Common factors that provoke the development of this pathology also include:
- High body weight. It leads to an increase in mechanical and shock-absorbing loads on the joints of the bones.
- Pregnancy. In the later stages, if you do not follow the recommendations of your doctor, divergence of the pelvic bones may appear.
- Pathologies of cartilage and bone tissue. This may be the occurrence of bone growths, stretching of the joint capsule and a number of similar problems.
- Bad habits. Inflammation often manifests itself against the background of heavy smoking, drinking alcohol, or ingesting heavy metal salts.
- Problems with blood supply. They can arise due to varicose veins, atherosclerosis and a number of other factors.
- Traumatic impact. In addition to the injuries listed above, the pathology can be caused by bruises with the formation of internal hematomas, microscopic ruptures of tendons and fascia, and other injuries that may be invisible to the naked eye.
Therapeutic procedures will be aimed at achieving the following goals:
- preventing the inflammatory process;
- eliminating pain syndrome;
- normalization of blood circulation in the joint;
- preventing further destruction of cartilage tissue.
Treatment of the hip joint in the “Health Workshop” relieves muscle spasm, pain and inflammation in the joints, normalizes the nutrition of the cartilage and accelerates its recovery. Therapeutic procedures activate blood circulation and improve overall well-being.
After completing the course, our doctor will give the patient a manual with joint gymnastics exercises to perform independently at home. The doctor will advise what else to do to prevent the disease.
Drug treatment
Drug therapy for this pathology varies greatly depending on what was the root cause of the disease. to treat hip joint pain :
- Glucocorticoids. Prescribed for severe intoxication.
- Antibacterial agents. They are used if it has been established that the cause of the disease is an infectious effect. Fluoroquinolones, macrolides or tetracyclines are commonly used.
- Muscle relaxants. Used if you need to reduce muscle spasm.
- Immunosuppressants. They are used if the cause is reactive arthritis or psoriasis. Often, the doctor prescribes their use in conjunction with folic acid.
- Non-steroidal anti-inflammatory drugs. Help reduce the inflammatory response.
- Chondroprotectors. They stimulate the restoration of cartilage tissue and stop the development of degenerative processes.
- Vitamins and immunostimulants. Used as maintenance treatment.
All of these medications (and a number of others) can be used exclusively as prescribed by the attending physician. Independent choice of drugs can lead to aggravation of the situation and the emergence of health problems.
Anatomy of the pelvic bone
Each pelvic bone is divided into the following three:
- The ilium is an opening bone that forms the upper pelvic lobe of the bone. You can feel (touch) it by simply placing your hands on your hips.
- The ischium is the part of the hip bone that is located at the back below, resembling an arch in appearance.
- Pubic - the anterior lobe of the base of the pelvic bones.
When connected, these bones create the acetabulum, the main socket that houses the head of the femur.
In childhood (up to 16–18 years), these bones are united with each other by cartilage; at an older age (after 18 years), this tissue hardens and gradually turns into a solid bone, which is called the pelvic bone. The photo shows the body of the ischium.
Interesting! At the base of the ischium there are tubercles - rough, thickened bones. They are popularly called sitting bones because in a sitting position, the human weight is distributed on the pelvic bones.
Normal pelvic anatomy
The pubic joint in front and the sacroiliac joints, which are formed from the ear-shaped plane of the back of the bone and the base of the sacrum, are the normal anatomy of the pelvic bone. In the video you can see in detail the structure of the human pelvis.
Anatomically, the pelvis is divided into two sections:
- Large - an extremely large part of the bone (located at the top of the pelvis).
- The small pelvis is its narrow part (located at the bottom of the pelvis).
Both pelvises are conventionally separated by the so-called boundary line, running along the top of the sacrum, then to the arcuate contour of the ilium, which also covers the outer part of the pubic bone and the symphysis of the same name.
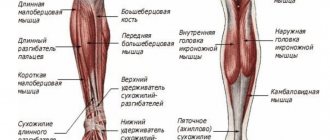
Numerous muscles of the abdominal cavity, back and spine are attached to these bones on both sides. Some leg muscles originate from them. Thus, a muscular frame is obtained.
