Back pain that occurs due to osteochondrosis is a common occurrence. You can get rid of them only after proper therapy. However, most people, citing a lack of free time, prefer to endure discomfort, which only aggravates the problem. Then the pathology continues to progress, causing dangerous complications.
Osteochondrosis with radicular syndrome is manifested by a whole complex of symptoms that arise as a result of compression of the spinal nerves. This condition develops as a result of long-term degenerative-dystrophic changes in the intervertebral discs. As a rule, the result of such disorders is an intervertebral hernia, which further injures the spinal roots. Radicular osteochondrosis requires long-term and complex treatment.
Causes
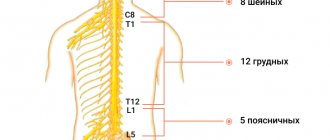
Radicular osteochondrosis is a consequence of damage to the nerve roots that exit the spinal cord. These branches innervate the skin, skeletal muscles, diaphragm, and internal organs.
When nerve bundles are damaged, a sharp shooting pain appears that spreads to different parts of the body. In addition, the sensitivity of the area for which the inflamed nerve is responsible is impaired, and tendon reflexes are impaired.
Degenerative disorders of the spine develop over a long period of time. First, the vessels that nourish the cartilaginous lining of the vertebrae become empty, for this reason there is a lack of nutrients and a disruption of metabolic processes. The disc becomes denser, thinner, and its outer shell (annulus fibrosus) protrudes. Cracks may appear on its surface, then the nucleus pulposus protrudes through them, causing rupture of the outer shell. This is how a hernia is formed. Then an autoimmune process is launched, in which the immune system mistakenly begins to destroy its own tissues. Due to age-related changes, ossification of cartilage tissue occurs and osteophytes form on the vertebrae.
Radicular syndrome develops when nerve bundles are pinched by protrusions, hernias, osteophytes, or displaced vertebrae. Pathology develops with inflammation of the nerve root, damage to the myelin sheath of the nerve, and a decrease in its blood supply.
Reference. Symptoms of osteochondrosis are observed in 50% of people aged 35–40 years. And by the age of 70, degenerative processes are detected in 95% of patients.
Radicular osteochondrosis can be caused by the following factors:
- Excessive load on the spinal column due to excess weight, pregnancy, frequent wearing of high-heeled shoes, heavy physical work, and playing strength sports.
- Curvature of the spinal column (scoliosis, kyphosis), drooping arches of the feet, deformation of the legs.
- Regular static loads during sedentary work.
- Frequent hypothermia of the back, infections.
- Spinal injuries.
- Poor nutrition, lack of nutrients in the diet, excess salt intake, etc.
- Systemic diseases, etc.
Radicular syndrome can be provoked by various factors that act individually or in combination.
No ads 1
Characteristic features of the pathology
Radicular osteochondrosis is the final stage of a long-term destructive and degenerative process occurring in the intervertebral discs. Pain syndrome manifests itself after heavy lifting, a respiratory or intestinal infection, or an awkward sudden movement. The annulus fibrosus of the disc ruptures and it extends beyond its boundaries. In the vacated space, an intervertebral hernia forms, compressing the spinal roots. Radicular syndrome develops - a set of symptoms that significantly complicates a person’s life.
Acute pain occurs not only as a result of trauma to the spinal roots. The situation is aggravated by the resulting bone growths and the extended disc, which infringe on the adjacent soft tissues. This leads to even greater pain, and sometimes to aseptic inflammation. The pathogenesis is also complicated by dyscalgia - pain in the area of innervation of the corresponding roots of the spinal nerves.
General symptoms
Symptoms of radicular osteochondrosis are varied, they depend on which part of the spine is damaged. But doctors have identified the main ones, which indicate pathology:
- The main symptom of the disease is intense pain (constant or paroxysmal), which radiates from the damaged nerve branch to the area for which it is responsible.
- Loss of sensitivity in the damaged area and along the nerve path. The doctor can identify this symptom during a visual examination. To do this, he makes light injections in the area for which the nerve is responsible. If the sensations are more pronounced on the other side, then this indicates radicular syndrome.
