A disease such as arthrosis of the facet joints of the spine can rarely be found in a patient’s outpatient chart. It is quite difficult in differential diagnosis. Therefore, in case of characteristic jadoba, the doctor prefers to diagnose the familiar osteochondrosis. In fact, arthrosis of the facet joints is a pathology that, with proper examination, can be detected in 70% of modern urban residents who have crossed the age line of 45 years. And after reaching the age of 60 years, arthrosis of the facet joints occurs in 95% of the examined patients.
The development of the disease is due to a number of reasons. Among the most common negative influence factors, doctors cite excess weight, a sedentary lifestyle and lack of regular physical activity on the muscular frame of the back.
Regular attendance at manual therapy sessions allows not only to avoid the development of arthrosis of the facet joints of the spine, but also to restore the natural mobility of the spinal column to a physiological extent at any age. If you have back pain with limited range of motion, a feeling of stiffness in the morning and rapid fatigue of the muscular frame of the spine, then we invite you to a free initial consultation at our manual therapy clinic. We see experienced vertebrologists, neurologists, osteopaths and chiropractors. The initial appointment for each patient is provided completely free of charge.
During the initial free consultation, the doctor examines the patient, establishes a preliminary diagnosis, and gives individual recommendations for further diagnosis and treatment.
Facet joints of the spine and their facets
To understand the essence of this pathology and the factors of its development, it is necessary to familiarize yourself with the basics of anatomy. The spinal column is a flexible structure that provides not only support for the entire body, but also flexibility and mobility of the torso. Due to the special structure of the spine, a person can make body turns, bends in different directions, twisting and a number of other active movements.
The spinal column consists of:
- vertebral bodies with spinous processes;
- intervertebral discs, consisting of cartilage tissue and ensuring uniform distribution of shock-absorbing load;
- uncovertebral joints;
- facet joints with pronounced process facets.
It is the facet joints that provide attachment of the spinous processes to each other. And due to this, it becomes possible to make various movements with the body and head.
Normally, the facet joints of the spine are covered inside with a cartilaginous synovial layer. A dense joint capsule ensures stability of the facets. And synovial fluid creates ideal conditions for the heads of bones to glide easily during various movements.
The facets of the facet joints have a certain structure that prevents their rapid destruction during injury. But with prolonged exposure to excess body weight or curvature of the spinal column, these bones quickly collapse and become deformed. It is for this reason that people who are used to slouching and holding their back unevenly suffer from crunching and pain with any movement. This indicates that the facets of the facet joints of the spine are destroyed. If complex treatment is not started in a timely manner, the disease quickly progresses and leads to impaired mobility.
The blood supply to the facet joints and their structural parts (cartilaginous, synovial, connective, bone tissue) is carried out through diffuse exchange with the surrounding muscles. To do this, the muscular frame of the back must be subjected to constant physical activity. During muscle fiber contraction, fluid is released, which is absorbed by the cartilaginous structures of the joints and intervertebral discs. If the muscles do not work, then diffuse metabolism is disrupted.
The process of dehydration of cartilage and synovial tissue begins. This becomes the beginning of a destructive process. At first, tight mobility is observed, then, as the cartilaginous layer thins and the bone tissue is exposed, it begins to crack and fill with deposits of calcium salts.
Degenerative changes of the facet joints
Chronic degenerative changes of the facet joints begin at a young age. During puberty (12–16 years), hormonal changes in the human body begin. If during this period a teenager leads a sedentary lifestyle and does not force his back muscles to constantly “work,” then the excess amount of hormones starts the process of destruction of cartilage tissue. This can only be avoided with regular physical activity in accordance with the age-related recommendations of physiologists.
At an older age (approximately 25–27 years), an age-related restructuring of the configuration of the spinal column occurs. the process of fusion of the sacral vertebrae begins. This reduces the shock-absorbing capacity of the spinal column, which gradually provokes the destruction of its facet, uncovertebral and facet joints.
Degenerative changes lead to the development of arthrosis, osteoarthrosis or spondyloarthrosis. X-rays, CT or MRI will help establish an accurate diagnosis.
Diagnostics
In cases where painful episodes recur monthly or more often, it is first necessary to conduct x-rays in several projections. As a rule, radiography allows us to determine pathological changes in the facet joints. However, CT allows better visualization of not only the joints, but also other structures of the spine.
MRI is not as effective for diagnosing this spinal pathology, but is very useful when it is necessary to diagnose a herniated disc or problems in the abdominal cavity.
But the most informative in this regard is the injection of a small amount of contrast agent into the facet joints, followed by radiography.
