Spondyloarthrosis deformans of the thoracic spine is a chronic degenerative disease that affects the hyaline cartilaginous fibers of the intervertebral joints. Due to the gradual destruction of the cartilaginous synovial membrane, they undergo deformation, and bone osteophytes form on their surface. The thoracic spine may completely lose its ability to move.
Long-term spondyloarthrosis of the thoracic spine disrupts the process of gas exchange in the lung tissue. The structure of the thoracic spine is specific. The vertebral bodies have special notches that form bone articulations with the costal arches. These small joints provide the ability to make breathing movements through the chest. With spondyloarthrosis, not only the facet, facet and uncovertebral intervertebral joints are affected. The costovertebral joints of bones are also subject to the process of destruction and deformation. Therefore, the chest loses its ability to move. The breathing process is ensured only by the movement of the diaphragm, which significantly reduces the vital volume of the lungs.
Oxygen deficiency negatively affects the performance of the brain, heart and other internal organs. It is very important to begin treatment in the early stages of the degenerative dystrophic process. In later stages, treatment can only be carried out surgically.
It is very important to know the first symptoms of spondyloarthrosis of the thoracic spine and begin treatment immediately after detecting the pathology. Current information about the disease is presented on this page. If you suspect its development, we recommend that you immediately consult a doctor. A simple X-ray examination will allow you to identify signs of pathology and begin timely treatment, allowing you to restore chest mobility and vital lung capacity without surgery.
In Moscow, you can make an appointment for a free appointment with a vertebrologist at our manual therapy clinic. Here the patient will be provided with all the information about the possibilities of treatment using manual therapy methods. During the initial free consultation, the doctor will conduct an examination and make a preliminary diagnosis, and give individual recommendations for additional examinations and a course of treatment.
What is spondyloarthrosis?
Spondyloarthrosis is a disease that is characterized by pain in different parts of the spine and causes a constant feeling of discomfort. Like any degenerative chronic disease, spondyloarthrosis is curable if:
- The treatment of spondyloarthrosis should be approached comprehensively.
- The patient himself makes efforts to eliminate the disease and its symptoms.
- Treatment begins at an early stage of spondyloarthrosis.
Each vertebra has two articular processes in the upper and lower parts, through which it is connected to another vertebra. These joints are called facet joints; A disease that affects the facet joint with arthrosis is called spondyloarthrosis.
At the MART clinic on Vasilyevsky Island
- Experienced doctors (including those practicing in the USA and Europe)
- Prices affordable for everyone
- Expert level diagnostics (MRI, ultrasound, tests)
- Daily 8:00 — 22:00
Make an appointment
Sometimes, when characterizing spondyloarthrosis, the terms arthrosis of the intervertebral joints, arthrosis of the facet joints or facet syndrome are used. The objects of destructive processes are all elements of the joint: cartilaginous surfaces, ligaments, subchondral bones, joint capsules and adjacent muscles.
Spondyloarthrosis refers to diseases that appear as a result of degenerative changes in the spine, while spondyloarthrosis itself refers to chronic degenerative diseases of the spine (joints), contributing to the destruction of the musculoskeletal system.
Deformations and shifts add mechanical loads to the elements of inflamed joints - primarily to the cartilaginous surfaces, increasing their size and creating osteophytes (bone growths, spines), erosion, contributing to the accumulation of synovial fluid in the joint capsules. As degenerative processes increase, the cartilage wears out, the number of microtraumas increases, and pain increases due to stretching of the extensively innervated joint capsules. Pain also causes pressure on the periosteum, which is saturated with encapsulated nerve endings.
Diagnosis and treatment of spondyloarthrosis
If symptoms of spondyloarthrosis appear, consult a doctor - he will conduct a competent diagnosis. He will listen to your complaints, take an anamnesis, examine you and conduct several physical tests. Will refer you to the necessary additional studies - for example, x-ray or computed tomography.
Treatment of spondyloarthrosis is usually conservative and complex. It may include a spinal traction procedure, physiotherapeutic procedures, and a physical therapy complex.
Treatment is aimed at reducing and eliminating pain, optimizing the load on the spine and preventing the progression of the disease.