The structure of the small and large pelvis
The pelvis is a constituent part of the lower region of the human skeleton. In addition to the coccyx and sacrum, it is formed by two pelvic bones. In addition to the bones, the pelvic joints and ligaments act as support for the entire body.
The large pelvis is open in the front, with the planes of the ilium on both sides, and the lumbar vertebrae and the place where the sacrum forms at the back.
The small pelvis is a cylindrical space, on the sides of which are the lower parts of the ilium and ischium. The pubic bones form the anterior walls of the pelvis, while the posterior ones are made up of the bones of the sacrum and coccyx.
Converting large to small creates an overhead passage. And the lower passage is made of the pubic bones, coccyx and ischial tuberosities.
Pelvic joints and ligaments
The hip joint has a complex structure and performs an extremely important function in human life. Thanks to this connection, a person can perform the following actions:
- walk;
- stand;
- sit;
- run;
- jump;
- tilt.
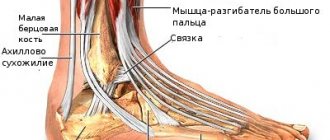
The joint consists of the head of the femur and the acetabulum. Those parts of the recess that are in close contact with the femoral head are densely covered with cartilage tissue. In the middle part of the acetabulum there is a fossa, which at the bottom is filled with connective tissue and surrounded by a synovial membrane. It is in this fossa that the ligament of the femoral head is attached.
Rehabilitation after surgery
Most often, non-surgical methods help cure inflammation of the hip joint. However, if there is severe pain or stiffness in the joint, surgery is necessary. We do not perform hip surgery.
If you have had surgery on a joint, you need to begin a rehabilitation course within a few days. This course can be taken at the Health Workshop network of clinics in St. Petersburg. Our doctors will create a set of procedures for the patient that will strengthen the body, restore mobility to the operated joint and consolidate the positive effect of the operation.
Stage of resection of part of the femur with a tumor
Surgical electric drill saw for bone processing:
The process takes less than a minute.
At the cutting site, the surgeon takes bone marrow samples and sends them to the laboratory to ensure that the remaining portion of the femur is free of tumor cells.
The resected ligaments and a fragment of the femur are removed along with the tumor without opening the bone shell. The photograph shows the articular surfaces of the hip joint:
The surgeon explains that removing a large amount of soft tissue around the tumor reduces the risk of recurrence of the malignant disease.
Results of histological examination of the removed bone fragment: “Microscopically: metastases of clear cell renal cell carcinoma. Macroscopically: in the soft tissues a tumor measuring 5.4 / 3.4 / 4 cm of a whitish color is determined with ingrowth into the bone by 1.5 cm. The distance to the edge of bone resection is 3.5 cm.” That is, it is confirmed that the source of the metastasis is the previously removed kidney, and the cutting site was chosen correctly. The surgeon sent an image of tumor cells:
Prevention
Doctors at the Health Workshop give the following recommendations for preventing joint inflammation:
- swim, walk more, get stronger;
- do not overload or overcool the joints;
- treat infections in a timely manner, do not endure them “on your feet”;
- drink at least 1.5 liters of water per day;
- watch your weight and posture, don’t slouch;
- do not drink alcoholic beverages or smoke;
- limit the consumption of sugar and salt, carbonated drinks;
- monitor the level of uric acid in the body;
- eat more dairy products, fruits, vegetables;
- include fatty fish, jellied meat, jelly and other products with gelatin in your diet.
Pathological anatomy
There are quite a lot of bone anomalies and they depend on a variety of factors, ranging from intrauterine bone underdevelopment (most often found in premature babies) and ending with injuries (dislocations, fractures), which subsequently led to pathology of the pelvic bones.
The most common anomalies are a wide, narrow or deformed pelvis.
- Wide. Today, a clinically and anatomically wide pelvis is distinguished. This pathology is most likely in tall, overweight people.
- Narrow. Just like wide, they are divided into clinically and anatomically narrow. The causes of a narrow pelvis may be impaired development inside the womb, insufficient nutrition, or some serious diseases, for example, rickets.