Hypertrophy and deformation of facet joints
Based on the results of an MRI examination, hypertrophy of the facet joints is often detected, which is a direct clinical sign of the development of the initial stage of arthrosis or spondyloarthrosis.
Spondyloarthrosis of the facet joints begins with primary dehydration of cartilage tissue. Then the thinning of the synovial layer begins. As a compensatory reaction, hypertrophy of the facet joints begins, which means a total uniform growth of bone tissue in the form of deposition of calcium salts.
Such deformation of the facets of the facet joints is considered an irreversible process, since there are no pharmacological drugs that would be able to return the physiological shape of the facets after their hypertrophy. In fact, at the initial stage it is possible to reverse this pathological process. For this purpose, manual therapy techniques are used:
- massage and osteopathy restore microcirculation of blood and lymphatic fluid in the area of tissue damage;
- reflexology starts the process of tissue regeneration by using the body’s hidden reserves;
- Therapeutic gymnastics and kinesiotherapy ensure uniform development of the muscular frame of the back, due to which the diffuse nutrition of all cartilaginous tissues of the spinal column is completely restored.
If you require treatment for arthrosis of the facet joints, then you should not resort to the use of non-steroidal anti-inflammatory drugs. They effectively relieve pain and stiffness of movement only in the early stages of the disease. Then their effect is completely neutralized and the patient requires injections of corticosteroids. These drugs also have anti-inflammatory and analgesic effects. However, they have an unpleasant side effect - they wash away calcium from bone tissue and provoke the development of osteoporosis. With arthrosis of the arcuate joints, this is fraught with acceleration of the process of destruction of bone tissue and loss of performance.
Introduction
Low back pain remains a common musculoskeletal disorder, with a lifetime incidence of 60–90%. Various structures are involved in the formation of chronic pain - the posterior longitudinal ligament, dura mater, annulus fibrosus, large muscles of the lumbar spine and facet joints [1].
Osteoarthritis of the facet joints is the most common pathology of the facet joints and develops in people over 20 years of age. The most common predisposing factors are mechanical stress, microtrauma and/or genetic predisposition. Most often, adults over 60 years of age are affected - almost every second person. Presumably, facet joint arthrosis is the most common cause of low back pain in older adults over 50 years of age [2, 3].
At risk are people whose lifestyle is associated with heavy lifting, loads that are inadequate for the spine (twisting movements) - athletes, loaders, mechanics, etc., as well as people forced to be in static tension and a sitting position for a long time - drivers, office workers, etc. [4].
Anatomy and innervation
Facet joints are a flat type of synovial joint between the articular processes of two adjacent vertebrae and are surrounded by articular capsules [5]. The cartilaginous surfaces of the facet joints provide a low-friction surface to facilitate movement under normal conditions in a healthy spine [6]. The facet joint capsule, subchondral bone and synovium are richly innervated by nociceptive nerve fibers [7]. Each facet joint is innervated by two medial branches arising from the spinal nerves [8, 9].
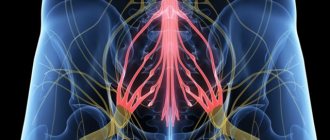
The dorsal branch is divided into medial and lateral (dorsal) branches at the level of the upper border of the transverse process [10]. The medial branches from the L1-L4 dorsal rami pass between the superior articular process and the vertebral pedicle, then along the upper edge of the corresponding transverse processes, pass under the mammillary (mamillo-accessory) ligament and divide into several branches innervating mm. multifidus, interosseous muscles, ligaments and two facet joints. Each medial branch innervates the overlying and underlying joint. The ascending branch starts from the mamillary ligament, the descending branch passes distally and goes to the underlying joint [11]. L1-L3 medial branches descend to 1-2 vertebrae, and L4-L5 medial branches descend to 2-3 vertebrae, L4-L5 medial branches reach the dorsal part of the sacrum and supply the lumbosacral joint [10] (Fig. 1) . Thus, pain sensations are transmitted along the medial branches of the spinal nerves from the capsule and synovium of the facet joint, mm. multifidus, ligaments, periosteum of the vertebral arches and vertebrae [12].
Rice. 1. DR - dorsal branch; ib—intermediate branch; lb - lateral branch; mb - medial branch; TP—transverse process; a - articular branch; ZJ - facet joint; VR—ventral branch [11].
