Cubital tunnel syndrome, also called cubital tunnel syndrome, is a condition in which the ulnar nerve becomes pinched in the joint. In this area, the nerve is located close to the skin and bone, due to which swelling or tissue defects lead to pinched nerves or other pathologies. Nerve deformation is also possible.
The cubital canal is the space in the elbow joint where the nerve leading into the hand is located. This canal is formed by the olecranon process, the epicondyle of the humerus and the ligament that connects them. The nerve responsible for the sensitivity of the little and ring fingers passes through the tunnel.
Cubital tunnel syndrome of the ulnar nerve: symptoms, treatment
Ulnar nerve cubital tunnel syndrome develops as a result of strong and frequent pressure on the nerve itself. And this can be provoked not only by certain physical activities - for example, professional basketball. There are other reasons:
- The habit of often leaning on the elbow, placing it on a hard surface.
- Frequently finding the elbow in a bent position - while sleeping or while talking on the phone.
- Excessive physical activity.
- Abnormal bone growth in the elbow.
Cubital tunnel syndrome of the ulnar nerve, the treatment of which is described below, can be detected in time by paying attention to such symptoms.
- Feeling of numbness in the elbow, pain.
- Tingling in the little finger and ring finger.
- Inability to squeeze fingers normally – especially the little finger and thumb.
- Decreased hand strength.
The last two symptoms indicate that the disease has entered a severe stage - treatment cannot be delayed. At a mild stage of the disease, you can manage with conservative therapy using a protective cut, a splint, reducing pressure on the elbow, and reducing physical activity.
If the disease progresses, surgery will be needed to completely eliminate the symptoms.
In terms of frequency of observations, cubital syndrome is in second place among all neuropathies of the upper limb, second only to compression syndrome of the median nerve at the wrist level. However, the symptoms of ulnar nerve compression are better known than carpal tunnel syndrome.
At some point, most people have experienced numbness and paresthesia in the ring and little fingers when leaning on their elbows for long periods of time or keeping their arm bent at the elbow while talking on the phone or reading in bed. Fortunately, numbness and paresthesia in these situations are transient and rarely progress to neuropathy.
The limits of compression of the ulnar nerve at the level of the elbow joint are limited to 10 cm proximal and 5 cm distal to the medial epicondyle. Five potential points of ulnar nerve entrapment in this area have been identified.
1. Struthers Arcade.
The arcade of Struthers is a musculofascial ligament, 1.5 to 2.0 cm wide, running from the medial head of the triceps (8-10 cm proximal to the medial epicondyle) to the medial intermuscular septum. Although the arcade was found in 70% of cadavers, it is more of anatomical interest than a possible cause of nerve compression. The intermuscular septum and medial head of the triceps are much more likely to cause compression in this area. The septum can cause compression if the nerve passes through its edge, especially in the distal part where it is thicker.
2. Medial epicondyle
The second location for potential ulnar nerve entrapment is at or just proximal to the medial epicondyle. Most often, compression at this site develops as a consequence of fractures of the humerus. In relation to this situation, the term “late ulnar nerve palsy” has been proposed.
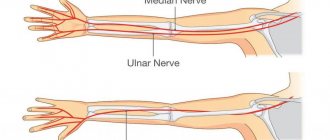
Fig. 1 from the book Operative Techniques: Hand and Wrist Surgery, Kevin C. Chung, MD, MS, 2012
3. Level of the ulnar groove - Cubital canal
At this level, the nerve passes through an osteofibrous tunnel bounded anteriorly by the medial epicondyle, laterally by the olecranon process and the ulnohumeral ligament, and is covered by fibroaponeurotic fascia
Incarceration in this location can be caused by a wide range of injuries and pathological processes, which can be grouped into three categories:
A. Compression of the ulnar nerve as a result of pathological processes localized inside the cubital canal (intracubital compression):
— Bone fragment from a fracture of the epicondyle
— Osteophyte (bone tumor) from the epicondyle or olecranon
— Soft tissue neoplasm
— Synovitis (eg, rheumatoid arthritis)
— Infections (for example, tuberculosis)
- Hemorrhage after injury or due to a bleeding disorder.
B. Compression of the ulnar nerve as a result of pathological processes localized outside the cubital canal (extracubital compression).
Long-term incorrect position of the limb (for example, in patients confined to bed, the left arm of car drivers, patients with incorrect positioning of the arm during surgery, an incorrectly applied splint fixing the elbow joint). Most of these patients already have subclinical nerve compression that is exacerbated by hand positioning.
An abnormal muscle arising from the medial edge of the olecranon process and inserting on the medial epicondyle.
B. Compression of the ulnar nerve as a result of pathological processes leading to its displacement (nerve dislocation).
— Congenital weakness of the fibroaponeurotic part of the cubital canal or its rupture
— Congenital hypoplasia of the humeral trochlea
— Post-traumatic deformity of the medial epicondyle
4. Fourth place of potential compression
-
the point where the nerve passes between the two heads of the flexor carpi ulnaris muscle.
