Tendinitis (ICD10 code No. M70-M79) is a disease in which an inflammatory-degenerative process develops in the tendons. A pathological process can develop in the muscle tendons that provide movement in the knee, hip, shoulder, and elbow joints. There is tendonitis in the wrists and feet. Rheumatologists at the Yusupov Hospital diagnose the disease using the latest equipment from leading global manufacturers.
Which doctor treats tendinitis? At the Yusupov Hospital, tendonitis is treated by a rheumatologist. With the development of degenerative changes in the tendon, the need for surgical intervention arises. The operations are performed by orthopedic traumatologists. Rehabilitators implement a rehabilitation treatment program. Psychologists help the patient cope with the problem, avoid depression and quickly return to normal life.
In most cases, treatment for tendinitis is performed on an outpatient basis. Patients with severe pathological processes undergo inpatient treatment in the therapy clinic. The level of comfort in the rooms meets European standards. Doctors take an individual approach to the choice of medications, physiotherapeutic procedures, type of massage and gymnastic exercises.
Severe cases of tendinitis are discussed at a meeting of the Expert Council with the participation of doctors and candidates of medical sciences, doctors of the highest category. Leading specialists in the field of rheumatology and orthopedics collectively determine patient management tactics. If conservative therapy is ineffective, the patient is offered surgical treatment. Orthopedists are fluent in the tactics of modern surgical interventions on tendons.
Knee tendonitis
Tendinitis of the tendons of the knee joint (ICD code 10 No. M76) is a consequence of an injury. Post-traumatic tendonitis develops in athletes, older people and people involved in heavy physical labor. The provoking factors of knee tendinitis are constant jumping on hard surfaces, an ill-conceived training regimen, prolonged use of antibiotics, wearing uncomfortable shoes, injuries to the knee joint, flat feet, valgus position of the feet, poor posture and pathological changes in the spine. The cause of secondary tendinitis can be rheumatic diseases, metabolic disorders, or previous infectious diseases. Over time, tendons can undergo degenerative changes and develop tendinitis ossificans.
The following symptoms are characteristic of tendinitis of the tendons of the muscles that provide movement in the knee joint:
- During active movements that are performed with the participation of the affected tendon, while similar passive movements are painless;
- Pain on palpation along the affected tendon;
- Redness, increased body temperature over the tendon area;
- Crepitus (crunching) when performing movements in the knee joint.
Doctors at the Yusupov Hospital make a diagnosis of tendinitis based on the patient’s complaints, life and illness history, characteristic clinical manifestations of the disease and instrumental research data. Changes in blood and urine tests are detected only with secondary symptomatic tendonitis. In patients suffering from rheumatic diseases, anti-citrullinated antibodies and rheumatoid factor are detected in the blood. Metabolic disorders increase the level of creatinine and uric acid. Ultrasound examination and magnetic resonance imaging make it possible to determine the localization of the pathological process. Changes on the x-ray will be present in the case of bone pathology.
Shoulder tendonitis
Inflammatory-dystrophic diseases of the shoulder joint are based on neurodystrophic reflex disorders, which are closely related to cervical osteochondrosis. Tendinitis of the shoulder joint (ICD code 10 - M75) develops under the influence of direct or indirect trauma to the arm, shoulder against the background of osteochondrosis of the cervical and upper thoracic spine. The disease develops in the presence of the following factors:
- Occupational hazards;
- Microtrauma of the tendons of the muscles of the shoulder girdle, which are associated with monotonous and frequently repeated movements of the arm;
- Excessive loads on the upper limb;
- Hand inactivity for a long time.
Tendinitis of the supraspinatus muscle is based on microcirculatory disorders with the subsequent development of a focus of tendon necrosis. This causes reactive inflammation and swelling of the tendon segment near the location of the lesion. Due to the thickened segment of the affected tendon, it is difficult to move the arm to the side and upward. The patient experiences pain, most pronounced in the lateral part of the shoulder below the edge of the acromion process. The intensity of the pain increases at night. Sometimes pain does not interfere with daily activities, but it limits self-care.