For the first time, pain syndrome with damage to the facet joints was described as lumbosacral pain in 1911 by J. Goldthwait [13]. Later Badgley et al. suggested that the cause of back pain in 80% of cases is degenerative changes in the facet joint [7]. Experiments were conducted on healthy volunteers who were injected with irritating solutions into the capsule of the facet joint - and the patient experienced pain with the same irradiation as a person with back pain. After mapping the radiation patterns of pain caused by the facet joints in healthy volunteers, McCall et al. concluded that it is impossible to clearly determine the level of the affected joint [14].
Facet joint pain
High load on the joint and inflammation caused by dystrophic changes lead to severe pain.
In the subchondral plate of the inflamed joint, substance P, inflammatory mediators such as prostaglandins and cytokines (IL-6, TNFα), [7] calcitonin gene-related peptide (CGRP), dopamine, B-hydroxylase (DBH), vasoactive intestinal polypeptide (VIP), neuropeptide Y (NPY) [14]. Inflammation reduces the pain sensitivity threshold of nerve endings, which leads to persistent pain due to inflammation of the facet joints [15].
Long-term inflammation can lead to the development of secondary and primary central sensitization and the development of neuropathic pain [16].
Pain when the facet joints are affected may radiate. Pain patterns overlap (Figure 2) . It may extend to the buttocks or trochanter and distally. L1/L2 facet joints often have a central and lateral zone of pain irradiation. From levels L2/L3, pain radiates to the lower back, buttocks, hip joints and lateral thighs [17], L3/L4 - to the lumbar region, buttocks, hip joints, lateral thighs and groin area, L4/L5 - to the lumbar spine , buttocks, hip joints, back of the thighs and groin, L5/S1 - in the lower back, buttocks, sometimes hip joints, lateral thighs, groin and back of the thighs [14, 17, 18].
Rice. 2. Pain patterns.
a — irradiation of pain along the anterior surface; b — irradiation of pain along the posterior surface [7].
Diagnostics
Typical complaints are pain in the morning, corresponding to a mechanical nature, painful and difficult turning in bed, waking up at night from pain. During the day, the pain regresses slightly with movement, but intensifies with prolonged standing, sitting, or walking. It is difficult to get out of the car, and it is difficult to try to straighten the spine. It is painful to go down the stairs, while pain when going up stairs and when getting up from a chair is characteristic of damage to the sacroiliac joint [15, 19].
The irradiation is non-dermatomal in nature and does not extend below the knees. Upon examination, a positive Kemp's sign is revealed, pain when bending back with simultaneous pressing on the facet area, bending to the side [15, 20, 21]. Positive effect of taking non-steroidal anti-inflammatory drugs (NSAIDs) [1].
The diagnosis is made primarily clinically: pain in the back, buttocks, legs or groin, signs of muscle spasm, sensitivity of paravertebral points, pain with movement and the absence of other neurological signs, lasting more than 6 months [22].
The use of diagnostic blocks is central to the diagnosis of back pain caused by lesions of the facet joints, and is fundamental to the diagnosis of low back pain in general [15, 22, 23]. Patients with different localization of pain, but predominantly involving the facet joints, have a positive effect from the administration of local anesthetic. Fluoroscopically controlled blocks are the “gold standard” and can be compared with any clinical and radiological test for joint pain [1, 12, 15]. Facet joint osteoarthritis is a common radiographic finding, especially among older adults. Degeneration is characterized by narrowing of the joint space, sclerosis, bone hypertrophy and osteophytes. A CT scan can detect a narrowing of the joint space with subchondral sclerosis and erosions, bone proliferation and/or hypertrophy of the ligamentum flavum, which also causes narrowing of the intervertebral foramina [14]. Radiographic changes in osteoarthritis are equally common in patients with and without low back pain [14].
MRI has the advantage of assessing the extent of joint cartilage degeneration and its impact on surrounding neural structures [7], but MRI also does not correlate it with pain severity, which may be due to inflammation. There is effusion, proliferation, and dystrophic-atrophic processes in the periarticular muscles.
Most studies of the relationship between the severity of pain and findings using radiological diagnostic methods have levels of evidence C and D [22].
Treatment
Treatment of pain in the lower back begins with conservative methods - these are NSAIDs, simple analgesics, paracetamol, therapeutic exercise, massage [1, 12]. Intra-articular and para-articular injections of glucocorticosteroids (GCS) and radiofrequency denervation are also used [1].
The effectiveness of a particular treatment method depends on many factors; it is reported that the effect of intra-articular administration of GCS is maintained for 3-6 months [24]. The number of cases of musculoskeletal pain increases in the age group over 65 years, as somatic diseases progress and, in general, the level of physical activity decreases significantly [15].