- Deformation (displacement of bones). In 99% of cases, displacement occurs in the baby’s body at birth (if the child’s mother has deformed pelvic bones, then the child’s bones, as they pass through the birth canal, become bent and displaced, not only in the pelvis, but also in the entire skeleton). This pathology is transmitted from mother to child. And in only 1% of patients, pelvic deformation occurred as a result of injury.
- Aplasia or hypoplasia - this disease, transmitted by inheritance, is quite rare, characterized by the absence or underdevelopment of one of the pelvic bones.
- Deep acetabulum - the head of the femur is located more deeply. The pathology can be either unilateral or bilateral (most common).
- Divergence of the pubic symphysis is most often observed in patients with disorders of the central nervous system, bladder or spinal exstrophy.
A clearer idea of the extent of the anomaly is provided by X-ray data.
Kinds
There are two types of lesions in this area:
- Osteosarcoma of the hip joint is a cancerous tumor growing from bone tissue;
- Chondrosarcoma of the hip joint is a cancerous tumor growing from cartilage tissue.
Osteosarcoma of the hip joint
This type of cancer is a common disease in the human body. Most often it affects men, adolescents and children, and women very rarely.
This pathology is characterized by rapid growth and easy metastasis to neighboring organs.
Causes of osteosarcoma of the hip joint
The main causes of this disease are the following:
- Rapid bone growth;
- Consequences of injuries;
- External ionizing radiation;
- The presence of benign tumors in the body or their detection before illness.
Symptoms of osteosarcoma of the hip joint
It is very difficult to diagnose pathology in the early stages without special equipment. The appearance of the pain syndrome is quite similar to pain in other pelvic diseases. Also, in the first stages, the pain may not be severe, and an increase in body temperature may be observed.
In subsequent stages, the pain intensifies, which can often be observed when moving. Ridges and spots may appear on the skin. Malignant cells grow, which leads to pressure on nerves, blood vessels, and nearby organs. Then the pain spreads to the thigh area and genitals. The hip joint becomes less mobile.
Over time, osteosarcoma develops and the pain becomes very difficult to relieve. With blood and lymph, metastases quickly spread to other organs.
Diagnosis of osteosarcoma of the hip joint
First you need to visit an oncologist. He will order an x-ray to determine the location of the tumor.
Afterwards, cancer cells are taken for examination using a biopsy, a CT scan is done to determine the size of the formation, and the vessels are checked using angiography.
Treatment of osteosarcoma of the hip joint
Treatment methods for this type of osteosarcoma are the same as for other cancers: chemotherapy and surgery. You just need to remember that for osteosarcoma of the hip joint, radiation therapy is not used, since it has no effect on this pathology.
Chondrosarcoma of the hip joint
This pathology is a tumor that grows from cartilage tissue.
Symptoms of chondrosarcoma of the hip joint
Symptoms for this type of cancer will be as follows:
- The appearance of swelling in the thigh area;
- Some swelling of the skin;
- Displacement, compression and organ dysfunction due to chondrosarcoma;
- Severe pain when moving.
Diagnosis of chondrosarcoma of the hip joint
Foot cancer
First you need to visit an oncologist.
Further, radiography can be used. Thanks to this research method, it is possible to determine the location of the suspected cancer.
The next diagnostic method is biopsy. In order to determine the nature of the cancer and its stage, cancer cells are taken for analysis.
A CT scan is also done to determine how the cancer has spread and the size of the tumor.
Angiography is also performed, which shows the condition of the blood vessels near the tumor.
PET CT evaluates the overall condition of oncology.
Treatment of chondrosarcoma of the hip bone
Treatment for chondrosarcoma will also be surgery or chemotherapy.
Cement fixation of the endoprosthesis
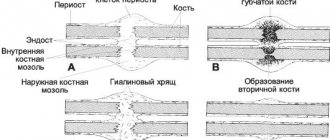
Bone cement is made by mixing liquid and powder during surgery to create a quickly hardening plastic that bonds the surface of the bone to the prosthetic components. This cementing method has improved significantly in recent decades. Until now, bone cement has been the weakest link in the prosthesis-cement-bone energy transfer chain. Today we use all technical capabilities to optimize the process and use the “Vacuum Cementing Method”.
