This chronic disease associated with destruction of articular cartilage is considered to be a disease of older people, but the percentage of children suffering from arthrosis of the foot is extremely high. Foot disease is diagnosed in children aged from one to four to five years. Cartilage depletion occurs and, as a result, the space between the joints decreases. This process is accompanied by pain and stiffness in movements, so if your child complains of pain in the legs, do not delay in finding out the cause of poor health.
Symptoms
The increase in symptoms occurs gradually:
- A feeling of heaviness, aching in nature after prolonged physical activity. Damage to the joints of the lower extremities may be accompanied by periodic lameness.
- The intensity of the pain increases even after light exertion, mobility is limited, and swelling appears.
- The pain is constant, mobility is severely limited, and organ deformation is noted.
The first stage is characterized by the beginning destruction of cartilage, gradual loss of elasticity and the formation of roughness on its surface. As a result, the patient experiences pain and stiffness at the beginning of movement, which then quickly disappears.
As the cartilage deteriorates, the stress on the surfaces of the joints increases. When cartilage tissue is destroyed, aggressive substances are produced that cause irritation of the synovial membrane and its inflammation.
The formation of effusion in the joint cavity is accompanied by its swelling and increase in size. Touching causes pain, the temperature rises, and redness of the skin occurs.
The second stage of the disease is characterized by synovitis. Bone spines (osteophytes) begin to grow on the articular areas (along the edges). The presence of bone growths clinging to each other leads to limited joint mobility.
Over time, they become so large that they bulge, causing the joint to become deformed. The processes occurring in the bone tissue cause compression of small blood vessels and nerve endings, which is accompanied by constant severe pain.
When moving, a crunching sound appears - a characteristic symptom of arthrosis. As joint mobility is limited, the surrounding muscles weaken and decrease in volume.
When the knee joint is damaged, pain occurs when walking (especially on stairs): tissue friction occurs when moving. Osteoarthritis of the knee is a danger associated with joint deformation and the development of ankylosis.
With arthrosis of the hip, the pathology manifests itself in different ways in patients. Signs depend on the degree of inflammation.
- What is arthrosis of the foot and how to treat it?
If measures are not taken, the pathological process progresses over time, and inflammation affects other joints.
Diagnosis and treatment of arthrosis of the knee joint
Diagnosis of arthrosis of the knee joint takes place in the office of a rheumatologist or orthopedist. The doctor examines the affected joint, palpates it, listens to complaints and asks additional questions. Performs several tests - for example, asking the patient to bend his leg or walk a few steps. Then, if it is necessary to clarify the stage of the disease or the nature of pathological changes, he refers for additional studies. For example, for computed tomography or radiography.
Treatment of arthrosis of the knee joint is often complex, aimed at eliminating pain and restoring cartilage, ligaments and joint functions.
To reduce pain, anti-inflammatory drugs, creams, and rubs are used. To protect joint tissue - chondoprotectors. Sometimes hormonal drugs are prescribed.
Physiotherapeutic procedures and therapeutic exercises aimed at activating blood circulation in the joint area and strengthening the surrounding muscles are effective.
If the changes are irreversible, surgical treatment - prosthetics - is prescribed.
Causes of childhood osteoarthritis
In children, arthrosis can develop due to increased loads that exceed the functional capabilities of the joints. Often there are several factors causing the disease:
- congenital hip dysplasia;
- weak muscular-ligamentous apparatus;
- traumas suffered in early childhood;
- excess body weight;
- disruption of metabolic processes.
Tissue maturation in children has not completed; they are easily injured during active movement. In adolescents, the disease is often associated with injuries received during outdoor games and sports.
The resulting injuries (subluxations, sprains, fractures) are accompanied by an inflammatory process that has a negative effect on cartilage tissue, joint fluid, and soft tissues.
As a result of injury, joint deformation and displacement from its natural position may occur. Lack of timely treatment leads to the development of irreversible processes: rubbing tissues wear out faster.