The presence of comorbidity, as well as the side effects of NSAIDs (gastrointestinal toxicity, nephrotoxicity, side effects associated with the cardiovascular system) significantly limit their use, despite the fact that this treatment is pathogenetic in nature [25, 26]. The use of central analgesics and weak opioids does not reduce the level of the inflammatory response and can also cause serious complications [15, 27, 28].
The use of such non-pharmacological means as electrotherapy [29], acupuncture [30] and homeopathy, laser therapy, manual therapy [31], despite their widespread use in the Russian Federation, does not have a convincing evidence base.
An important role is played by therapeutic physical education (PT) [32]. However, exercise therapy is primarily aimed at treating the muscular-tonic component of pain.
Therapeutic and diagnostic blockades are pathogenetic in nature. Radiofrequency ablation (RFA) does not affect inflammation, but is effective in controlling pain. Blockade is a prerequisite for identifying the source of pain and is included as the first step in the diagnosis of facet joint syndrome by most associations of specialists involved in the interventional treatment of pain [22, 33].
Radiofrequency denervation has remained the method of choice for pain relief in facet joint lesions for more than 45 years. C. Shealy in 1975 was the first to use radiofrequency denervation of the facet joints [34]. According to various sources, its effect lasts up to 48 months [35, 36].
Radiofrequency denervation
Nerve fibers can be destroyed by physical means: heat (radio frequency), or cold (cryoneurolysis), or chemical means (alcohol/phenol).
The principle of radiofrequency denervation is as follows. The generator produces a sinusoidal current (400–500 kHz) [7]. Electrodes are placed on the target tissue. The electric field causes charged molecules to vibrate and generate heat in surrounding tissue. Coagulative necrosis occurs in the target tissue. The resulting lesion has the shape of a spheroid with a long axis along the active tip of the cannula. Most denervations are carried out at a probe temperature of 60-90 for 90-120 s; irreversible denaturation of the protein occurs. With pulse denervation, damage extends only to demyelinated C-fibers [37], due to which the transmission of the pain impulse ceases. The procedure is performed under the control of fluoroscopy or CT navigation [38].
Most studies report effectiveness in pain control over 6 months. For example, in a study by P. Dreyfuss et al. patients with pain in the lower back underwent thermocoagulation; there was a decrease in pain on a visual analogue scale (VAS) from 5 points before the procedure to 0.2 points after 3 months and the effect was maintained (1 point) up to 12 months. Selection criteria were: age 18-80 years, duration of back pain 6 months or more, pain in no more than two segments on both sides or no more than three segments on one side, ability to understand changes after diagnostic blockade. Assessment was carried out using VAS, Multidimensional Personality Questionnaire (MPQ), McGill Pain Questionnaire, Quality of Life Questionnaire (SF-36) and Rollan Morris disability questionnaire [39].
In a study by van Kleef et al. patients underwent radiofrequency denervation. As a result, pain reduction (not higher than 2 points on VAS) persisted for up to 12 months. Selection criteria: age 20–60 years, pain for 12 months, pain severity according to VAS 4–7 points, lack of effect from conservative therapy, absence of neurological deficit [40].
The study by S. Klessinger confirms the effectiveness of radiofrequency denervation for spondylolisthesis. Pain relief of up to 80% was maintained for more than 24 months. The average duration of pain relief in successfully treated patients was 10.9 months. The average follow-up time for 40 patients after RFA was 18.6 months (3–48 months). An 80% reduction in pain was observed for at least 6 months. Inclusion criteria: confirmation of spondylolisthesis by MRI and positive response to medial branch block. Exclusion criteria: back surgery, neurological deficit, spondylolytic spondylolisthesis, lack of response to medial branch blockade [41].
In a study by R. Paulsen et al. emphasis is placed on the importance of patient selection and diagnostic blockades. In this study, candidates were divided into two groups based on their response to two diagnostic blocks. It was found that patients with a pain reduction of up to 80% had a greater reduction in low back pain over the entire follow-up period, whereas patients with a pain reduction of up to 50-79% did not have a statistically significant reduction in pain. Inclusion criteria: age over 18 years, pain duration over 6 months, no use of corticosteroids. Assessment was carried out using the Quality of Life Questionnaire (EQ-5D), Oswestry Disability Questionnaire and VAS [42].
