Ankylosing spondylitis is a chronic form of arthritis primarily affecting the spine. It is characterized by pain and stiffness in the lower back, buttocks, thoracic back, neck and sometimes in the hips, feet, and chest. It may also manifest as swelling and limited mobility in other joints. This disease occurs more often in men than in women. To date, there is no way to completely cure this disease. The goal of treatment is to relieve symptoms and stop progression. Most patients retain their ability to work and be physically active. A complication of AS ( Bechterew's disease ) may be inflammation of the iris (iritis) and impaired respiratory function associated with kyphosis and deformation of the chest.
Symptoms
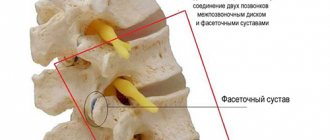
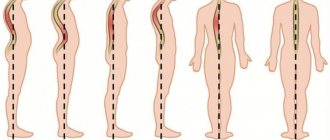
This disease can manifest itself as pain of varying intensity in the lower back and buttocks, especially in the morning. Some patients may have pain in the legs and feet. The pain tends to gradually decrease after some physical activity. AS usually occurs between the ages of 15 and 30 years. The disease, as it progresses, causes inflammation of the ligaments, tendons, and joints of the vertebrae, which leads to limited mobility in the lumbar and cervical spine (up to fusion of the vertebrae). As stiffness develops, the normal physiological curves in the neck and lower back change and kyphosis sharply increases. This leads to a pronounced forward tilt of the body and limitation of motor functions such as walking. Due to the fact that inflammation of the joints in the area of the articulation of the costal arches with the sternum is possible, difficulty breathing may occur. Other joints, eyes, sometimes lungs, heart valves, aorta, and intestines may be involved in the inflammatory process. A prolonged inflammatory process leads to tissue scarring and irreversible changes. In some cases, the disease progresses slowly and does not lead to significant complications; in others, rapid progression leads to disability and persistent symptoms. There is a certain dependence of the degree of progression of AS on the onset of the disease, age and area of localization of the pathological process. With early diagnosis and timely treatment, the likelihood of slow progression of the disease increases.
Risk factors, causes
The greatest predisposition to the development of this pathology is noted among the following categories of people:
- people caught in the epidemic zone;
- those who have chronic diseases of internal organs and systems;
- population living in unfavorable conditions, especially if there are sanitary and hygienic violations;
- children and adolescents;
- patients suffering from endocrine system disorders;
- people who have undergone organ implantation surgery;
- patients undergoing hormonal therapy;
- people who have been diagnosed with a malignant neoplasm.
Consequences
If the necessary therapeutic measures are not applied to the identified disease, the following complications may occur::
The main complication of Pott's disease is disruption of the functioning of the spine; problems with the motor function of the spine;- paralysis of the lower or upper limbs;
- bladder dysfunction;
- pathologies in the functioning of the large intestine;
- problems with reproductive function;
- tuberculous meningitis;
- breakthrough of the abscess and its penetration into the lumen of the spinal canal, leading to epiema (a complication that represents the accumulation of pus in any body cavity or inside organs).
Due to the risk of disease outcome, it is important to start therapy as early as possible to avoid the development of serious complications. If proper treatment of the disease is not carried out or started too late, there is a high risk of death .
Slowly progressive form
Typically, this form of AS is characterized by dull lower back pain and stiffness in the back. Exacerbations of the disease, manifested by increased pain and stiffness, last several weeks.
- Pain and stiffness limiting mobility may appear in the lower back, middle back or neck. The pain intensifies slowly, over several weeks, and does not have a clear localization. Stiffness usually occurs in the morning (sometimes early in the morning at 3-6 am) and disappears within an hour of waking up. Physical activity helps reduce pain and stiffness.
- Some patients report fatigue. This is due to the fact that part of the energy in the body is spent on the inflammatory process.
- Inflammation of the iris. This inflammation (iritis) occurs in 20-30% of patients with AS. It manifests itself as redness, soreness in the eye and increased sensitivity to light.
How do we treat ankylosing spondylitis?
Non-steroidal anti-inflammatory drugs are used as basic therapy for ankylosing spondylitis. To significantly slow down the development of the disease, it is recommended to use them in long courses.
We examine the patient for various infections and, if detected, treat them. This helps prevent exacerbations of the disease.
Hirudotherapy (leech treatment) is also successfully used in the treatment of this disease. The enzymes contained in the saliva of leeches can have a complex effect on the disease: they “soften” and make the spine more flexible, increase immunity and have an anti-inflammatory effect.
Kinesiotherapy, a unique set of exercises for the spine and joints, also helps prevent ankylosis of the spine. This complex was developed by our specialists. It is therapeutic and educational. During individual or group sessions, patients learn to perform exercises on their own so that they can practice at home.
We also use massage, acupuncture, bee therapy and other methods, which can be found here.
Rapidly progressive form of AS
Processes of changes in connective tissue lead to irreversible processes and severe symptoms.