Hip dysplasia is accompanied by a disorder of bone structure. As a result of the unnatural arrangement of bones, the risk of arthrosis increases: due to displacement, the joints are overloaded, and the muscles take on excess weight. Dysplasia is a common cause of coxarthrosis.
Disturbances in metabolic processes can lead to degeneration of cartilage tissue due to untimely receipt of necessary substances.
With excess body weight, pressure on weak joints increases, having a negative impact on them. Adolescence is characterized by rapid bone growth and a simultaneous lag in muscle strength and an increase in mass.
Reactive arthritis
The disease occurs 2-3 weeks after treatment of infections, which often occurs due to weakened immunity.
Symptoms
- Drowsiness appears and the temperature rises.
- Often the joints of the legs become swollen, swollen and inflamed.
- Reactive childhood arthritis may require treatment for eye inflammation (photophobia, severe redness, increased tearing).
- The pain in the affected areas becomes stronger when they are disturbed.
- Even a month before the lesion, the child’s temperature may rise, and sometimes there is frequent urination. This is also common with intestinal infections and chlamydia infections.
- There may be pain in the posterior ankle area.
How is it recognized?
- Stool testing is designed to help identify residual traces of salmonella, shigella or yersinia (bacteria that can cause dysentery or salmonellosis).
- A blood test detects the presence of antibodies to bacteria that indicate a previous infection (for example, chlamydia).
- A urine test is needed to determine the quantitative and qualitative composition of white blood cells and various bacteria.
Treatment
Reactive arthritis in children is treated with anti-inflammatory non-steroids. The most important principles of treatment:
- Do not put stress on your joints.
- The use of antirheumatic drugs for complications.
- The use of antibacterial drugs when chlamydia is detected.
- Injection of non-steroidal hormones into the joint itself if necessary.
Treatment of reactive arthritis in children lasts from 2-3 weeks to a year. With a mild course, the symptoms begin to disappear within 2-3 days after the start of treatment measures. Arthritis does not cause irreversible consequences. Treatment should be carried out as effectively as possible to avoid relapse.
Diagnostics
To make a diagnosis, it is necessary to conduct a comprehensive examination. The doctor clarifies the complaints, examines and palpates the joint, and notes the range of motion.
Muscle atrophy is detected by measuring the circumference and length of the diseased limb, then compared with that of a healthy limb. Additional methods are used:
- What is grade 1 arthrosis and how to treat it?
- blood and urine tests;
- blood chemistry;
- synovial fluid analysis;
- X-ray diagnostics;
- Ultrasound;
- CT;
- MRI.
Treatment
With an integrated approach to treatment, techniques are used aimed at saving the joint. A distinctive feature of the therapy is the impossibility of using medications approved for adults; it is more similar to methods of treating the disease in pregnant women, when there are many restrictions.
The main tasks that the doctor must solve:
- prevent ossification;
- restore mobility;
- normalize blood supply and necessary nutrition.
For this use:
- chondroprotectors;
- exercise therapy;
- physiotherapeutic procedures;
- traditional medicine;
- drug treatment for acute forms;
- surgical treatment;
- Spa treatment.
Among medications, NSAIDs (Indomethacin, Naproxen, Diclofenac, Ibuprofen) are used to relieve acute manifestations. For severe inflammation, glucocorticoids are prescribed.
Chondroprotectors are used to influence hyaline cartilage. The drugs have contraindications and undesirable effects. The course lasts several months.
In case of exacerbation, analgesics and anti-inflammatory drugs are used in the form of injections. For muscle spasms, muscle relaxants are prescribed.
When using surgical methods of treatment, the diseased organ is replaced with an artificial one (arthroplasty, endoprosthetics) or the head is resurfaced (arthroscopy), osteotomy, and cleaning using special equipment (debridement).
The operations are expensive and not performed in all clinics, so this method is used in extreme cases.
Physiotherapeutic treatment improves blood circulation in the sore joint. Ultrasound, shock wave therapy, and low frequency currents are used.
- How to treat arthrosis of the foot at home: folk remedies and medications, video
Exercise therapy helps increase bone mobility and improve microcirculation. Exercises are done outside the period of exacerbation. You can perform special gymnastics at home.