Using palpation, the doctor determines pain in the anterior outer area of the shoulder under the edge of the acromion process of the scapula. The pain intensifies when the shoulder is moved to the side. For supraspinatus tendonitis, doctors identify a positive Dowborn's sign. It manifests itself as maximum pain under the edge of the acromion process on the outside of the left shoulder at the 15 o'clock level and the right one at the 9 o'clock level during active abduction of the arms to the sides and raising them upward. The pain disappears or weakens with further upward movement of the arm. When you lower your arm, severe pain appears again. It can cause a real arm block. Active movements of the affected upper limb become impossible.
Coracobrachialis tendinitis is characterized by anterior tenderness at the level of the coracoid process of the scapula. The arm is slightly abducted, extension is limited. When performing passive rotational movements, the patient does not feel pain. Pain appears during active movements of the affected upper limb.
A sign of tendovaginitis of the long head of the biceps muscle is Ergason's symptom: passive rotational movement of the forearm, bent at the elbow joint at an angle of 90°, outward, with resistance from the patient, causes pain in the front of the shoulder along the projection of the tendon of the long head of the biceps muscle. With tendonitis of the infraspinatus and teres minor muscles, pain occurs with external rotation of the shoulder. In order to determine the exact cause of shoulder pain, rheumatologists prescribe radiography of the shoulder joint, ultrasound and magnetic resonance imaging to the patient. With the help of clinical and biochemical studies, the inflammatory and autoimmune nature of tendonitis is excluded.
Tendinitis: Causes
Excessive physical activity and microtrauma. During the work of our muscles, the places where they are attached to the bone skeleton experience a lot of stress. If this load is very high, then the tendons and cartilage tissue at the points of attachment undergo degenerative changes: ruptures, microcracks, changes in shape, due to the deposition of calcium salts at the site of rupture, tissue necrosis (necrosis). In turn, hard deposits of calcium salts in the form of spines or osteophytes can further injure surrounding tissues. Some diseases of rheumatic origin: rheumatoid arthritis, gout, reactive arthritis. In these cases, tendonitis is often accompanied by tendovaginitis. Sports injuries Monotonous and frequently repeated joint movements. For example, wrist tendinitis can be caused by prolonged work at the computer, namely by constant and prolonged pressing of the computer mouse keys.
Tendonitis symptoms:
- Pain with movement, which intensifies if the affected area is involved in the process of movement. With passive movement (palpation), pain may be absent.
- A sensation that resembles rubbing or crunching of a tendon (clearly audible through a phonendoscope.
- Swelling and swelling of the affected area, sometimes combined with hypermia or redness.
- Feeling of weakness in the affected area due to pain.
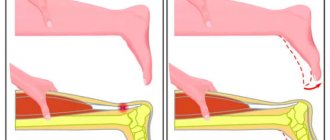
If symptoms persist or worsen, the tendon may even tear (split) and the ends may be felt at the tendon line. Movement in this area will become even more difficult.
Diagnosis of tendinitis
Tendinitis, epicondylitis, or tenosynovitis (inflammation of the sheath surrounding the tendon) can be diagnosed by your doctor at your appointment. During the examination, the doctor may ask:
- Where is the pain located and how severe is it?
- Have you ever had any injuries while working or training?
- The doctor may ask you to perform certain movements and palpate certain areas of the body.
For a correct diagnosis, instrumental examination methods such as MRI and ultrasound . These methods allow you to accurately determine which tendon is torn, whether there are calcium deposits in the affected areas, their size and the possibility of damage to adjacent tissues.
Tendinitis - treatment
Conservative treatment of these diseases is a combination of rest and restoration of the affected area. At the first stage of treatment, it is necessary to relieve or reduce pain. With proper treatment, pain should decrease over a 3-week period. But for the tendon to fully heal, it takes longer - at least 6 weeks for the new scar tissue to completely restore the affected area. Scar tissue will continue to form in the affected area after the 6-week period. In some severe cases, scar tissue can form within 1 year after the start of treatment.