In a study by Q. Zhou et al. A comparison was made between the control group and the group with denervation of the facet joints, assessed by VAS after 30 minutes, 1 day, 1 week and 6 months. After 6 months, in the group with denervation of the facet joints, there was a decrease in pain to 1.7 points with an initial value of 6.7 points on the VAS. Inclusion criteria: duration of pain more than 6 months, characteristic pain in the buttocks, lower back (up to the knee), more pronounced in the morning, decreasing after movement, without neurological deficit. Patients with confirmed intervertebral disc herniation, stenosis, or spondylolisthesis were excluded. The condition was assessed using the Hospital Anxiety and Depression Scale (HADS) [43].
A. Conger et al. report pain relief of up to 80% of baseline within 6 months. The assessment was carried out using the VAS scale [44].
M. Chang reports the effectiveness of pulsed radiofrequency denervation of the facet joints at the thoracic level in patients with pain refractory to the administration of local anesthetics. VAS scores changed significantly over time: before treatment - 6.0±1.0 points, after 1 month - 3.3±2.2 points, after 2 months - 3.9±2.1 points, after 3 months - 4.0±2.2 points. Of the 20 patients, 11 (55%) reported successful pain control 3 months after denervation. The assessment was carried out only according to VAS. Inclusion criteria: pain for more than 6 months in the facet joints, age 20-79 years. Patients with intervertebral disc herniation, stenosis, myelopathy, thoracic spine fracture, suspected radiculitis, history of surgical treatment, infectious back diseases, blood coagulation disorders, iodine allergies, rheumatic diseases and uncontrolled somatic or psychiatric diseases were excluded [45].
Studies have also been conducted on combining radiofrequency denervation of the facet joints with exercise. Thirty-nine patients with facet joint disease underwent radiofrequency denervation. The patients were divided into two groups, one of the groups was given an additional set of exercises for 6 weeks. In the study group, pain decreased from 6 to 1 point according to VAS, in the control group - from 8 to 5 points. A significant effect was achieved in both groups, however, after 2 weeks, in the group of patients who performed exercises, the pain regressed completely, and in the group of patients who did not perform exercises, pain decreased by only 1 point on the VAS relative to the value that was after the procedure [46].
Similar data are also presented in the pharmacoeconomic review by E. Maas: the effectiveness of treatment in the group that combined interventional treatment and physical rehabilitation was significantly higher than in the group that used only one treatment method. The total cost of combination therapy was also lower [47].
Complications from radiofrequency denervation are extremely rare, the most common of which is neuritis, with an incidence of about 5% [48]. Negative results were most often obtained due to incorrect diagnosis, poor patient selection, and technical failures [24]. Despite some complications associated with facet joint blocks, they have been shown to be effective, safe, and reliable as a diagnostic tool. Denervation of the medial branch is promising for the permanent control of pain due to lesions of the lumbar facet joints [12].
Signs of arthrosis of the facet joints of the cervical and thoracic spine
Anatomically, the facet joints of the cervical spine can be classified as a flat type of structure. They are susceptible to destruction in the horizontal plane. The maximum physical load is placed on them when performing various movements. Deforming arthrosis of the facet joints of the cervical spine begins with long periods of static load:
- working on a computer;
- night rest in an uncomfortable position;
- wrong type of pillow for sleeping;
- the impact of the kinetic force of inertial movement during emergency braking while a car or train is moving;
- injury to the neck and surrounding muscle tissue;
- poor posture.
The facet joints of the thoracic region also have a flat horizontal structure. since this section does not have great mobility, arthrosis of the facet joints of the thoracic region rarely develops. But this disease causes severe pain and complete loss of mobility.
The main clinical signs of facet joint arthrosis include the following manifestations:
- pain in the affected area with irradiation along the radicular nerves (for example, with degeneration of joints in the cervical region, pain can spread through the arms, and if the process is localized in the lumbosacral region, through the legs);
- stiffness of movement in the morning and after a long period of being in one body position;
- crunching in the spine or clicking when performing certain movements;
- paresthesia, numbness, a tingling or crawling sensation in those parts of the body that are innervated by the radicular nerves located in those sections where the facet joints of the spine are destroyed.
When such signs appear, it is necessary to carry out differential diagnosis as quickly as possible, establish an accurate diagnosis and begin comprehensive treatment. For diagnosis, it is recommended to first carry out an x-ray examination. The photographs may show degenerative changes in bone tissue and narrowing of joint spaces. If radiographic images are not informative, the patient is recommended to undergo an MRI examination. In this case, the doctor has the opportunity to assess the condition of all structural parts of the spinal column.
It is important to exclude the possibility of developing ankylosing spondylitis - with it, the clinical manifestations are similar to spondyloarthrosis of the facet joints of the spinal column. But a blood test for rheumatic tests will allow for a correct differential diagnosis. The fact is that the treatment of ankylosing spondylitis differs radically from the treatment of this disease.
