Lumbodynia or chronic lower back pain is not uncommon. For example, in the United States, low back pain is the second most common neurological ailment after headaches. Often, chronic low back pain leads to long-term loss of ability to work, and in a certain percentage of cases, to disability. As a rule, acute lower back pain is most often caused by injury or inflammation (arthritis) and lower back pain usually lasts from several days to several weeks. Acute pain can also be caused by pathology of the internal organs and be of a reflected nature. Some acute pain syndromes can lead to serious complications if not properly treated.
Chronic low back pain is pain that lasts more than 12 weeks (3 months). Chronic lower back pain can progress and sometimes it is not possible to find out the true cause of lower back pain.
What is lumbodynia
Pain with lumbodynia can be chronic or acute/subacute, but in any case it is caused by spinal pathology. Lumbodynia syndrome is considered a sign of osteochondrosis of the lumbar spine, although often with this diagnosis there may be no pain at all. The severity of pain can vary and depends on the individual and a combination of a number of factors. It occurs mainly in people of working age (25-45 years).
Lumbar pain can be localized only on one side or on both (right-sided, left-sided, symmetrical). It most often worries in the lower lumbar region and can radiate to the gluteal region (one or both buttocks).
Diagnosis of vertebrogenic syndrome.
To make a diagnosis and prescribe treatment, you must contact a neurologist.
The doctor will ask you in detail about the type and nature of pain, study your medical history, and ask about genetic abnormalities, lifestyle and work activity.
The doctor can determine the displacement of the vertebrae by feeling the spinal column.
Afterwards he will prescribe tests on the devices.
Criteria for diagnosis:
- pain in the cervical, thoracic, lumbar and sacral regions;
- if the pain intensifies with movement;
- if using a corset or lying down the pain decreases;
- if you have to provide support with your hands when standing up;
- if when walking the gait becomes swaying;
The studies that give the most effective results are considered to be computed tomography (CT), which studies the affected area in detail, and magnetic resonance imaging (MRI), which helps to detect the cause of blood flow disturbances.
If the case is not advanced, sometimes it is enough to take an x-ray.
Kinds
Vertebrogenic lumbodynia is the main manifestation of the chronic form of osteochondrosis (lumbar zone) and is more often characteristic of men. Can have any duration (last from several weeks/months to several years). If the cause of pain is diseases of the intervertebral disc (herniation, protrusion), then lumbodynia is called discogenic.
In addition to the above, “classic” one, there are other types. It can be combined with nagging pain in one or both legs (sciatica), in which case it is called lumboischialgia. (left-handed or right-handed). Depending on the distribution (on one or both limbs). Accompanies the non-radicular phase of lumbar osteochondrosis.
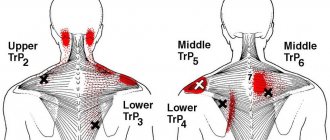
When the pain is intensified not only by movements, but even by the slightest activity, such as talking, sneezing, bending over, then this type is called lumbodynia with muscular-tonic syndrome. Often, there is a moderate curvature of the spine, causing pronounced reflex tension in the lower back muscles (bilateral or unilateral), which provokes pain.
Chronic type
Although acute back pain is common, the basis of vertebrogenic lumbodynia is made up of chronic degenerative-dystrophic processes. The disease takes a protracted course with autoimmune damage, in the presence of unoperated intervertebral hernias. The main signs of chronic lumbodynia:
- prolonged aching pain;
- duration of incapacity for work – at least 3 months per year;
- weak effect of NSAIDs;
- significant improvement with the use of hormones, cytostatics and antidepressants;
- persistent signs of spinal damage on x-ray.
The pain is often unilateral, less often bilateral, which is associated with asymmetrical compression of the spinal roots. If the symptoms spread to both parts of the back and lower extremities, then we are talking about a tumor or autoimmune process. In this case, the prognosis is always serious; a thorough detailed examination using magnetic resonance or computed tomography is required. Right-sided lumbodynia is somewhat more common, since the force of the load is distributed unequally. People who are right-handed, and these are the majority in nature, tend to load this half of the body with physical effort. As a result, the muscle corset sags, and the degenerative-dystrophic process progresses, which inevitably leads to right-sided pain syndrome.