Information about Clinic Discounts and Promotions Here!!!
Tendonitis, epicondylitis, tendovaginitis - these diseases are successfully treated with conservative methods of physiotherapy. In our clinic, to treat these diseases, we successfully use the method of shock wave therapy in combination with magnetotherapy, laser therapy (ILBI), and ultrasound therapy. Operative (surgical) treatment is used when various conservative treatment methods have failed or when there are signs of stenosing tendinitis.
In many cases, the shock wave therapy method can be used as a mono-factor for successful treatment without the use of other factors of physiotherapy.
Shock wave therapy shows high effectiveness in treating various orthopedic disorders, including tendinitis. It is thanks to the unique properties of the shock wave therapy method for the regeneration of new tissues, vessels (capillaries), and the extremely high increase in metabolic processes in the affected area that can significantly accelerate the process of scar tissue formation and reduce treatment time.
In most cases, successful treatment requires no more than 6-7 sessions of shock wave therapy.
The key to successful treatment of these conditions is patience; with proper therapy, it takes some time without significant stress for the tendon to recover.
Elbow tendonitis
Inflammation of the elbow tendon is called tendonitis. In ICD 10, the disease is assigned code M70.9 (soft tissue diseases associated with stress, overload and pressure). Tendinitis of the lateral tendon of the elbow is often called “tennis elbow,” and tendinitis of the tendons located on the inner surface of the elbow is often called “golfer’s elbow.” At the initial stage, symptoms are mild or absent altogether. A person feels slight discomfort in the hand, which is attributed to overload or fatigue.
As the inflammatory process intensifies, the intensity of clinical manifestations also increases. The pain is usually clearly localized and does not radiate to the forearm or wrist. Painful sensations first occur when flexing, extending the joint, or turning the hand outward or inward. The intensity of the pain syndrome with strong tension in the skeletal muscles, since their contraction leads to tension in the tendon. In the absence of medical intervention, the patient begins to feel pain at rest. It becomes aching and constant, preventing you from sleeping peacefully and doing your daily work efficiently.
There is a restriction of movements in the elbow joint, swelling of the periarticular tissues. Pathological exudate interferes with the smooth sliding of the tendon. A person deliberately spares his hand, since flexion, extension, and rotation cause him severe pain.
Sometimes, when palpating an inflamed tendon, a rheumatologist discovers characteristic nodules. Their formation indicates the traumatic nature of tendinitis. Fibrous tissues grow and become denser over time. Their dimensions can exceed several millimeters. When you press on the nodules, they move slightly due to the tension of the muscle fibers. The seals are elastic, elastic, but can harden during the crystallization of calcium salts. Sometimes fibrous nodes sometimes resolve, but only if there are no calcium deposits in them.
When listening with a stethoscope, you can hear the specific sounds that a swollen, inflamed tendon makes during movement. They are almost indistinguishable at the initial stage of the disease. The noise is more accentuated when fibrous nodes form.
The inflammatory process from the tendon quickly spreads to the subcutaneous tissue and epidermis. Due to the rush of blood to the surface of the skin, it appears reddened. This is clearly visible when comparing diseased and healthy elbow joints.
Ultrasound diagnostics is the most informative for traumatic tendonitis, as it allows you to detect fiber ruptures. X-rays allow you to assess the condition of bone and cartilage tissues. Magnetic resonance imaging helps to determine the degree of damage to tendon tissue, the number and location of fibrous nodules, and calcifications.
Additional facts
Tendinitis is a disease of the tendon. Accompanied by inflammation, and subsequently by degeneration of part of the tendon fibers and adjacent tissues. Tendonitis can be acute or subacute, but is more often chronic. Typically, tendonitis affects the tendons located near the elbow, shoulder, knee and hip joints. The tendons in the ankle and wrist joints may also be affected. .