Cement fixation of the hip joint endoprosthesis© Implantcast
Mixing of cement is carried out in a special vessel in a vacuum, for which a special pump is used. This reduces the number of air pockets in the cement during the curing process and therefore increases the strength of the cured bone cement.
Before applying the bone cement, the bone is cleaned using pulsed lavage. It is an irrigation pump that constantly injects water into a cap with a lid under low pressure. Water is simultaneously pumped out of this cap using suction. Contaminants such as blood residues, bone fragments and fat fractions are removed. This improves the contact between the bone surface and the surface of the endoprosthesis.
In addition, when cementing the stem, the medullary cavity of the femur is closed from below, so cement can be introduced under pressure without additional air entering the prepared cavity. This is achieved by using a special suction device to remove blood components and air from the surgical field.
How does chondrosarcoma manifest?
The severity of clinical manifestations of chondrosarcoma depends on its morphological structure. Well-differentiated tumors are characterized by long-term slow growth (over 4-5 years) with low severity of symptoms. Such formations can reach significant sizes. With anaplastic chondrosarcomas, which often affect young people, symptoms develop faster, on average within 3 months.
The main symptoms of the disease are pain in the area of tumor growth. The pain is constant, characterized by a progressive increase in intensity. Other local manifestations (increased venous pattern, local increase in temperature, dysfunction of a nearby joint) are less common than with osteosarcoma and are less pronounced.
Book a consultation 24 hours a day
+7+7+78
Causes and risk factors for developing pelvic bone cancer
Factors that predispose to the development of the disease are some disembryonic disorders, as well as radiation and chemical effects on the body. As a result of an experiment on animals, the occurrence of bone cancer was revealed after the effect of radioactive strontium on the body. Precancerous conditions are considered to be osteochondral exostoses and deforming ostosis (Paget's disease).
Osteosarcoma most often develops during periods of increased bone growth. Therefore, adolescents, especially young men, are more at risk of developing this tumor.
Cementless fixation of the endoprosthesis
With cementless fixation, all parts of the endoprosthesis are in direct contact with the bone. Therefore, the surfaces of the prosthesis are specially coated and processed in such a way that the endoprosthesis grows into the bone. This process is called "Osseointegration". Special bone substitutes, such as hydroxyapatite and various titanium alloys, are used to cover the endoprosthesis. All components of the endoprosthesis are pressed into the bone using the so-called 'Press-fit-Technik' technique.
This process requires a certain preparation of the bone surfaces in contact with the endoprosthesis.
- To install the endoprosthesis stem, the medullary cavity of the femur is cut out with special cutters in the shape of the endoprosthesis. After this, the leg of the prosthesis is pressed into a previously prepared cavity, which makes it possible to quickly load the leg after surgery.
- When installing a cup, a so-called 'Press-fit' cup is often used. It is driven in and seems to get stuck in the bone, because... by its design, it is larger in size than the corresponding depression. Screw cups with self-tapping external threads that are screwed into the bone are not used at Gelenk-Klinik.
Diagnosis of the disease
Based on complaints and examination of the patient, a specialist may suspect pelvic bone cancer, but an accurate diagnosis can be made using the following instrumental research methods:
- X-ray diagnostics. Taking an image in two projections is mandatory if bone cancer is suspected. The main radiological symptoms of malignant bone tumors are foci of destruction of a plastic, lytic or mixed nature. The lesions do not have clear boundaries. A common symptom is periostitis with a needle or bulbous pattern.
- Osteoscintigraphy. The severity of the malignant process in the bone is characterized by the intensity of accumulation of the radiopharmaceutical. This study is used both to identify hidden lesions inside and outside the bone, and for the purpose of differential diagnosis with bone metastases.
- Computed tomography allows you to clarify the boundaries of tumor formation. Using CT, you can also determine the nature of the location of the primary lesion in relation to the surrounding soft tissues.
- A histological examination is mandatory to establish a diagnosis of bone cancer.
Sometimes it becomes necessary to perform phlebography or angiography. These studies help to clarify the location of the vessels near the tumor before performing surgery.