If conservative treatment methods do not help, the doctor refers the patient to surgical treatment - surgery.
Causes of spondyloarthrosis
The causes of spondyloarthrosis cannot be determined unambiguously, since both the etiology (occurrence) and pathogenesis (development) of this disease are complex and insufficiently studied processes. The reasons for the development of spondyloarthrosis have been studied much better; a number of internal and external factors are identified:
- unilateral loads due to professional activities or sports;
- damage and degeneration of intervertebral discs;
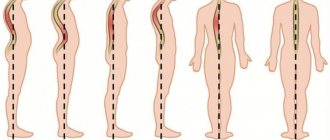
- spinal deformation/instability;
- scoliosis;
- hyperlordosis;
- rheumatism;
- overweight;
- muscle weakness;
- congenital abnormalities of the spine (dysplasia);
- infectious diseases;
- chronic arthritis (rheumatoid arthritis, spondyloarthritis).
Hormonal disorders, especially estrogen deficiency of female sex hormones, contribute to the appearance of spondyloarthrosis.
Therefore, the incidence of the disease is high among people over 60 years of age of both sexes and in women over 55.
Symptoms of spondyloarthrosis
Since spondyloarthrosis affects all parts of the spine, the symptoms correlate with the area of the disease. More often, degenerative changes occur in the lumbar spine. Thus, the pain associated with spondyloarthrosis occurs in the lower back.
Frequent back pain is the most common symptom of spondyloarthrosis. Under load and with movement, the pain intensifies. However, the symptoms and manifestation of discomfort in diseases of spondyloarthrosis are varied. There are no specific clinical signs that clearly indicate facet syndrome. This complicates the diagnosis of spondyloarthrosis and differentiation from other diseases that affect the spine, intervertebral discs, tendons and adjacent muscles.
Spinal osteochondrosis and spondylosis
So, dear readers, we have finally come to consider the condition that modern medicine considers the cause of most spinal problems, with which I categorically disagree and will try to refute the popular opinion. But in order to argue reasonably, I first want to give you a classical idea of \u200b\u200bthe disease.
The view on the problem of osteochondrosis has changed several times over the past two hundred years, depending on certain trends in medical science, or, if you like, medical fashion. Thus, the first known descriptions of destructive processes in intervertebral discs were made in the middle of the 19th century. In 1857, Dr. Virchow described a herniated cervical disc and defined it as a “chondroma,” that is, a tumor. Following him, a number of other authors reported similar “tumors.”
This “fashion” for tumors persisted until the 30s of the 20th century. It was only in 1934 that doctors Piet and Echols recognized the fallacy of this view and proposed the term “disc herniation” . Since then, most spinal problems have been “attributed” to hernias (unfortunately, this practice has not disappeared to this day).
However, ten years later, the development of the doctrine of infections led to the fact that damage to the spine and nerve roots began to be considered as a consequence of sore throat, flu, rheumatism and other infectious diseases. For example, the term “radiculitis ,” meaning inflammation of a nerve root, implied the presence of infection.
Ten years later, a new revolution occurred in the views of scientists, or rather, a turn to the old and spinal diseases again began to be considered as a result of intervertebral hernias .
Since about the 70s of the 20th century, a modern view on the development of spinal osteochondrosis has been formed and established, but, frankly speaking, this is a rather strange view if we consider osteochondrosis as the cause of pain in the spine. After re-reading a lot of classical, traditional medical literature, at some point I suddenly realized that many authors themselves do not really understand (or do not think about it) how osteochondrosis leads to pain in the back.
Here is a typical description of osteochondrosis for most special reference books: “Osteochondrosis occurs when the nucleus pulposus of the intervertebral disc changes. In the initial stage of osteochondrosis, drying of the nucleus and disruption of its function are observed. The disc loses its firmness and elasticity, degeneration of the fibrous ring occurs, fibrous fibers are torn or ruptured; The height of the intervertebral disc is significantly reduced. Subsequently, the nucleus pulposus can break through the weakened fibrous ring with the formation of a disc herniation or push through the vertebra with the formation of a Schmorl hernia.”