- Restricted mobility due to thinning of the muscles served by the affected nerve bundle.
If such symptoms appear, treatment should be started immediately.
[node:field_similarlink]
Symptoms of radicular syndrome in cervical osteochondrosis
Radicular osteochondrosis (RO) of the cervical spine is rarely diagnosed. This is due to the fact that there are strong ligaments in this area, and the diameter of the intervertebral foramina is small, so hernias rarely come out of them.
Radicular osteochondrosis of the neck is manifested by pain, numbness of the neck and upper body
KO of the cervical segment often develops when the artery that supplies nutrients and oxygen to the nerve bundles is compressed.
Painful sensations quickly appear and intensify when turning, tilting the head or torso.
Clinical manifestations of cervical osteochondrosis with radicular syndrome (RS) depend on which vertebra is damaged:
- C1 – cephalgia (pain in the head), impaired sensitivity in the area of the crown and back of the head.
- C2 - the same symptoms as with damage to C1, and there may also be slight sagging of the muscles and skin on the chin.
- C3 – pain, numbness spreads to the affected part of the neck, the tongue becomes numb, speech is impaired.
- C4 – pain and sensory disturbance in the area of the collarbone, scapula, and shoulder. Sometimes the heart and liver hurt.
- C5 – painful sensations, paresthesia spreads from the neck, down the shoulder to the hand. Weakness appears in the shoulder when the patient tries to raise his arm.
- C6 – symptoms radiate from the neck, involving the shoulder blade, shoulder girdle, and thumb. The tone of the biceps decreases, so it is difficult for the patient to move his arm.
- C7 – painful sensations from the neck extend to the shoulder blade, the front and back surfaces of the shoulder, forearm, affecting the index, middle finger, and little finger. Sensitivity in the same area is impaired. The tone of the triceps decreases, so weakness appears when moving the affected limb.
The pain intensifies with tension, sneezing or coughing.
No ads 2
Vertebrogenic cervical radiculopathy - etiology and pathogenesis
The etiology of vertebrogenic cervical radiculopathy includes disc herniation, spinal stenosis, osteophyte formation in the vertebrae, cervical spondylosis and spondyloarthrosis. The immediate cause of the entire complex of pain syndromes in cervical radiculopathy is compression (compression) of the spinal roots, blood vessels, as well as the spinal cord and choroid plexuses. Compression can be caused by a herniated disc, less commonly by protrusion, osteophytes in the vertebrae and facet joints. Spondylolisthesis can cause the same consequences. There are other possible causes of radiculopathy, including spinal injuries, infectious diseases and cancer.
Intervertebral hernias can be medial (middle) - they occur quite rarely and can lead to compression of the spinal cord (myelopathy), but practically do not cause pain. Compression of the spinal roots and intense pain are characteristic of lateral (side) hernias. More often, disc herniations are detected at the level of vertebral motor segments (VMS) C5-C6 and C6-C7, leading to damage to the C6 and C7 roots, respectively.
The most commonly affected cervical root is C7 (60% of cases), less commonly C6 (up to 20% of cases), which is explained by the higher load on the lower joints of the cervical spine.
The direct cause of pain in windbrogenic cervical radiculopathy is two factors: irritation of pain receptors (nociceptors) in the outer layers of the damaged disc and surrounding tissues, and damage to the nerve fibers of the root as a result of compression, inflammation and swelling, and nutritional disturbances in the surrounding tissues.
Radicular syndrome in cervical radiculopathy is often accompanied by the formation of painful trigger points in the muscles of the neck, shoulder girdle, and arms, which can further increase the pain syndrome.
CS for thoracic osteochondrosis
Thoracic osteochondrosis with radicular syndrome is diagnosed more often than CS of the cervical segment. This is due to the structure of this part of the spinal column, where hernias often form.
Making a diagnosis for this type of pathology is not so easy, since painful sensations appear not only in the damaged area of the back, but also in the internal organs. Therefore, patients often confuse osteochondrosis with diseases of the heart, respiratory or digestive organs.
The attack of pain appears sharply, and with immobilization it weakens. When the patient tries to get up again, the pain syndrome resumes.