One of the types of chronic spinal lesions is post-traumatic lumbodynia. There is always an indication of trauma in the anamnesis, usually in the form of a compression fracture or surgical correction. Clinical remission is difficult to achieve, since the organic nature of osteoarticular changes prevents effective therapy with conservative means. Such patients are assisted by a neurologist together with a neurosurgeon, since it is often necessary to switch to surgical treatment tactics.
Causes of lumbodynia
Low back pain (lumbodynia), both chronic and acute, is most often caused by pathological processes (degenerative-dystrophic) in the spine, especially in the lumbar region. In addition to osteochondrosis, lumbodynia is caused by its complications, such as protrusion, spondylolisthesis, intervertebral hernia, spondyloarthrosis, spondylosis.
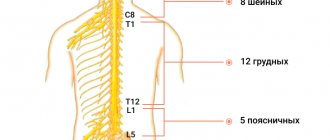
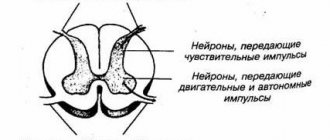
The mechanism of lumbodynia is based on irritation of the nerves (especially sinuvertebral). Pain is especially pronounced with cracks in the fibrous ring. Also the cause is abnormalities in the development of the lumbar spine.
Pain can occur after a single physical overload, lower back injuries, hypothermia, stress, sudden turns of the body, hypothermia, exposure to drafts, prolonged exposure to an uncomfortable or monotonous position. Moreover, lumbodynia can manifest itself not only after a few days or weeks, but even several months after the provoking factor.
The risk group also includes those who are overweight, have certain chronic diseases, have infectious diseases, workers in hazardous industries, those who experience increased stress, lead an adynamic lifestyle, or are in an uncomfortable or the same body position for a long time.
Treatment and prevention of vertebrogenic pain syndrome
Experts advise treating pain syndrome in a comprehensive manner:
- Preventive methods . In the first few days it is better to stay in bed. Eliminate physical activity, sit less. Use orthopedic mattresses and pillows, wear special corsets and a collar.
- Medication methods. Use analgesics, non-steroidal and anti-inflammatory drugs: diclofenac, relanium, ketorol, ketoprofen, nimesulide, piroxicam. To block prolonged pain, nerve blockades are prescribed using lidocaine, novocaine, diprospan, hydrocortisone.
- Unconventional methods. These methods include the use of:
- manual therapy for realignment of vertebrae;
- osteopathy to correct and suppress the symptoms of pain and eliminate it;
- reflexology to relieve nerve tension;
- hirudotherapy, which relieves swelling;
- homeopathy to eliminate disturbances in the functioning of internal organs.
Physiotherapy, magnet and ultrasound therapy help prevent the development of exacerbation of pain syndrome.
If after using all treatment methods the pain does not go away, experts recommend surgery.
Remember that timely contact with specialists will help not only get rid of vertebrogenic pain syndrome, but also prevent its consequences, which may be irreversible.
Symptoms
With vertebral osteochondrosis, lumbodynia is aching in nature and is more pronounced in the morning. May have different durations, decrease or increase during the day. There are provoking factors that increase or decrease the intensity of lumbodynia. For some it is caused by activity, while for others it is its absence; accordingly, opposite actions ease the pain. A combination of these manifestations may occur in the same person.
Pressure on the vertebrae and paravertebral areas in the lumbar area is usually painful. In addition, bending and many other movements are difficult and most often accompanied by pain. Patients have difficulty bending, especially forward, and the angle of inclination of the torso becomes limited. There may be sharp pain in response to palpation of the exit point of the sciatic nerve on the thigh.
Doctors explain the subsidence of pain in the lying position by reducing the load on the lumbar intervertebral discs. Patients intuitively or consciously find the most comfortable position (in which the pain is least pronounced). Most often, this is a position lying on your side with your legs bent.
At first, there is moderate lumbodynia, gradually the pain intensifies, but does not reach the same degree of severity as with lumbar pain (lumbago), also called acute lumbodynia. Patients can move around and do work, but the quality of life is significantly reduced.
Spondylogenic type
Damage to the intervertebral joints and vertebral processes is the basis of spondylogenic lumbodynia. It is most often autoimmune in nature, as it is associated with systemic damage to osteochondral tissue. Discogenic lumbodynia is caused by changes in the intervertebral space due to joint deformation. This leads to damage to the spinal roots, and subsequently the sciatic nerve is involved in the process. Pain in the spine, radiating to the leg and buttock with damage to the sciatic nerve, is called “sciatica.” The typical pain syndrome is felt more in the leg, which makes even simple movements of the limb difficult.
