The pelvis is one of the most important, although sometimes ignored, parts of the skeleton. The pelvis is shaped like a basket with a tip and its cavity contains many vital organs, including the intestines and bladder. In addition, the pelvis is at the center of gravity of the skeleton. If the body is compared to a pencil balanced horizontally on a finger, its point of balance (center of gravity) will be the pelvis.
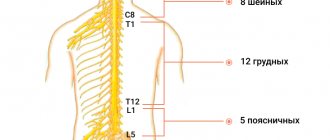
Therefore, it is obvious that the location of the pelvis greatly affects posture. It's the same as if the central block in the tower is offset, and in this case all the blocks above the offset risk falling. And if you compare the central block with a box, then tilting can lead to the box falling out. Similar mechanisms occur when the pelvis is tilted, and the contents of the pelvis shift forward. The result is a protruding belly and protruding buttocks. Since the pelvis is the junction of the upper and lower torso, it plays a key role in body movement and balance. The pelvic bones provide support to the most important supporting part of the body – the spine. In addition, the pelvis allows the lower limbs and torso to move in a coordinated manner (in tandem). When the pelvis is positioned normally, various movements are possible, twisting and bending and the biomechanics of movements are balanced and the distribution of load vectors is even. Displacement (distortion) of the pelvis from normal positions causes dysfunctional disorders of the spine, as there is a change in the axis of load distribution during movement. For example, if there is a misalignment of the axle in a car, then rapid wear of the wheels occurs. Something similar happens in the spine, lever effects and excess load on certain points occur, which lead to rapid wear and tear of the spinal structures. Therefore, often the main cause of back and neck pain is a change in the position of the pelvis (displacement, distortion). Changing the position changes the biomechanics, which can lead to degenerative changes in the spine, disc herniation, scoliosis, osteoarthritis, spinal canal stenosis, sciatica, etc. Pelvic misalignment also leads to pain and dysfunction in the neck, neck pain radiating to the shoulders and arms, and contributes to the development of carpal tunnel syndrome and other problems in the extremities.
1.What is chronic pelvic pain in women and its causes?
Chronic pelvic pain in women is diagnosed when pain in the pelvis and abdominal pain lasts more than 6 months.
The area where such pain is located is below the navel. Persistent abdominal pain in the pelvic area can manifest itself differently in different women. For some, it is a mild pain in the abdomen that appears and then disappears. For others, it is severe and constant pain in the pelvic area, which interferes with work, sleep and just living normally.
If the cause of pain in the pelvic area is found, its treatment will get rid of the problem. But if the exact cause of pelvic pain is not clear, the situation is not hopeless. There are ways to relieve pain and return to a full life.
Causes of pelvic pain
There are several groups of common causes of pelvic pain:
- Problems with the reproductive system
such as endometriosis, adenomyosis, uterine fibroids; - Scar tissue
(adhesions) in the pelvic area after an infection or surgery; - Diseases of the kidneys, urinary tract or intestines
- irritable bowel syndrome, chronic irritation of the bladder; - Physical or sexual abuse.
The exact reasons for this phenomenon are not known, but approximately half of women with chronic pelvic pain have been subjected to such violence.
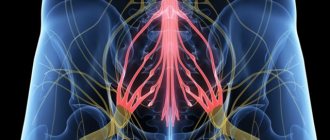
Doctors are not always able to identify the causes of chronic pelvic pain. Sometimes even a large number of different tests and examinations do not give results. It also happens that the cause of pelvic pain is discovered and even eliminated, but the affected nerves continue to send pain signals. This is called neuropathic or neuropathic pain
. In this case, diagnosis is even more difficult.
A must read! Help with treatment and hospitalization!
Symptoms
Symptoms of displacement (distortion) of the pelvis can be either moderate or severe and significantly impair the functionality of the body. With moderate misalignment, a person may feel unsteady when walking or may experience frequent falls.
The most common symptoms such as pain are:
- In the lower back (with irradiation to the leg)
- Pain in the hip, sacroiliac joints, or groin
- Pain in the knee, ankle or foot Achilles tendon
- Pain in shoulders, neck
If the pelvis is misaligned for a long time, the body will correct and compensate for biomechanical imbalances and asymmetries and corresponding adaptations of muscles, tendons and ligaments will occur. Therefore, treatment may require some time. In addition, pelvic distortion can be difficult to correct, since over time a pathological pattern of movements is formed. The longer the period of pelvic distortion, the longer it takes to restore normal muscle balance.
2.Types of pelvic pain
The type of pain can vary greatly. Sometimes abdominal pain and pelvic pain are associated with menstruation, and sometimes they are not. Main types of pelvic pain
problems that women may experience are:
- Mild to severe pain in the pelvic area;
- The pain ranges from constant but mild to sharp and sudden;
- Severe pain with cramps during menstruation;
- Pain during sex;
- Pain when urinating or defecating.