Facet syndrome
Arthrosis changes in the spine can develop after 25–30 years, which is facilitated by congenital anomalies of the spine (lumbarization, sacralization), hypermobility of the spinal segments and trauma. Among elderly people, the incidence of facet syndrome reaches 85–90% [2]. Etiology and pathogenesis The morphological basis of facet syndrome is spondyloarthrosis deformans. According to most authors, the terms “spondyloarthrosis” and “facet syndrome” are synonymous. However, some researchers argue that the term “spondyloarthrosis” has a more general meaning, since the degenerative process usually involves the facets, capsule of the intervertebral joints, ligamentum flavum and other periarticular tissues. The term "facet syndrome" implies more specific clinical symptoms from a specific joint.
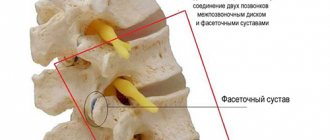
Anatomy of the facet joint. Facets (synonyms: facet joints, articular processes) extend from the vertebral plate and participate in the formation of facet joints (Fig. 1). Two adjacent vertebrae are connected by two facet joints located on either side of the arch, symmetrically relative to the midline of the body. The arcuate processes of adjacent vertebrae are directed towards each other, and their ends are covered with articular cartilage. The ends of the articular processes are enclosed in an articular capsule. Due to the presence of facet joints between the vertebrae, a variety of movements are possible, and the spine is a flexible, movable structure [1]. The anatomical structure of the spinal column emphasizes the purpose of its anterior sections (anterior longitudinal ligament, vertebral bodies, intervertebral discs) mainly to resist gravity (compression), and the posterior sections (intervertebral joints, pedicles, transverse and spinous processes, plate) - to protect against axial rotatory and displacement forces in the anteroposterior and lateral directions. The distribution of gravity forces in a normal spinal motion segment, which includes a 3-joint complex, occurs as follows: from 70 to 88% falls on its anterior sections, and from 12 to 30% on the posterior, mainly intervertebral (facet) joints, although both parts of the spine experience stress when exposed to any forces. When discs are damaged, where degenerative changes in the spine most often begin, the weight load gradually shifts to the intervertebral joints, reaching from 47 to 70%. Such overload of the joints leads to successive changes in them: synovitis with the accumulation of synovial fluid between the facets; degeneration of articular cartilage; stretching of the joint capsule and subluxation in them. Continued degeneration due to repeated microtrauma, weight-bearing and rotatory overloads leads to periarticular fibrosis and the formation of subperiosteal osteophytes, increasing the size of the upper and lower facets, which become pear-shaped. Eventually the joints degenerate dramatically, losing almost all cartilage. Quite often, this process of degeneration occurs asymmetrically, which is manifested by uneven loads on the facet joints. The combination of changes in the disc and facet joints leads to a sharp limitation of movements in the corresponding motion segment of the spine.
The vertebral segment includes not only the cartilaginous disc between adjacent vertebrae and the facet joints, but also the ligaments and muscles connecting them: intertransverse, interspinous and rotator cuff muscles. These muscles, under the influence of impulses from the affected spinal segment, especially from the posterior longitudinal ligament, reflexively tense, and a muscular-tonic syndrome is formed [3]. An important role in the formation of facet syndrome is played by a violation of articular tropism, i.e., the asymmetrical arrangement of the facet joints. The linear arrangement of the facet joints deserves special attention. In the cervical region, the facets are located horizontally (transversely), with a slight posterior-inferior deviation. In the thoracic region, the facet joints are located at a lower level (relative to the vertebral body) and can be compared to the location of the nerve root (horizontal in the neck and downward in the thoracic spine). In the lumbar region, the facet joints are located sagittally at the first and second vertebrae and almost coronally (i.e., parallel to the coronal suture or perpendicular to the lateral surface of the vertebral body) at the 3rd–5th vertebrae. Sometimes the facet joint is located in the sagittal plane on one side, and in the coronal plane on the other side. Such anomalies of tropism occur in many people and are considered a predisposing factor for additional rotational load on them [2].