So what happens? According to the reference book, osteochondrosis is a shrinkage of the core and a decrease in the height of the intervertebral discs, as well as the formation of an intervertebral hernia, which for some reason is considered as a result of osteochondrosis. But in fact, disc herniation is an independent disease and is in no way connected with osteochondrosis.
Let me remind you that real, clinically manifested hernias are not associated with age-related weakening of the discs and occur very often in young people - even at an age when there is no hint of senile changes in the spine! In addition, in young patients, the manifestations of intervertebral hernia are especially pronounced - precisely because the core of the disc is very strong and elastic (ask any practicing neurosurgeon or vertebroneurologist about this, and they will definitely tell you how much more difficult it is in most cases to treat with therapeutic methods of young patients). And even more so, Schmorl’s hernia can hardly be classified as osteochondrosis, if only for the reason that it occurs only when the disc turns out to be strong enough and “presses through” the bone structure of the vertebra (I wrote about this above).
So, dear readers, let's remember: osteochondrosis is in itself, and a hernia is in itself.
Now let's look at osteochondrosis itself (without a hernia), in which the disc shrinks and loses its elasticity. But what does this change and how does it cause pain? There is no answer to this question in traditional reference books. They again, again and again refer to the hernia, and only to it, as if there were no other disorders: muscle rigidity and hypotonicity, displacement and blocking of intervertebral joints!
By the way, the idea of displacement and blocking of intervertebral joints in general is for most classical authors something like a red rag for a bull, and if we admit that individual muscle disorders are at least somehow ready, then the term “displacement of joints” causes an explosion among medical conservatives indignation: this does not exist and cannot exist, because it can never happen!
However, I will give my own example for my opponents. I am a healthy and physically developed man. I don’t have any significant muscle disorders, I’m still young enough to have serious age-related changes in the discs, and besides, I haven’t had any pain in my life. And then one morning, while reaching for the alarm clock, I made an unsuccessful sudden movement and felt a click in the cervicothoracic junction of the spine. I didn’t experience any pain (muscular compensation was good), but the next day I felt discomfort and tension in the damaged area, and a crunching sound appeared in other parts of the neck when I moved. And two days later, a headache began to arise - from tension, usually in the evening, and the clarity of thinking decreased - also in the evening hours.
Having a fairly good command of manual techniques, I tried to perform the manipulation on myself, but it turned out to be difficult. Then I turned to a friend, with whom we once began to study manual therapy. I explained to him what to do, how to position his hands and in which direction to move them, and we began the procedure. After a short preparation, he made the necessary movement, a click was heard - and my problems were literally removed by hand! The headache disappeared, my head “cleared up”, and the crunching noise when moving no longer occurred.
Now let's think about what kind of illness I had? If I went for a consultation with a regional neurologist, 80 doctors out of 100 would diagnose me with osteochondrosis or a herniated disc and prescribe appropriate treatment. But if it was a hernia, then where and why did it disappear? After all, it is almost impossible to correct a hernia, and even more so it is impossible to do it instantly, without traction, with just a turn of the head.
If I had osteochondrosis, then why did it arise at such a young age, and did not arise gradually, as is typical for it, but immediately, at one moment? And why did this osteochondrosis disappear after one procedure? In my opinion, dear readers, there was no trace of osteochondrosis here, and the only damage that could develop in this way was a displacement (block) of the intervertebral joint.
But let's return to osteochondrosis itself. Still, can it lead to some troubles or not? Of course it can, but very moderately. For example, to limited mobility of the back, which is very natural in old age. In addition, osteochondrosis contributes to the appearance of arthrosis of the intervertebral joints. In general, these two diseases usually go hand in hand. And finally, as osteochondrosis develops, it gradually leads to spondylosis.
Spondylosis deformans, in principle, is simply the next stage of osteochondrosis, or, if you like, the next stage of the disease. With spondylosis, the fibrous fibers of the intervertebral disc are slowly squeezed out under the pressure of the body weight beyond the boundaries of the vertebral bodies and “pull” the edges of the vertebrae fused to them, promoting the formation of bone protrusions, “hooks” - osteophytes. As a result, the disc is limited on the sides and “covered” at the edges by osteophytes.