Radicular thoracic osteochondrosis is often confused with diseases of the heart and respiratory tract
Symptoms of CS for thoracic osteochondrosis also differ, depending on the damaged area:
Symptoms of thoracic osteochondrosis in women
- Th1 – discomfort is localized in the shoulder blades, armpits, and reaches the elbow along the inside of the arm. Sensitivity in the same area is impaired. The throat feels dry and painful.
- Th2 – Th6 – pain appears, numbness of the skin between the shoulder blades, around them, in the armpits, intercostal area to the lower part of the sternum. In addition, weakening muscles may cause the shoulder blade to droop. The patient feels discomfort in the pharynx, esophagus, which sometimes reaches the stomach. There may be a sensation of a foreign body in the upper parts of the digestive canal.
- Th7 – Th8 – sensitivity disorder, pain syndrome spreads from the angle of the shoulder blades and slightly lower on the back of the back, passes along the lower edge of the ribs, closing in the epigastric region (epigastric region). The muscles tense in this same area. Painful sensations appear in the stomach, behind the sternum and in the heart.
- Th9 – Th10 – pain passes in front of the navel, along the lower edge of the ribs, ending on the back at the same level. In the same area, the skin becomes numb and the muscles tense. The patient may have stomach or intestinal pain.
- Th11 – Th12 – pain syndrome spreads from the navel, reaches the groin area and closes at the level of the thoracic vertebrae. Numbness spreads along the same trajectory, and muscle tone in the lower abdomen increases. Patients complain of pain in the stomach and intestines.
Painful sensations with radicular thoracic osteochondrosis become more pronounced when the patient tries to breathe deeply, coughs, sneezes or sharply moves the body. With this type of pathology, the horizontal position of the body does not help relieve pain, since the load on the vertebrae increases.
Reference. Some patients develop cervicothoracic osteochondrosis with radicular syndrome, which is accompanied by symptoms of both diseases. Patients often confuse this disease with pathologies of the heart or respiratory organs. This is one of the most dangerous types of the disease, since diagnosis becomes more complicated and 2 segments of the spine are affected at once.
Manifestations of radicular syndrome in lumbar osteochondrosis
Osteochondrosis of the lumbar region with CS occurs most often. This is due to the fact that the load on the vertebrae of this segment is high, and the diameter of the intervertebral foramina is large. The situation is aggravated if the patient has an underdeveloped muscle corset.
Lumbar osteochondrosis with radicular syndrome occurs most often
Aching or sharp pain in the lumbar region occurs on one side and is quite strong. The nature of the pain syndrome depends on the degree of damage to the nerve bundle, the level of the pain threshold and external factors (concomitant diseases, wearing a special corset, etc.).
Reference. Lower back pain will be relieved if the patient turns over onto his healthy side.
Lumbar osteochondrosis with CS is accompanied by the following symptoms:
- L1 – L3 – pain, numbness in the lower back, anterior thigh, lower abdomen and groin area.
- L4 – pain radiates from the lower back to the front and outer surface of the thigh, knee, reaching the lower leg. Weakness is felt when bending/extending the knee. The likelihood of a decrease in thigh muscle mass on the affected limb increases, this is due to the fact that the quadriceps muscle atrophies. It is difficult for the patient to lean on the affected limb.
- L5 – pain and numbness are present on the outer thigh, lower leg, inner surface of the foot, big toe. The muscles of the foot become weak, then it is difficult for the patient to stand on the affected leg.
With radicular lumbar osteochondrosis, the patient tries to take a position in which the pain is relieved. This usually requires bending your legs slightly. When raising a straight leg in a horizontal position, the pain intensifies (Lasegue's symptom). When the affected limb is bent at the knee from a prone position, the pain syndrome becomes more pronounced (Wassermann's symptom).
Lumbosacral osteochondrosis with CS is manifested by pain in the groin, external genitalia, and lower abdomen. When the cauda equina is damaged (a bundle of roots from the 4 lower lumbar, 5 sacral nerves, with the terminal filament of the spinal cord), the likelihood of involuntary urination, defecation, and sexual disorders in men increases.