Clinical picture Features of the anatomical structure of the facet joints determine their most common lesions in the cervical (55%) and lumbar (31%) parts of the spine. With facet syndrome, pain increases with extension and decreases with flexion. The pain can radiate paravertebrally, to the shoulder, buttock. Referred pain emanating from the intervertebral joints is lateralized, diffuse, difficult to localize, and has a sclerotomal distribution. Sometimes the pain radiates to the limb, but does not extend below the elbow or popliteal fossa. Facet pain may be more or less cramping. Characterized by the appearance of short-term morning stiffness, lasting 30–60 minutes, and an increase in pain towards the end of the day. The pain intensifies from prolonged standing, extension, especially if it is combined with bending or rotation to the painful side, when changing body position from lying to sitting and vice versa. Unloading the spine - bending it slightly, taking a sitting position, using support (stand, railing) reduces pain [3]. Characteristic signs of pain caused by facet syndrome: – the onset of pain is associated with rotation and extension of the spine; – pain has a lateralized diffuse nature; – irradiation of pain does not spread far from the affected area; – characterized by morning stiffness; – pain increases in static positions; – warming up and unloading the spine reduces pain. Diagnosis There are no pathognomonic symptoms characteristic of facet joint lesions. Upon examination, smoothness of the cervical and/or lumbar lordosis, rotation or curvature of the spine in the cervicothoracic or lumbosacral regions are detected. Tension of the paravertebral muscles and quadratus dorsi muscle is detected on the sore side. Local tenderness may be detected over the affected joint. The muscle tension around the intervertebral joint is determined by palpation. Unlike radicular syndrome, symptoms of prolapse are not typical. Sometimes, in chronic cases, some weakness of the erector spinae and popliteal muscles is detected. Thus, a clinical feature of diagnostic significance is pain in the spine, aggravated by extension and rotation with localized pain in the projection of the facet joint [4]. X-ray examination and computed tomography reveal hypertrophy of the intervertebral joints and the presence of osteophytes on them. With active arthrosis, radionuclide scintigraphy detects the accumulation of the isotope in the intervertebral joints. The final diagnosis of facet syndrome is established after the positive effect of para-articular blockade with local anesthetic of the suspicious intervertebral joint.
Treatment In the treatment of pain with facet syndrome, it is rational to use non-steroidal anti-inflammatory drugs (NSAIDs), which have a good analgesic and pronounced anti-inflammatory effect. The mechanism of action of NSAIDs is to suppress the activity of the enzyme cyclooxygenase (COX), which plays a leading role in the synthesis of prostaglandins, which enhance the inflammatory process and are directly involved in the formation of pain.
One of the most proven NSAIDs in practice is Xefocam (lornoxicam). Xefocam is a non-selective NSAID belonging to the group of oxicam derivatives. Thanks to the balanced inhibition of COX-1/COX-2, Xefocam combines pronounced analgesic and anti-inflammatory activity with a low risk of adverse events (AEs) [8]. Xefocam has a shorter half-life (3–4 hours) than other oxicams. It has been established that a longer half-life of NSAIDs in blood plasma is associated with an increased risk of AEs. Consequently, the rapid removal of Xefocam from the body helps reduce the incidence of AEs, especially from the gastrointestinal tract [9]. A feature of Xefocam is the stimulation of the production of endogenous dynorphin and endorphin, which indicates the drug’s ability to influence the central links in the pathogenesis of pain. The dual route of excretion of the drug (through the kidneys and gastrointestinal tract, bypassing the enterohepatic circulation) reduces the load on organs and improves tolerability, therefore, in case of mild to moderate degrees of hepatic and/or renal failure, dose adjustment is not required [5]. Thus, Xefocam is well tolerated compared to other NSAIDs.
Since facet syndrome is more common among older people, good tolerability of Xefocam becomes a priority factor when choosing NSAIDs. On the pharmaceutical market, Ksefokam is presented in the following dosage forms: – Ksefokam – standard tablets of 4 and 8 mg; – Xefocam lyophilisate – for preparing a solution for intramuscular and intravenous injections, 8 mg of lornoxicam in 1 bottle; – Xefocam Rapid – quickly absorbed tablets 8 mg. The recommended dose for a single dose of Xefocam is from 4 to 8 mg, the maximum daily dose is 16 mg with intervals between doses of 8–12 hours. The analgesic effect develops within 45–60 minutes when using standard tablets and lasts 8 hours [7]. A feature of the Xefocam Rapid form is the speed of onset of the analgesic effect - 30 minutes after administration, which is achieved due to the rapid absorption of the drug already in the stomach [6].