Typical signs of spondylogenic lumbodynia of an autoimmune nature with sciatica can be presented as follows:
- severe pain in the buttock and leg;
- severe limitation of movements in the limb;
- slight low-grade fever;
- severe emotional lability of the patient;
- reaction of acute-phase blood parameters with the systemic nature of the disease;
- bilateral changes in the joints on CT or MRI examination.
The patient's vertical posture is especially difficult, but what is it? This means that the patient cannot stand in a standing position for even a few seconds due to severe pain in the leg. The problem disappears after drug stabilization of the patient's condition.
Diagnosis of lumbodynia
Lumbodynia can be diagnosed in different ways. A neurologist diagnoses this disease. The most common is a clinical examination and questioning of the patient, combined with static and dynamic examination of the spine, as well as manual diagnostics. Additionally, the organs of the pelvic and abdominal cavities are examined to exclude diseases that are a source of referred pain. In addition, MRI, radiography, and ultrasound diagnostics will not be superfluous. During the examination, lumbodynia is differentiated from myositis of the spinal muscles and pathologies of the hip joint.
IMPORTANT! Lumbodynia is a serious symptom that can tell a person about significant problems in the lumbar spine, ranging from inflammatory phenomena to destructive diseases. That is why, if you have lumbodynia, you cannot self-medicate, but you should definitely consult a specialist!
Experienced doctors at the Kuntsevo Medical and Rehabilitation Center will conduct a thorough diagnosis and understand the causes of the symptom. A treatment plan for the patient will then be drawn up. Make an appointment with our doctor and take a step towards getting rid of lumbodynia!
Sign up
Accurate diagnosis is the key to successful treatment
The arsenal of modern medicine includes non-destructive neuroimaging methods that allow us to obtain a complete picture of the processes taking place. When it comes to neurological pathologies, the most important method is MRI. Magnetic tomography clearly visualizes the spinal cord roots, vessels and soft tissues, joints, discs and vertebrae. You can choose a clinic with a powerful device, suitable opening hours and low prices on our website.
You can find out whether the clinic does MRI with contrast, whether they accept children, whether you can consult with a specialist after the examination, whether it is possible to undergo the procedure with sedation, etc.
Treatment with manual therapy
You can get rid of lumbodynia only by eliminating the causes that caused it. This type of treatment can be considered complete. In other cases, the help will have a temporary effect and after some time, lumbodynia will appear again, and if the treatment was inadequate, it will intensify or recur. It is important to find a good chiropractor, otherwise you may not only not be cured, but even make things worse.
Since the main cause of lumbodynia is considered to be vertebral osteochondrosis, the cause of which, in turn, is improper functioning of the spine, it is not lumbodynia that should be treated, but osteochondrosis. In addition, by getting rid of osteochondrosis, you will protect yourself from the occurrence of its complications, such as hernias and disc protrusions.
Manual therapy is considered one of the most effective ways to eliminate problems in the spine. It is especially effective in combination with the subsequent implementation of a complex of physical therapy (physical therapy). All this not only improves the condition, but also stimulates recovery processes, thanks to which the course of the disease can sometimes not only be stopped, but also reversed.
The number of procedures is prescribed individually, based on the patient’s health characteristics, stage of the process, complications, and concomitant diseases. It is also necessary to perform exercise therapy to consolidate the achieved result and maintain it after treatment.
Recovery Exercises
Physical therapy is an important part of the treatment of the disease. However, before you start training, it is important to establish the causes of lumbodynia. If there is a compression fracture, then bed rest with gentle exercise is indicated. Novocaine blockade often helps with severe pain.
The full set of exercises can be viewed here:
Physical activity should be combined with other non-drug methods of assistance. Massage is especially effective for chronic pathologies. It is advisable to conduct his sessions no more than 2 times a year. Can there be a temperature with lumbodynia? This question cannot be answered unequivocally. There should not be a high temperature reaction, but a slight low-grade fever due to an autoimmune process or excessive emotional outbursts is possible.
To alleviate the condition, hormones, cytostatics and psychocorrectors are prescribed. But what antidepressants can be taken in combination with exercise? According to neurologists, there are no serious restrictions on taking these drugs. Modern antidepressants can be used long-term.