Tendinitis can develop in a person of any gender and age, but is usually observed in athletes and people with monotonous physical labor. The cause of tendinitis is too high loads on the tendon, leading to microtrauma. As you age, your likelihood of developing tendonitis increases due to weakening of ligaments. In this case, calcium salts are often deposited at the site of inflammation, that is, calcific tendinitis develops.
Lateral tendonitis.
Lateral epicondylitis, also known as lateral tendonitis or tennis elbow, is an inflammation of the tendons that attach to the extensor muscles of the wrist: the extensor carpi brevis and longus muscles, as well as the brachioradialis muscle. Less commonly, lateral tendonitis affects the tendons of other muscles: the extensor carpi ulnaris, extensor radialis longus, and extensor digitorum communis.
Lateral tendonitis is one of the most common diseases of the elbow joint in traumatology, occurring in athletes. This form of tendonitis affects about 45% of professionals and about 20% of amateurs, who play on average once a week. The likelihood of developing tendinitis increases after age 40.
A patient with tendonitis complains of pain along the outer surface of the elbow joint, often radiating to the outer part of the forearm and shoulder. Gradually increasing weakness of the hand is noted. Over time, a patient with tendonitis begins to experience difficulties even with simple everyday movements: shaking hands, twisting clothes, lifting a cup.
Palpation reveals a clearly localized painful area on the outer surface of the elbow and above the lateral part of the epicondyle. The pain intensifies when trying to straighten the bent middle finger against resistance.
X-rays for tendonitis are not informative, since the changes affect soft tissue structures rather than bones. To clarify the location and nature of tendinitis, magnetic resonance imaging is performed.
Treatment for tendinitis depends on the severity of the disease. In case of mild pain, you should avoid putting stress on your elbow. After the complete disappearance of pain, it is recommended to resume the exercise, initially in the most gentle mode. In the absence of unpleasant symptoms, the load is subsequently increased very smoothly and gradually.
For tendinitis with severe pain, short-term immobilization using a light plastic or plaster splint, local non-steroidal anti-inflammatory drugs (ointments and gels), reflexology, physiotherapy (phonophoresis with hydrocortisone, electrophoresis with novocaine solution), and subsequently therapeutic exercises are indicated.
For tendonitis accompanied by persistent pain and the absence of effect from conservative therapy, blockades with glucocorticosteroid drugs are recommended.
The indication for surgical treatment of tendonitis is the ineffectiveness of conservative therapy for one year with reliable exclusion of other possible causes of pain.
There are 4 methods of surgical treatment of lateral tendonitis: Heumann's laxative operation (partial cutting of the extensor tendons in the area of attachment), excision of the altered tendon tissue with its subsequent fixation to the lateral epicondyle, intra-articular removal of the annular ligament and synovial bursa, as well as tendon lengthening.
In the postoperative period, short-term immobilization is recommended. Then therapeutic exercises are prescribed to restore range of motion in the elbow joint and strengthen the muscles.
Medial tendonitis.
Medial epicondylitis, also known as pronator and flexor tendonitis, or golfer's elbow, develops when the tendons of the palmaris longus, flexor carpi ulnaris, flexor carpi radialis, and pronator teres tendons become inflamed. Medial tendonitis is detected 7-10 times less often than lateral tendinitis.
This disease develops in those who are engaged in light but monotonous physical labor, during which they have to perform repeated rotational movements of the hand. In addition to golfers, medial tendonitis often affects assembly workers, typists and seamstresses. Among athletes, tedninitis is also common in those who play baseball, gymnastics, tennis and table tennis.
The symptoms are similar to lateral tendonitis, but the painful area is on the inside of the elbow joint. When bending the hand and pressing on the area of injury, pain occurs above the inner part of the epicondyle. To confirm tendinitis and assess the nature of the process, magnetic resonance imaging is performed.