Sanatorium-resort treatment is aimed at improving metabolic processes and nutrition of the musculoskeletal system. Many sanatoriums have swimming pools, special exercise equipment, etc.
Juvenile ankylosing spondylitis
This is a chronic inflammation, the causes of which are unknown to science. This arthritis is also called ankylosing spondylitis.
Signs
- The appearance of edema at the site of inflammation.
- After waking up, the child moves stiffly for about 30 minutes.
- Asymmetry of inflammation.
- A clear sign of this particular type of arthritis in children is sudden pain in the spine or legs.
- The joints of the spinal column may be damaged, which results in painful sensations in the lower back and legs.
- Arthritis is often accompanied by ulcerative colitis and uveitis.
How is it recognized?
- Immunogenetic testing detects the HLA-B gene complex
- Rheumatoid factor was negative during the diagnosis of this arthritis in children!
- X-ray examination of the spinal column, bones, joints reveals inflammatory and deformative symptoms, deposits of potassium salts between cartilage and vertebral discs.
- A general qualitative and quantitative blood test reveals the inflammatory process.
Treatment
- It is necessary to strictly adhere to medical instructions regarding drug therapy.
- Exercise (usually swimming). But specialist supervision is required.
- Non-steroidal drugs are prescribed to reduce the intensity of pain. Antirheumatic and biological agents are also used for the same purposes.
Prolonged illness can lead to partial deformation (sometimes destruction) of the joints, resulting in disability.
Complications
When joints are damaged, the patient experiences severe pain and loses the ability to perform usual actions. An unpleasant complication is loss of organ function, deterioration in quality of life, and disability.
Trying to reduce the load on the diseased limb, patients load the healthy one, which contributes to the development of other pathologies and worsening of the condition.
If large joints of the lower extremities are affected, the affected leg is shortened, the center of gravity of the body shifts, and the load on the spine increases. This cannot pass without leaving a trace on the body.
Prevention of adolescent DOA
Preventing a disease is easier than treating it. Prevention measures are:
- physical activity that does not overload weak joints;
- walking, swimming (help strengthen muscles and ligaments);
- proper nutrition (inclusion in the diet of foods that strengthen cartilage tissue, containing vitamins C, group B);
- body weight control (the child’s weight should be in accordance with normal values for a given age);
- See a doctor if discomfort or joint pain occurs.
It is recommended to teach the child to group himself when falling. Shoes should be comfortable, made from natural materials, and have a stable sole.
Unconventional methods
Arthrosis can be treated using traditional medicine. Turning to the practices of traditional healers for childhood arthrosis is completely justified and is due to the fact that the disease at this age is much less pronounced, and the use of most serious medications is also contraindicated.
It should be emphasized that treatment with traditional methods is more effective when compared with the use of traditional recipes. Therefore, if there are no contraindications, it is still advisable to prefer drug therapy. However, natural remedies can also become an excellent complement to drug therapy, and sometimes they are able to completely defeat the disease when it has not yet become too advanced.
It is worth noting such a nuance that unconventional drugs do not bring such effective results; they are less effective than drugs of conservative medicine. But they have a significant advantage - almost all drugs are harmless. A noticeable healing effect as a result of their use comes only after a few months. The arsenal of such drugs contains natural remedies used as rubbing liquids, tinctures, and compresses. Since usually a small child does not suffer from arthrosis as much as an adult, he can often be cured with folk remedies without using strong medications.
Arthrosis in adults
Arthrosis is a chronic disease in which degenerative-dystrophic changes occur in the joints. Osteoarthritis can impair joint function, and in later stages, complete destruction of the joints and loss of motor functions can occur.
The disease is more often diagnosed in patients over 45-50 years of age, but it also occurs at an earlier age, and even in children.
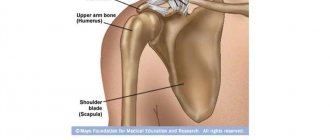
Large articular joints are most susceptible to arthrosis: the knee and hip joints, and the shoulder joint. But there are also other types of the disease, which will be discussed below.