No ads 3
Diagnostic measures
If signs of radicular osteochondrosis appear, you should urgently contact a neurologist. During diagnosis, the specialist determines the stage of the pathology and tries to distinguish radicular osteochondrosis from other pathologies (oncology, diseases of the gastrointestinal tract, kidneys, heart).
The study begins with a patient interview and visual examination. During the survey, the doctor tries to determine the nature of the pain syndrome and provoking factors. Then he identifies pain sensitivity, checks tendon reflexes, and evaluates muscle tone. During a visual examination, the specialist pays attention to the patient’s posture, the configuration of the spine, and his gait.
In some cases, you may need to consult with specialized specialists: gastroenterologist, cardiologist, oncologist, therapist, gynecologist, urologist.
To clarify the diagnosis, radiography is performed. This study allows you to identify symptoms of osteochondrosis, curvature of the spine, displacement of the vertebrae, deposition of calcium salts, and signs of a hernia.
If necessary, an MRI or CT scan is prescribed. These are highly informative studies that help determine the location of protrusions or hernias, swelling of nerve bundles.
Reference. Magnetic resonance or computed tomography is required before surgery.
If necessary, the doctor may prescribe ultrasound, myelography, and laboratory tests to clarify the diagnosis.
Treatment methods
In the acute stage of the disease, treatment is aimed at relieving pain and restoring motor activity. When the pain disappears, complex therapy is carried out to help prevent relapses. At this stage, doctors decide whether surgical intervention is necessary.
Important. In the acute period of radicular osteochondrosis, it is recommended to remain in bed for 1 to 3 days. The patient should rest on a hard, level surface. If the pain has disappeared earlier, the patient can allow himself light physical activity in the form of walking.
On the first day after the onset of pain, it is recommended to use applications with cooling ointments. On the second day, you can rub gels and ointments with a warming, analgesic, anti-inflammatory effect, for example, Fastumgel, Finalgon, into the diseased area.
Treatment of osteochondrosis with radicular syndrome is carried out using the following medications:
- Analgesics (Analgin, Ketoral) will help relieve pain. For this purpose, different forms of drugs are used: capsules, injection solutions. To get rid of severe pain, therapeutic blockades with Novocaine, Lidocaine, and in advanced cases - narcotic analgesics are used.
- NSAIDs have analgesic and anti-inflammatory effects. The most commonly used are Diclofenac, Nimesulide, Meloxicam, Indomethacin, Ibuprofen, Celocoxib.
- Muscle relaxants relax spasmodic muscles, improve blood circulation, and relieve pain. These include Clonazepam, Diazepam, Miolastane.
- Psychotropic medications reduce psychoemotional stress caused by debilitating pain. Patients are prescribed Amitriptyline, Desipramine.
- Chondroprotectors inhibit the process of destruction of the intervertebral disc and accelerate its recovery. The most popular drugs from this group include Artra, Dona, Structum, Teraflex, Chondroxide.
- Preparations based on B vitamins help restore nerve fibers. For radicular osteochondrosis, Milgamma, Neurobion, Neuromultivit are used.
Before using any medications, consult your doctor.
Surgical intervention is used in the following cases:
- Presence of intervertebral hernia.
- Damage to the cauda equina, the appearance of neurological disorders of the pelvic organs.
- Severe pain that is not relieved by medication for a long time.
- Numbness or paralysis of the limbs.
Surgical intervention is performed to correct spinal deformities that arose as a result of the CS.
Osteochondrosis with CS at the remission stage should be treated with exercise therapy. A set of exercises is compiled by a doctor or instructor for each patient individually, taking into account the severity of the pathology, the location of the lesion and the general state of health. Therapeutic gymnastics will help strengthen muscles and ligaments, make them more elastic, and increase the flexibility of the spine.
Massage for radicular osteochondrosis relieves pain, increases blood circulation and trophism of damaged tissues, normalizes muscle tone
Massage can be performed during exacerbation and during remission. After a course of procedures, local blood circulation and nutrition of the affected tissues improve, muscle tone is normalized, and pain is reduced.