To some extent, the appearance of osteophytes is a preserving reaction of the body during the “subsidence” and gradual destruction of the cartilage of the intervertebral disc - osteophytes do not allow fibrous fibers to spread further to the sides. And, as a rule, their appearance does not cause any harm to the body.
In connection with the above, situations seem strange when doctors try to “treat” spondylosis or fight osteophytes - this is sometimes the sin of some clinic doctors. As for the numerous charlatans who promise to “dissolve salts and break bone hooks,” they are simply ridiculous in their ignorance.
Spondylosis is a condition that, if it occurs, will never disappear, and the development of osteophytes can only be stopped, slowed down (by improving the condition of the discs), but not stopped altogether. And another question is whether it is necessary to try to stop the development of spondylosis at all, given that both spondylosis and the formation of osteophytes are a kind of reaction of an aging organism that tries to adapt to the changes occurring in it.
Symptoms of osteochondrosis and spondylosis
As you, I hope, have already understood, from my point of view, these two diseases have practically no separate independent symptoms, except for limited mobility of the spine and moderate pain. For the most part, these diseases can be considered in conjunction with arthrosis of the intervertebral joints, and they, in fact, develop together, simultaneously. That is, to put it more clearly, from my point of view, back pain is most often caused not by osteochondrosis and spondylosis. In 95 cases out of a hundred, severe back pain is caused by other causes and diseases, which we have already discussed in this chapter and will be discussed in the next chapter.
Diagnosis of osteochondrosis and spondylosis
To diagnose osteochondrosis and spondylosis, radiography and computed tomography examination are used. On X-rays with osteochondrosis, you can see a decrease in the distance between the vertebrae, and with spondylosis, osteophytes are clearly visible. Computed tomography, in addition, allows you to evaluate the condition of the intervertebral discs themselves.
Treatment of osteochondrosis and spondylosis
Treatment of osteochondrosis and spondylosis should combine the maximum range of effects and solve several problems:
improving the condition of intervertebral disc cartilage; improving blood circulation in the spine and surrounding tissues; pain relief; reducing the pressure of bones on each other and strengthening the bone structures of the spine.
To improve the condition of the intervertebral discs, chondoprotectors are prescribed, which nourish the cartilage of the discs and promote their restoration. Drugs in this group must be taken in courses, 2 times a year, for several years.
It is advisable to combine the intake of chondoprotectors with the simultaneous use of vasodilators, which activate metabolism and blood circulation in the spine, and also allow nutritional “building” substances to better penetrate the cavity of the affected segment of the spine.
Effectively improves blood circulation, naturally, back massage. For osteochondrosis of the spine, it is advisable to do it twice a year, in courses of 8-10 sessions. But the best way to stimulate blood circulation is hirudotherapy (treatment with medicinal leeches). The use of leeches for osteochondrosis is all the more justified because these unique little creatures, during a bite, inject a whole set of enzymes useful for the spine into the human body. It is clear that it is difficult for many to overcome natural disgust and agree to such treatment, but patients who can cope with themselves and decide to undergo a course of hirudotherapy are usually very satisfied with its results.
Among other measures that actually stimulate blood circulation, cryotherapy can be recommended. But when treating the spine, this method should be used very carefully and only under the supervision of an experienced specialist. Other physiotherapeutic procedures also improve blood circulation, but they do this to a much lesser extent, so they are used only for lack of a better one.
To reduce pain in spinal osteochondrosis, non-steroidal anti-inflammatory drugs are traditionally used, forgetting that their long-term use, according to a number of domestic authors, can slow down the restoration of cartilage tissue of damaged intervertebral discs. Therefore, I generally agree with the short-term use of anti-inflammatory drugs for exacerbations, but oppose their long-term use. After all, pain with osteochondrosis is rarely severe, and most often it can be tolerated or reduced in other ways, for example, acupuncture, massage, and electroacupuncture. In addition, in cases of severe pain, novocaine blockade of especially painful areas of the spine is performed.