Often, chronic pelvic pain, like other types of constant pain, leads to depression and poor sleep.
Visit our Gynecology page
Treatment
Pre-hospital assistance
Patients with pelvic fractures are placed on a backboard and given an anesthetic. In other cases, rest is recommended, sometimes taking analgesics, using local warming and anti-inflammatory drugs is acceptable. Pain in the pelvic bones often indicates the presence of serious pathologies that require prompt diagnosis and early treatment, so if this symptom is present, you should immediately seek professional help.
Conservative therapy
Patients with fractures undergo an intrapelvic block, apply skeletal traction, or are prescribed bed rest using a special position. Therapeutic tactics for other lesions depend on the characteristics of the disease. The following methods are used:
- Protective mode
. Patients are advised to limit physical activity. Sometimes it is necessary to use crutches or a cane. - Drug therapy
. Taking into account the characteristics of the pathology, antibiotics, NSAIDs, analgesics, chondroprotectors and other drugs can be prescribed. - Physiotherapy
. UHF, drug electrophoresis, magnetic therapy and other techniques are indicated. Exercise therapy, massage, and manual therapy are prescribed.
For malignant neoplasia, radiation therapy or chemotherapy may be used.
3.Diagnosis of the disease
Most likely, the first time you see a doctor for chronic pelvic pain, your doctor will perform a full gynecological examination.
to detect possible problems with the reproductive system.
In addition to general questions about symptoms, health, past illnesses, and health and mental health problems, your doctor may order specific tests and tests:
- Blood tests and urine tests to look for signs of infection;
- Pregnancy test;
- Tests for sexually transmitted infections.
If initial studies are inconclusive and do not help find the cause of chronic pelvic pain, visual examination of the abdominal organs may be performed, including:
- Transvaginal ultrasound;
- MRI;
- Computed tomography of the pelvis.
Another possible test is laparoscopy
. During laparoscopy, the doctor inserts a thin tube with a miniature camera on the end through a small incision in the abdomen. This allows you to detect any growths or scar tissue that may be causing your pelvic pain.
In fact, diagnosing and identifying the causes of pelvic pain can be a very lengthy process. To help your doctor, write down when the pain occurs, the type of pain, and possible causes that may be causing the pain. All of these are clues about why pelvic pain occurs and how to cope with it.
About our clinic Chistye Prudy metro station Medintercom page!
4. Treatment of pelvic pain
If the doctor was able to determine the cause of pain in the pelvic area, an individual treatment regimen is selected. Here are some common treatments for abdominal and pelvic pain in women:
- Birth control pills or hormone therapy to treat menstrual problems;
- Surgeries to remove a cyst or tumor;
- Medicines. For example, antibiotics to treat an infection or special medications to treat irritable bowel syndrome.
If the causes of chronic pain in the abdomen and pelvic area have not been identified, the doctor may suggest treatment methods that will help cope with the pain.
. For example:
- Painkillers – ibuprofen, naproxen. Some of them are sold without a prescription at the pharmacy. Other, stronger ones will be prescribed by the doctor. These medications work best when taken on an ongoing basis, rather than just when pain occurs. In any case, the dosage regimen should be determined by the doctor.
- Tricyclic antidepressants can help cope with both pain and depression;
- Consulting a specialist about pain response techniques and non-drug ways to cope with pain and stress may also be helpful.
You may have to try several different treatments for chronic pelvic pain before finding the one that works best.
Why do the pelvic bones hurt?
Traumatic injuries
Intense pain is observed with pelvic fractures that occur against the background of high-energy trauma. Sharp pain at the fracture site appears at the time of injury, subsequently decreases slightly at rest, intensifies with any movement, and often forces the patient to take a forced position. Possible shortening of the limb. The location of pain is determined by the type of fracture:
- fracture of the ilium - in the area of the wing of the bone;
- fracture of the ischium - in the perineum;
- fracture of the pubic bone - in the pubic area;
- fracture of the acetabulum - in the lower outer parts of the pelvis, hip joint, groin area.
Pelvic fractures in children correspond to injuries in adults. In adolescence, the edges of the bone may be torn off during intense physical activity, which is due to the relative weakness of the bones compared to rapidly growing muscles. Symptoms in such cases are mild, the pain is local, reminiscent of a bruise. A hematoma forms in the fracture zone.
