- Spinal injuries
- Congenital anomalies of the spine
- Hereditary predisposition
- Autoimmune diseases: ankylosing spondylitis, rheumatoid arthritis
- Pathological posture: scoliosis and other deformities of the spinal column
- Osteochondrosis, spondylitis, spondylolisthesis
- Long-term static loads on the spine
- Hard physical labor, intense sports activities
- Endocrine pathologies: hypothyroidism, diabetes, obesity
- Deficiency of vitamins, macro- and microelements
- Physical inactivity
- Specific (tuberculosis, syphilis) and purulent infections
Arthrosis of the intervertebral joints in the early stages of development is asymptomatic.
As the pathological process progresses, symptoms indicating spinal arthrosis also increase.
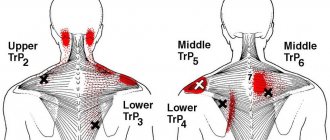
Cervical osteoarthritis is characterized by:
- Limitations in head movements
- Pain in the neck
- The appearance of a crunching, clicking sound when turning or tilting the head
- Deterioration of vision, hearing
- Tinnitus, loss of coordination
- Skin sensitivity disorder of the upper extremities
Symptoms of arthrosis of the thoracic spine:
- Stiffness, pain in the chest
- As the disease worsens, respiratory distress may appear, and the pain intensifies with breathing movements.
Signs of lumbar spondyloarthrosis:
- Feeling of heaviness in the lumbar region
- Pain in the lumbosacral spine of varying nature and intensity, aggravated by body movements.
- Stiffness in the area of the affected joint: inability to sit or stand independently.
- Sometimes paresthesia of the lower extremities develops: numbness, pain, weakness in the legs.
Stages of development of spinal arthrosis
According to the degree of development of dystrophic changes, arthrosis of the intervertebral joints is divided into stages:
- Stage I. Initial metabolic disorders begin to occur in the cartilage tissue, which, most often, are asymptomatic. There are no signs of arthrosis on the X-ray. The patient is sometimes bothered by discomfort in the back after physical activity.
- Stage II is characterized by the appearance of stiffness in the back in the morning or after a long stay in one position, as well as moderate pain, especially after sudden movements of the body: bending, turning. The x-ray shows thinning of the cartilaginous plate of the articular surfaces, marginal bone growths (osteophytes).
- Stage III. With the progressive destruction of cartilage, the ligamentous-muscular apparatus of the spine suffers, ensuring the correct anatomical position of the vertebrae and the stability of the spinal column. The x-ray shows a narrowing of the interarticular space and a massive proliferation of osteophytes. The pain is constant both at rest and with movement. There is stiffness in the damaged segment of the spine.
- Stage IV. The x-ray shows that the cartilage is completely destroyed, there is no joint space. The slightest movements cause excruciating pain.
Diagnosis of facet syndrome
To diagnose facet syndrome, blockade of the medial branch of the posterior primary branch of the spinal nerve or intra-articular injections of local anesthetic under neuroimaging control are used. The disappearance of pain within a few minutes after a diagnostic blockade is considered the standard for linking back pain with the pathology of the facet joints. It has been shown that diagnostic blockades without appropriate x-ray control lead to false positive results in 25-41% of cases.
How to diagnose
The diagnosis is made based on the patient’s complaints, medical history, clinical examination, examination data, which includes laboratory tests and instrumental methods.
Radiography –
reveals the condition of bone tissue and articular cartilage.
Magnetic resonance imaging
detects changes in intervertebral discs, ligaments, nerve plexuses, blood vessels, and spinal cord.
For the purpose of differential diagnosis, tests are performed to exclude or confirm other diseases:
- General blood analysis
- Biochemical blood test with rheumatological tests
Causes of facet syndrome
There are a large number of reasons leading to damage to the joints of the spine. Pain in the intervertebral joints can be associated with acute and chronic infectious lesions (for example, tuberculous spondylitis), systemic inflammatory arthritis (rheumatoid arthritis, spondyloarthritis), metabolic disorders (gout and pseudogout). Potential causes of back pain may include subluxations, ruptures of the joint capsule and cartilage, and microfractures, but the role of these changes remains unknown. The most common cause of back pain associated with damage to the facet joints is considered to be dystrophic changes (spondylarthrosis or facet syndrome).
In the vast majority of cases, damage to the facet joints is the result of many years of repeated trauma associated with a suboptimal range of motion in the joints and increased load on them due to degeneration of the intervertebral discs. In some cases, damage to the facet joints can develop acutely, for example, in cases of whiplash injury to the neck, in sports injuries, when there is trauma to the joint due to hyperflexion, excessive rotation or traction mechanism.
Spinal arthrosis: causes, symptoms, treatment
Causes
Arthrosis is very rare in young people. In most cases, this diagnosis is made to older people. In the younger generation, this disease occurs only in cases of spinal injury in the past, if the person has any defects in the structure of the spinal column, disorders of the spinal disc, or excess body weight.
If the spine has already been damaged, it often happens that the joints begin to wear out as a result. This issue is especially acute for overweight people, since in this case the joints are at risk even without injury.
Since the cartilage tissue becomes much thinner than before, this leads to pain in the back. Due to painful sensations, a person tries to change the position of the body, which leads to overload of the spinal column and significantly complicates the situation.
Since with age, irreversible aging processes occur in the body and, as a result, disruption of the nutrition of cartilage, ligaments, and joints. All this leads to the fact that the synovial fluid loses its functions and this is what becomes the cause of arthrosis.
