller Professor of Gynecology, Professor of Urology, Director Pelvic Floor Research Group, Director Female Pelvic Medicine/Reconstructive Surgery, Ann Arbor, Michigan, USA 13. Pomian A1, Lisik W2, Kosieradzki M3, Barcz E1. "Obesity and Pelvic Floor Disorders: A Review of the Literature." 1st Department of Obstetrics and Gynecology, Medical University of Warsaw, Warsaw, Poland. Department of General Surgery and Transplantology, Medical University of Warsaw, Warsaw, Poland. Department of General Surgery and Transplantology, Medical University of Warsaw, Warsaw, China (mainland) 14. Rocca Rossetti S. “Functional anatomy of the pelvic floor.” Professor of Urology, University of Torino, Torino 15. Bø K “Urinary Incontinence, Pelvic Floor Dysfunction, Exercise and Sport” 16. Christina Christie, PT. "The Inner Pelvic Core" 17. Christina Christie, PT. “Moves to Strengthen the Pelvic Floor” 18. Christina Christie, PT and Rich Colosi, DPT. "Paving the Way for a Healthy Pelvic Floor"