With the development of reflex muscular-tonic syndrome, the prescription of muscle relaxants is indicated. Muscle relaxants, eliminating muscle tension, interrupt the vicious circle “pain - muscle spasm - pain”. Treatment with muscle relaxants begins with the usual therapeutic dose and continues while the pain syndrome persists; As a rule, the course of treatment lasts several weeks. Taking into account the leading pathogenetic role of degenerative-dystrophic processes of intervertebral joints in the development of facet syndrome, the use of structure-modifying therapy (chondroitin sulfate and glucosamine) - drugs that help slow down the degeneration of cartilage tissue - is justified. The use of chondroprotectors is recommended already in the early stages of the development of this pathology [2]. In order to reduce pain, in addition to medications, magnetic therapy, sinusoidally modulated currents, ionogalvanization with painkillers (procaine or lidocaine), phonophoresis with hydrocortisone to relieve swelling and inflammation, massage and therapeutic exercises are used.
If conservative therapy is ineffective, surgical treatment is used. The most effective treatment method, recognized throughout the world, is radiofrequency denervation (destruction), in which the pathological process is eliminated by exposure to an electromagnetic field of wave frequency in the immediate vicinity of the affected joint. With this technique, it is possible to influence several diseased segments of the spine at once. This procedure, while effective in 80% of cases, does not require general anesthesia, an incision in the skin, lasts about 30 minutes, after which the patient leaves the clinic on his own after about 1 hour. Radiofrequency destruction of the medial branches of the dorsal roots of the spinal nerves (facet rhizotomy) effectively denervates the facet joints and provides long-term, high-quality pain relief. A successful facet rhizotomy typically provides pain relief for more than a year.
Prevention Since up to 80% of the population encounters manifestations of facet syndrome sooner or later, maintaining an active lifestyle will help delay their onset. Daily physical exercise, measured walking, and visiting a swimming pool ensure the formation of correct biomechanics of the spinal column, maintaining adequate blood circulation in the intervertebral joints, and strengthening the muscular frame. This allows you to maintain functional mobility of the spine for many years.
Literature 1. Putilina M.V. Dorsopathy of the thoracic spinal column. A manual for doctors. M., 2009. 104 p. 2. Gorbacheva F.E. Spondyloarthrosis of the spine: diagnosis and treatment. M., 2007. 12 p. 3. Gorbacheva F.E. What is hidden under the mask of spinal osteochondrosis? M., 2008. 12 p. 4. Yakhno N.N. Pain. Guide for doctors and students. M., 2009. 304 p. 5. Grishaeva T.P., Balabanova R.M. The use of Xefocam (lornoxicam) for the relief of acute and chronic pain syndrome // RMZh. 2005. T. 15. pp. 1009–1011. 6. Danilov A.B., Gak S.E. Xefocam (lornoxicam): possibilities of use for the treatment of pain syndromes // Breast Cancer. Pain syndrome. 2011. pp. 37–39. 7. Nycomed. Xefocam Monograph // medi.ru – 2008.03. 8. Hamza Yel-S., Aburahma MH Design and in vitro Evaluation of novel-release double-layer tablets of Lornoxicam: Utility of cyclodextrin and xanthan gum combination // AAPS Pharm Sci Tech. 2009. Vol. 10. P. 1357–1366. 9. Jiao H., Kut F. Pretreatment with lornoxicam, a cyclooxygenase inhibitor, relieves postoperative immunosuppression after total abdominal hysterectomy // Tohoku J. Exp. Med. 2009. Vol. 219. No. 4. P. 289–294.
Treatment of arthrosis of the facet joints of the lumbar spine
Arthrosis of the facet joints of the lumbar region, as well as the thoracic and cervical ones, is easily treated with conservative treatment in the early stages. Unfortunately, with severe deformation of the structural parts of the joints, it will no longer be possible to completely restore the layer of cartilaginous synovial tissue. But it is possible to restore at least partially lost mobility to the back.
We recommend starting treatment for facet joint arthrosis at the stage of primary clinical signs. To do this, it is advisable to contact a chiropractor or osteopath. A vertebrologist also treats this pathology. These specialists have sufficient knowledge and experience to develop individual treatment for facet joint arthrosis.
Osteoarthritis of the facet joints of the lumbar spine is characterized by the fact that pain increases rapidly. With total damage to the joints, a person quickly loses his ability to work. Painful sensations occur even in a lying position, in the evening and at night.
Correctly developed treatment allows you to restore mobility and relieve pain. Complex therapy begins with traction traction of the spinal column. This procedure allows you to restore the anatomical structure of the facet bone articulation. then an individual course is developed, which may include manual therapy, osteopathy, massage, reflexology and kinesiotherapy. A properly developed complex of therapeutic exercises can prevent the risk of relapse of the pathology in the future.
It is important to follow all recommendations of your doctor. Sign up for a free initial consultation with a vertebrologist at our manual therapy clinic. You will be given individual recommendations for diagnosis and treatment.