Pregnancy period
Minor aching and pressing pain in the pelvic bones in the II-III trimesters of pregnancy may be associated with the physiological adaptation of the body to bearing a child. Superficial pain in the projection of the womb, intensifying during sexual intercourse, at night, when pressing on the pubis, spreading the legs to the sides, walking up the steps, is noted with symphysitis. In severe cases, lameness develops, symphiolysis is possible, manifested by intense pain, inability to stand and walk.
Pelvic fractures in pregnant women are detected against the background of hypocalcemia. They are formed not only as a result of injuries, but also as a result of pathological childbirth or diseases of the pelvic bones (osteomyelitis, tuberculosis, osteodystrophy). Characterized by severe pain in the pubis, perineum or other pelvic area, impaired movement, forced body position.
Inflammatory and infectious diseases
When the pelvic bones are affected, pain of the corresponding localization occurs in patients with osteitis deformans. The painful sensations are dull, aching, continuous, intensified at rest, after rest. The affected bone thickens. Pathological fractures are possible. When the process is located in the acetabulum and adjacent areas, osteoarthritis is formed.
Pain in the sacrum and ilium is noted with sacroiliitis. The purulent form of the pathology is manifested by sharp tugging, tearing pain, deterioration of the general condition, intoxication, and hyperthermia. Other forms of sacroiliitis are accompanied by fleeting pain along the posterior surface of the pelvis; less commonly, persistent pain syndrome is observed.
Osteomyelitis of the pelvic bones is rarely detected; in adults it develops against the background of trauma and surgery; in children it can be a consequence of hematogenous spread of infection. It is characterized by extremely sharp pains that intensify with the slightest movements. The condition quickly worsens, hyperthermia and intoxication syndrome are detected. After the formation of the fistula, the intensity of pain decreases.
Pelvic tuberculosis is a rare form of osteoarticular tuberculosis that affects the sacroiliac joint and the articular surface of the ilium. It manifests itself as pain of unclear localization, stiffness of movement, and moderate pain in the affected area. Subsequently, local infiltration and the formation of leaky abscesses on the thigh are observed.
Pain in the pelvic bones
Tumors
The pelvic bones are quite often affected by tumor processes. The nature of the pain syndrome depends on the type of neoplasia. With benign neoplasms, the pain is insignificant, local, of uncertain localization, transient, and remains at the same level for many months or years. Malignant tumors manifest themselves with pain that increases over several months. At first the pain is weak, aching or nagging, later it becomes sharp, strong, constant, and can be eliminated only with narcotic analgesics. The symptom is observed with the following tumors and tumor-like formations:
- bone cyst;
- osteochondroma;
- osteoma;
- chondrosarcoma;
- chondroblastoma;
- Ewing's sarcoma;
- metastases to the pelvic bones.
Osteodystrophy
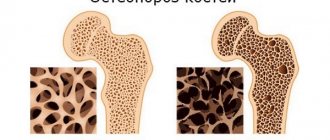
Pain in the pelvic bones is observed in various forms of osteodystrophy, including those caused by somatic diseases. Osteomalacia is characterized by vague pain in the bones of the pelvis and limbs. Pain is disturbing both during movement and at rest, intensifying with pressure and cessation of pressure on the iliac bones. Over time, the intensity of pain increases, pathological fractures, deformities, and restrictions of movement occur.
Pain in the pelvic bones with osteoporosis is minor, but can be combined with painful sensations in the spine, ribs, hip, and ankle joints. They are detected in postmenopausal, juvenile, and other types of osteoporosis. Pathological conditions that provoke secondary osteoporosis, osteomalacia or osteosclerosis include:
- Endocrine pathologies
: hyperthyroidism, diabetes mellitus, Itsenko-Cushing's disease, hyperparathyroidism, hypopituitarism. - Gastrointestinal diseases
: malabsorption syndrome, liver disease, condition after gastrectomy. - Kidney damage
: chronic renal failure, renal tubular acidosis, Fanconi disease. - Genetic diseases
: osteogenesis imperfecta, Ehlers-Danlos syndrome, Marfan syndrome. - Blood diseases
: leukemia, lymphomas, myeloma, thalassemia. - Other conditions
: COPD, condition after organ transplant, fasting, anorexia nervosa, prolonged immobilization, alcoholism. - Taking medications
: glucocorticoids, thyroid hormones, immunosuppressants.
Other diseases
Pain in the pelvic projection can be detected in the following diseases:
- Forestier's disease.
Minor periodic pain in the pelvis, combined with pain and stiffness of the spine. - Fibrous dysplasia.
Periodic mild pain, increasing deformations of the pelvic ring, causing the development of kyphosis or scoliosis. - ARS syndrome.
Pain in the projection of the symphysis after physical activity, increasing with hip abduction. - Mental disorders
. Unusual, rapidly changing or fanciful nature of pain that does not fit into the picture of a certain somatic pathology.