Manual therapy allows you to get rid of pain, make the spinal column more flexible, reduce disc herniation, and restore the position of displaced vertebrae. This type of therapy is used only outside the acute stage. It is important to find an experienced chiropractor as there is a risk of further damage to the nerves and other tissues that surround the spine.
Physiotherapeutic procedures will help increase the effectiveness of treatment. Patients are prescribed diadynamic therapy, electrophoresis using Novocaine, phonophoresis, etc. Acupuncture helps reduce the intensity of pain and has virtually no contraindications.
Reference. Warm baths are useful for radicular osteochondrosis. In addition, the patient is recommended to wear orthopedic devices that will remove some of the load from the spine.
The patient should supplement the diet with foods rich in vitamins and chondroitins. To do this, it is recommended to consume more fresh vegetables, fruits, dairy products, lean meat, and fish. The patient should eat jellied meat, jelly, and jellied dishes more often.
When treating radicular osteochondrosis, it is worth limiting the amount of salt, marinades, smoked foods, fatty, fried foods, and foods containing large amounts of refined carbohydrates. You should also give up coffee, strong tea, and alcoholic beverages.
If you are overweight, you need to gradually reduce the number of calories in your daily diet.
Attention. For osteochondrosis with CS at the stage of remission, it is recommended to consume at least 2 liters of water per day. In the acute period, you need to reduce the amount of fluid to reduce the swelling that compresses the nerve bundle.
Nutrition
A balanced diet is part of complex therapy for radicular osteochondrosis, without which it is difficult to achieve recovery. Especially if you are overweight, the diet should be low in calories, rich in vitamins and fiber. Exclude fatty, salty, spicy, smoked, flour, sweet, alcohol, coffee - containing products. Enrich food with vitamins and minerals.
Nutrition must be correct and balanced
The most important
Osteochondrosis with radicular syndrome is a consequence of long-term degenerative-dystrophic processes in the spine. This pathology is manifested by pain, numbness in the area that serves the damaged nerve, and limited mobility. When different segments of the spinal column are affected, the symptoms differ. If signs of the disease appear, you should visit a neurologist. It is important to carry out comprehensive treatment: medications, exercise therapy, physiotherapy, massage, etc. In the presence of intervertebral hernias, long-term pain that is not relieved by medications, and spinal deformities, surgery is prescribed. To avoid radicular osteochondrosis, you need to control your weight, eat right, include moderate physical activity, and wear comfortable shoes.
Diagnostics
Osteochondrosis of the lumbar spine with radicular syndrome is important to diagnose and differentiate from other pathologies in a timely manner. This is the first and important step on the path to recovery. At the first signs of the disease, you should immediately contact a neurologist who will conduct an examination, taking into account the complaints presented.
Very often, with osteochondrosis, the nature of the pain is very similar to the manifestations of such pathologies as: hepatic and renal colic, heart attacks, diseases of the gastrointestinal tract. Therefore, it is important to conduct a comprehensive examination, which includes:
- consultation with specialists of various profiles (neurologist, cardiologist, therapist, surgeon);
- instrumental methods (X-ray, MRI, CT scan of the spine);
- laboratory diagnostic methods (detailed clinical blood tests).
MRI is one of the methods for diagnosing pathology.
At the first examination by a neurologist, the patient is identified with a source of pain, risk factors, intensity and nature of pain, the presence of tendon reflexes, the degree of limitation of mobility, and the presence of special specific signs.
An X-ray image can reveal signs of osteochondrosis - displacement of the vertebrae, the presence of intervertebral hernias, bone growths. X-rays help differentiate pain caused by tumors or injuries from pain associated with osteochondrosis.
The most informative in this case will be computer and magnetic resonance imaging. With their help, it is possible to examine all layers of the spine, determine the position of a hernia, if present, as well as swelling of the nerve roots of the spinal cord.
If the above methods are not enough to make a diagnosis, the specialist will use additional methods such as:
- ultrasound diagnostics;
- general blood and urine tests, biochemical blood parameters;
- myelography.
An accurate diagnosis is necessary to begin effective treatment.