To reduce the pressure of the bone structures of adjacent vertebrae on each other and increase the distance between the compressed articular surfaces of the articulating vertebrae, traction (spinal traction) is used and auxiliary means such as a cervical collar and lumbar bandage are used. Traction is more effective in treating the cervical spine. When treating the lumbar region, you can use a homemade traction device, which is installed on the patient’s bed - see the section on the treatment of intervertebral hernias.
A good effect in the treatment of osteochondrosis is given, among other things, by the therapeutic gymnastics given in Chapter X of this book. You need to exercise at least 3 times a week for 30-40 minutes.
In conclusion, I would like to note that although spinal osteochondrosis is quite difficult to cure, nevertheless, when carrying out complex measures, it is possible to achieve significant improvement, regardless of the patient’s age. I emphasize this specifically, because often, when coming to an appointment, some elderly patient sighs doomedly: “I, a doctor, as a matter of fact, do not expect good results. I understand that at my age there is no point in hoping for recovery.” In this case, I always have to convince the patient that a person at any age has the opportunity to be quite healthy - all that is needed is desire, willpower, hard work and the recommendations of a good doctor, which must be followed strictly.
To summarize everything that has been said above on the topic of osteochondrosis, I want to conclude: in my opinion, the time has come to take a different look at the essence of metabolic-dystrophic diseases of the spine and make changes in the interpretation of diagnoses. In cases where the doctor is not just concerned about patients, but really wants to help the sick, to determine the necessary treatment he will need a more detailed analysis of the diagnoses and the simplified term “osteochondrosis” alone will not do.
For example, a full diagnosis of some conditions might look like this: “displacement of the C1-C2 intervertebral joint (between the first and second cervical vertebrae) against the background of general muscle hypotonicity.” Or this: “rigidity of the lumbar muscles against the background of Scheuermann’s disease, protrusion of the L5-S1 disc (lumbosacral junction).” Of course, formulating and writing down such a long diagnosis is somewhat more difficult and responsible than condensing it into two words “osteochondrosis of the spine.” But if a doctor really wants to prescribe effective treatment, he in any case must detail the causes of the disease, and in this case a diagnosis of osteochondrosis that does not explain anything will not suit him.
Article by Dr. Evdokimenko© for the book “Back and Neck Pain”, published in 2001. Edited in 2011 All rights reserved.
Signs of spondyloarthrosis
However, there are common signs for spondyloarthrosis:
- muscle tension;
- absence of pain at rest, appearance when starting to move;
- increased inflammation and pain over time.
Depending on the location in one of the three parts of the spine, lumboarthrosis, cervicoarthrosis and dorsarthrosis are distinguished.
Spondyloarthrosis of the lumbosacral spine
The most common type of spondyloarthrosis is lumboarthrosis, or spondyloarthrosis of the lumbosacral spine. Typical for him are:
- chronic dull or aching pain in the lumbar region;
- increased pain when bending, tilting the spine, especially backwards;
- pain in the lower back (lumbago);
- restriction of movement in the lumbar spine;
- feelings of stiffness, stiffness in the lumbar region.
Spondyloarthrosis of the cervical spine
Cervicoarthrosis is a spondyloarthrosis that affects the facet joints of the cervical spine. Manifests itself due to osteochondral deformations:
- pain in the neck, often radiating to the shoulder-scapula region or to the back of the head;
- pinching and irritation of nerve roots;
- irritation of the vertebral artery.
Spondyloarthrosis of the thoracic spine
Dorsarthrosis or thoracic spondyloarthrosis is less common, at least neurological disorders associated with degenerative lesions of the joints in this area are quite rare due to the anatomical features of the thoracic region.
If you have any questions, ask our specialist! Ask a Question
Dorsarthrosis
Spondyloarthrosis in the thoracic spine is called dorsartosis. Its symptoms include the following:
- pain localized in the thoracic spine, which initially occurs periodically, but as the disease develops, it becomes permanent;
- a feeling of discomfort and the appearance of aching pain with an increased level of humidity;
- feeling of stiffness in the morning;
- atrophy of the spinal muscles;
- the appearance of a crunch when making sudden movements.