Achilles tendonitis
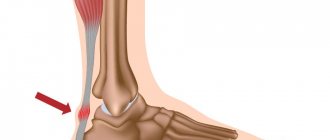
Achilles tendonitis (ICD 10 code in adults – M76.6) develops for the following reasons:
- Excessive load on the Achilles tendon (overstrain of the calf muscle, frequent running uphill or downhill, a sharp increase in the amount of physical activity);
- Using uncomfortable running shoes;
- Frequently wearing high-heeled shoes and changing heels to flat soles every night.
The patient experiences pain along the Achilles tendon, usually closer to the heel. Swelling and local redness of the skin appear in the tendon area. The pain intensifies when standing on your toes and jumping on your toes. Pain may occur within the first few minutes of walking in the morning. Mobility of the ankle joint is limited.
Tendinitis of the patellar tendon and thigh muscles
Chronic patellar tendinitis is known as “jumper's knee.” The quadriceps muscles are subject to excessive stress during many sports. Microtraumas systematically occur in them. Tendinitis develops more often in athletes who take anabolic steroids.
At the initial stage of the disease, touching the tendon causes pain. With more serious injuries, swelling of the tendon may occur. Over time, a degenerative process develops and the tendon may rupture. In the patellar ligament, degeneration occurs at the inferior pole of the patella or below, at the site of attachment to the tibial tuberosity.
At the onset of the disease, the patient feels pain only after physical activity. It is gradually felt during exercise, and over time does not leave the person even during rest. During the examination, rheumatologists determine the location of the pain by asking the patient to straighten the leg at the knee and applying pressure to the affected tendon. The diagnosis is confirmed using ultrasound. X-rays and magnetic resonance imaging can help identify calcifications within the tendon.
Quadriceps tendonitis occurs for the same reason as inflammation of the patellar tendon. The disease is rarely detected in young athletes. Due to the development of degenerative processes in older patients, rupture of the quadriceps tendon may occur due to tendonitis.
Description
Tendinitis. An inflammatory disease in the tendon area. It can be either acute or chronic. With chronic tendonitis, degenerative processes develop in the area of the affected tendon over time. As a rule, the part of the tendon adjacent to the bone is affected; less often, the inflammation spreads throughout the tendon. The main cause of tendinitis is a single or regular increased load, leading to microtrauma of the tendon fibers. The disease often occurs in athletes and people who work physically (especially if this work involves monotonous movements). Tendinitis is accompanied by pain during movement, slight swelling, hyperemia and local fever. Treatment can be either conservative or surgical. Prevention of exacerbations is of great importance in chronic tendinitis.
Treatment of tendinitis
At an early stage of the disease, to relieve the inflammatory process, doctors carry out conservative treatment of tendinitis:
- Peace;
- Cold;
- Non-steroidal anti-inflammatory drugs;
- Injections of glucocorticoids into periarticular tissues;
- Physiotherapeutic procedures (ultrasound, laser or magnetic therapy, UHF, phonophoresis of drugs).
At the Yusupov Hospital, patients suffering from tendinitis receive massage of the affected area. Rehabilitators individually compose a set of gymnastic exercises depending on the location, severity of the pathological process and the phase of the inflammatory process. If, despite complex therapy, treatment is ineffective, the disease progresses, a degenerative process develops in the tendons or stenosing tendinitis develops, patients are offered surgical intervention. After surgery, patients restore impaired functions in a rehabilitation clinic. The rehabilitation therapy program is compiled and implemented by a multidisciplinary team of specialists: rheumatologists, orthopedists, physiotherapists, and rehabilitation specialists.
When the first signs of tendinitis appear, call the Yusupov Hospital at any time of the day, regardless of the day of the week. Contact center specialists will make an appointment for you with a doctor. After an examination and an accurate diagnosis, the doctor will prescribe a comprehensive treatment aimed at relieving pain and inflammation and preventing the degenerative process.