Signs
Frequent pain is often the main indicator of arthrosis. As a rule, they are felt in a specific area of the spine. But if the disease is already in an advanced stage and osteophytes have appeared, the joints become inflamed, quite painful sensations may appear during any movement and discomfort in the spine in the morning, which is associated with hypertonicity of the muscles of the spinal column.
Diagnostic tests
To establish an accurate diagnosis, the doctor will necessarily analyze everything that the patient tells him about his condition and prescribe all the necessary tests. As a rule, this is a biochemical blood test, radioisotope scanning, radiography and magnetic resonance imaging. In order for the doctor to rule out a head disease, the patient is often also prescribed an ultrasound of the brain.
Treatment methods
To improve the patient’s health and cure the disease, the doctor prescribes the necessary medications, attending physical therapy, following a certain diet, using external medications, which are usually specialized ointments or rubs, physiotherapeutic procedures and surgery. Treatment of spinal diseases is always difficult and time consuming. Therefore, the patient must perform all the procedures prescribed by the doctor in combination to obtain a high-quality result.
In cases where parts of the spine are already affected by arthrosis, the doctor must prescribe painkillers and anti-inflammatory drugs. The use of muscle relaxants is also usually prescribed in order to relieve muscle tone.
If arthrosis or spondyloarthrosis, as it is also called, is only in the initial first stage, chondroprotectors that help restore intervertebral discs and medications designed to improve blood circulation are very helpful in its treatment. For the same purpose, abdominal decompression can be prescribed, in which artificial negative pressure is applied to the lower part of the person’s body. This not only helps increase blood circulation, but also helps slow down or completely eradicate inflammatory processes in the body.
A noticeable improvement in the patient’s condition occurs after regular visits to physiotherapeutic procedures such as acupuncture or reflexology, as it is also called, phonophoresis and magnetic therapy.
If the use of medications, attending procedures, following a special diet do not produce positive results and the disease does not recede, the patient must undergo surgery.
Usually it consists of replacing vertebrae damaged by arthrosis with artificial ones. Or doctors perform thermal disconnection of the patient’s nerve endings, which is called “denervation surgery.” Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Causes of pathology
Arthrosis of the joints of the spine can be primary or secondary. Primary forms occur for no apparent reason and, according to scientists, are caused by genetic predisposition or metabolic disorders. Secondary varieties are formed against the background of infectious diseases of the musculoskeletal system, osteoporosis, hormonal imbalances, osteochondrosis, gout, chondrocalcinosis and other diseases.
Factors that increase the risk of developing the disease include increased load on the lower back (heavy lifting, poor exercise technique), vibration damage, injuries, and hypothermia. Pathology also occurs in people who lead a sedentary lifestyle and do not have a strong muscular frame of the back.
Arthrosis of the spinal joints - etiology and pathogenesis
With deforming arthrosis of the facet joints of the spine, as with various types of osteoarthritis, dystrophic changes in the cartilage tissue of the joint, thinning and destruction of cartilage, as well as the formation of osteophytes are observed.
Most often, arthrosis of the vertebral joints develops in combination with other dystrophic changes in the spine (chondrosis, osteochondrosis). But localized development of this form of arthrosis is also possible - with spinal deformities (hyperlordosis, scoliosis).
The joints of the cervical spine are most often affected by deforming arthrosis, and it is this type of spondyloarthrosis that gives the most pronounced symptoms. Arthrosis of the lumbar intervertebral joints is clinically asymptomatic for a long time, or local pain occurs, typical of deforming arthrosis of any localization.
Lumbar spondyloarthrosis
Treatment of the disease in the vast majority of cases is conservative. Non-drug therapy, including massage and physical therapy, plays a critical role. Massage reduces muscle spasm, promotes blood circulation and tissue metabolism in the affected area. Exercise therapy helps reduce pain and restore the functional activity of the spine. In parallel, physiotherapeutic procedures are prescribed: ultrasound, electrophoresis of cobalt, sulfur and zinc, phonophoresis with hydrocortisone and magnetic therapy.
To reduce acute pain in the absence of signs of severe inflammation, use paracetamol or tramadol. In the presence of inflammatory phenomena, NSAIDs are prescribed: celecoxib, meloxicam, nimesulide, ibuprofen, diclofenac, etc. Along with tablet forms, anti-inflammatory and warming gels and ointments are used. For severe spasms, muscle relaxants are used: tizanidine, tolperisone and baclofen. In addition, in recent years, for arthrosis of various localizations, including spondyloarthrosis, along with the drugs listed above, chondroprotectors are increasingly being prescribed: marine fish extract, glucosamine, chondroitin sulfate, etc. These drugs prevent the progression of degenerative changes in cartilage tissue and slow down development of spondyloarthrosis.
For persistent pain syndrome, blockades with novocaine and cortisone are performed in the area of the facet joints. In addition, if there is no effect from conventional treatment, minimally invasive radiofrequency destruction of pain receptors in the area of the affected joints is sometimes performed. The procedure is well tolerated by patients and is performed in a clinic setting.
If conservative treatment is ineffective in young patients, in some cases surgical operations are performed, during which the doctor installs special implants - interspinous spoilers - between the spinous processes. These structures help to widen the intervertebral openings and reduce the load on the spinal discs. The operation belongs to the category of relatively low-traumatic surgical interventions and can be performed under local anesthesia, both in a hospital setting and on an outpatient basis. This expands the possibilities of using the technique in the treatment of elderly patients, who often suffer from concomitant somatic diseases and have difficulty with general anesthesia and extensive operations.