- These processes in the spine lead to fusion of the vertebrae (ankylosis).
- With ankylosis, the pain syndrome gradually decreases. But vertebral fusion increases the risk of fractures, especially in the cervical region.
- Disorders in the spine lead to changes in mobility and balance of the body. With severe kyphosis, it becomes difficult to straighten the torso and keep the back straight. The process of standing and walking is especially disrupted when the hips are involved in the pathological process.
- A pronounced forward tilt of the spine can cause breathing problems due to limited mobility of the chest. In addition, inflammatory changes can affect lung tissue, leading to pulmonary fibrosis and increased susceptibility to infection. The risk of lung infections is higher in smokers.
- Scarring processes in the eyes can lead to poor vision and glaucoma.
- In rare cases, damage to the myocardium and valve apparatus occurs, which leads to impaired contractile function and, as a consequence, to heart failure. Damage to the aorta and its expansion are also possible.
- Sometimes there is a connection between intestinal inflammation and AS. Some patients develop Crohn's disease.
- Possible kidney damage is largely associated with long-term use of medications prescribed for AS.
- In some patients (with pronounced changes in the distal spine) cauda equina syndrome occurs. This syndrome is manifested by impaired sensitivity in the groin area and dysfunction of the pelvic organs.
Ankylosing spondylitis has much in common with a whole class of joint diseases called arthropathy. For example, this is psoriatic arthritis, reactive arthritis (Reiter's syndrome), enteropathic arthritis. But in these diseases, spinal lesions are not as pronounced as in AS.
Diagnosis of ankylosing spondylitis
The first signs of AS are dull pain in the lower back or buttocks (a symptom that occurs in many diseases). What matters is a gradual increase in pain intensity. If AS is suspected, it is necessary to conduct an X-ray examination, genetic study or MRI of the iliosacral joints. Characteristic of AS are changes in the iliosacral joints visible on radiography, but they appear only after several years of the disease. Given the greater resolution of computed tomography and MRI, it is necessary to use these diagnostic methods more widely. Isolation of the HLA-B27 gene also helps in making a diagnosis. Therefore, early diagnosis of AS is a difficult task and often takes time to confirm the diagnosis.
Drug therapy
Treatment of the disease has 2 directions: combating the pathogen and eliminating the clinical manifestations of the pathology. The doctor prescribes the use of antibiotics and NSAIDs.
Tuberculous spondylitis can be cured with etiotropic therapy. The patient is prescribed the use of Rifampicin, Isoniazid and Streptomycin.
Use of antibiotics
These drugs are intended to fight infection. The best medicines are presented in the table.
Table 3. Antibiotic drugs:
| A drug | Description |
| Semi-synthetic antibiotic from the group of third generation cephalosporins. Has a bactericidal effect. |
| The drug treats infectious pathologies. |
| An antibacterial agent with a powerful antimicrobial effect. |
| Fights infectious and inflammatory pathologies caused by microorganisms sensitive to norfloxacin. |
| A broad-spectrum bactericidal drug from the group of fluoroquinolones. |
Use of non-steroidal drugs
The tablet presents the best medicines.
Table 4. Recommended NSAIDs:
| A drug | Description | Daily dosage |
| The drug reduces pain and inhibits inflammatory processes. | The drug is injected into the muscle. The duration of therapy is 8 days. Morning use is recommended. |
| Prescribed for symptomatic therapy. | One-time course - 1.5 weeks. Daily dosage - 1.5 ml. |
| Has anti-inflammatory, antirheumatic, analgesic effect. | The duration of the course is 1.5 weeks. Daily dosage - 16 ml. |
Treatment of tuberculosis
The tablet provides information about etiotropic therapy drugs.
Table 5. Help for tuberculous spondylitis:
| A drug | Description | Daily dosage |
| Prescribed for infectious and inflammatory pathologies. | 450-600 mg. The duration of the course is 4-8 weeks. |
| First line antituberculosis drug. Has a powerful bactericidal effect. | The dosage is prescribed on an individual basis. Course duration is 4-5 months. |
| An antibiotic drug of the aminoglycoside group with a wide spectrum of effects. | The medicine is injected into the muscle. The daily dosage is prescribed individually. The duration of the course is from 12 weeks to six months. |
Note! You cannot increase or decrease the dosage of medications on your own.
Treatment of AS
Treatment for ankylosing spondylitis mainly involves exercise and physical therapy. They help reduce stiffness and increase mobility. It is also possible to prescribe medication to relieve inflammation and reduce pain. With ankylosing spondylitis, there is a high risk of spinal injury, which requires the use of seat belts whenever driving a car. Regular eye examinations are necessary to check for inflammation of the iris. If necessary, you can use a cane to reduce the stress on your joints when walking. Surgical treatment methods are used extremely rarely for this disease (sometimes severely damaged joints are replaced with prostheses - hip and knee). Considering that today there are no pathogenetic treatment methods, the main task is to reduce symptoms and maintain motor activity.
Author: V.I. Dikul