Arthrosis in women
Predisposition to arthrosis is transmitted genetically. The development of the disease can be affected by congenital features or defects in the structure of connective tissue and joints (dysplasia), especially in combination with acquired factors. The latter may include injuries, obesity and other diseases.
Before the age of 45, arthrosis is diagnosed in 2-3% of women, but this percentage increases more than 10 times in the age range from 45 to 60 years. After reaching the age of 65, symptoms of arthrosis occur in 70% of women. Men suffer from this disease somewhat less frequently.
Arthrosis in pregnant women
Arthrosis in pregnant women can significantly complicate bearing a child. And not only because due to the inevitable increase in body weight, the load on the joints increases significantly. During pregnancy, it is necessary to eliminate or significantly reduce the intake of certain medications used to treat arthrosis.
In particular, this applies to drugs belonging to the group of non-steroidal anti-inflammatory drugs, the use of which is contraindicated during pregnancy.
A woman does not always know about the arthrosis she has: the disease can manifest itself after conception, under the influence of hormonal changes and weight gain. But if symptoms of arthrosis have appeared before, pregnancy planning must necessarily include a preliminary examination and treatment.
It is necessary to weigh all the risks associated with joint arthrosis and accurately determine the degree of development of the disease. Arthrosis in pregnant women can worsen in the first trimester, then subside, and again appear after childbirth.
Therefore, pregnancy management in a woman with arthrosis of the joints is carried out in close cooperation with a gynecologist, orthopedist and rheumatologist. Doctors jointly resolve issues related to the treatment plan for arthrosis, taking medications, and prescribing a special regimen. A pregnant woman may need to wear special orthopedic devices designed to alleviate arthrosis and not interfere with pregnancy. These could be knee pads, elbow pads, or corsets.
In agreement with doctors, traditional methods of treating arthrosis can be used, but no amateur activities should be allowed.
Arthrosis in nursing women
After childbirth, arthrosis in women can become more complicated due to increased physical activity. But treatment can be significantly complicated due to the inadmissibility of taking many medications that are incompatible with breastfeeding.
Therefore, it makes sense to take care of disease prevention: avoid putting too much stress on the joints, and do not overload them. Help from loved ones in carrying out tasks associated with significant physical activity can significantly make the life of a nursing woman easier.
It is better to prevent the disease than to decide how to treat arthrosis during pregnancy.
Diseases of the hip joints in children
Most often, adults develop arthrosis of the knee and hip joints, and the same trend can be seen in children. The knee joints are most susceptible to injury and suffer from overload, but arthrosis of the hip joint in children is usually dysplastic. Dysplasia is a pathology that is associated with immature bones, improper formation of the joint during intrauterine development, or trauma during childbirth. If the ligaments are weak, the head of the femur is underdeveloped, and the acetabulum is not deep enough, the bone connection becomes excessively mobile. The situation is aggravated by hormonal changes before childbirth.
Hip dysplasia can manifest itself in the form of preluxation, subluxation and dislocation. The first two forms usually resolve spontaneously, but with dislocation, the head of the femur is located outside the acetabulum. If this dysplasia is not corrected, the cavity gradually becomes overgrown with adipose tissue. Children with congenital dislocation of the hip begin to walk later; their gait is unsteady, limping with a unilateral dislocation, and waddling with a bilateral dislocation. Uncorrected hip dislocation provokes arthrosis of the hip joint in children. Typically, dysplastic coxarthrosis develops after 25 years, but earlier manifestations also occur. In addition to congenital hip dislocation, childhood arthrosis of this localization can be associated with the following pathologies:
- congenital malformation (delayed ossification) of the proximal femur - a rare pathology, occurs in 0.002% of newborns;
- Perthes disease (aseptic necrosis of the head of the femur in children) - impaired blood supply to the bone tissue of the head and nutrition of the cartilage due to a congenital malformation or joint injury, infection;
- advanced coxopathy (coxitis, arthritis of the hip joint) is an inflammatory process of post-traumatic, infectious, autoimmune nature.
The risk of developing arthrosis increases during periods of rapid bone growth.