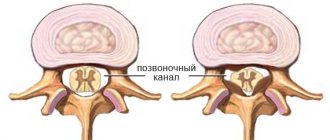
The lower part of the canal is limited by the medial collateral ligament of the elbow joint, the upper part is a fibrous ligament, which is a continuation of the fibroaponeurotic fascia covering the nerve at the level of the ulnar groove. The most commonly used name for this fibrous ligament is “Osborne’s fascia”, and terms such as triangular ligament, arcuate ligament, or humeroulnar arch are also used. The ulnar nerve is most susceptible to compression in the cubital tunnel because the cross-section of the canal changes when the limb is flexed at the elbow joint. The Osborne ligament stretches 5 mm for every 45 degrees of flexion and becomes tense, and the medial collateral ligament relaxes, thickening in the middle and moving medially. In this regard, the cross-sectional contour of the cubital canal changes from oval (with full extension in the elbow joint) to a flat ellipse (with full flexion). As a consequence of these changes, the pressure inside the canal increases 7 times, and with additional contraction of the flexor carpi ulnaris muscle, it increases up to 20 times.
5.Flexor-pronator aponeurosis
The fifth zone of compression of the ulnar nerve is where the nerve exits from under the flexor carpi ulnaris muscle, piercing the fascial septum, and located between the deep and superficial flexor digitorum muscles. The fascial bridge in this area is otherwise called the flexor-pronator aponeurosis. Similar to the Struthers arcade level, compression at this level is uncommon.
PATHOPHYSIOLOGY AND CLINICAL SYMPTOMS OF ULNA NERVE COMPRESSION
Progressive structural changes that occur in the nerve trunk during chronic compression lead to predictable clinical symptoms and physical findings. The result of mechanical compression of the nerve is a local deterioration of intraneural circulation, which manifests itself already at an external pressure of 20 mm Hg. Art. At the initial stage of the pathological process, a violation of the blood-neural barrier occurs, which is accompanied by swelling of the nerve and aggravation of microcirculatory disorders. Deterioration of blood circulation causes nerve ischemia, which is manifested by the appearance of paresthesia and hypoesthesia in the 4-5 fingers of the hand. At this stage of the disease, changes in the nerve fibers also occur in the motor fibers, but these changes can only be detected with instrumental methods of examining patients.
After approximately 6 months of chronic compression, the processes of demyelination of nerve fibers, thickening of the perineurium, and interfascicular fibrosis begin. The combination of ischemic block of axonal conduction and structural changes in the nerve leads to a decrease in the conductivity of the motor nerves and an increase in the threshold of the sensory nerves, which is manifested by weakness of the hand muscles (positive Froment's sign - an attempt to hold a sheet of paper between the index finger and the thumb located on top is accompanied by slight flexion of the nail phalanges of the thumb; positive Wartenberg's sign (inability to actively adduct the little finger), as well as decreased sensitivity (increased indicators of the two-point discrimination test) in the area of innervation of the ulnar nerve.
At the late stage of chronic compression of the ulnar nerve, axonal death occurs in it. Axonal losses are manifested by hypotrophy of the hand muscles, and ultimately by their paralysis and complete atrophy, as well as complete anesthesia of the innervated zone.
Unlike chronic, with acute nerve compression, when there is a significant increase in pressure on the nerve over a short period of time, the sudden onset of pain, paresthesia and movement disorders is noted within a few hours after the onset of the disease.
DIAGNOSTICS
The primary diagnosis is based mainly on the clinical picture and the results of provocative tests. In most patients, when tapping in the projection of the place of compression of the ulnar nerve, Tinel's symptom appears; it should be noted that this symptom is quite sensitive and can often be positive on both hands. The second test involves full flexion of the elbow joint and maximum extension of the wrist joint (can be combined with finger compression of the ulnar nerve proximal to the cubital canal). The test is considered positive if pain or paresthesia occurs after a minute. The test has good sensitivity and specificity.
The diagnosis is confirmed by electroneuromyography (ENMG).
Study of the conductive function of motor fibers of the nerve (Fig. 2). Local decrease in SRV at the elbow level below 50 m/s or a relative decrease in SRV compared to the distal and proximal points by more than 10 m/s. The decrease in the amplitude of the M-response above the elbow level should exceed 20%–25%. After 6-12 months of nerve compression, the amplitude of the M-response at the distal point will also be reduced.
Rice. 2 Fig. 3
Study of the conductive function of sensory nerve fibers (Fig. 3). Presence of slowdown or impulse conduction block.
With ultrasound examination of the nerve, it is possible to determine its position (important in case of dislocations), accurately determine the location of compression, as well as the morphostructure of the nerve. (Fig. 4,5,6)
Rice. 4 Fig. 5
Rice. 6
CONSERVATIVE TREATMENT OF CUBITAL SYNDROME
In patients with this pathology, conservative measures are aimed at reducing pressure on the ulnar nerve. This is achieved by instructing patients on organizing the workspace, avoiding prolonged forced flexion in the elbow joint, as well as static splinting in the position of flexion in the elbow joint by 30 degrees, with mandatory fixation of the hand in a neutral position (to avoid contraction of the flexor carpi ulnaris muscle).
Paraneural injections of glucocorticoids are not used for this disease.
If the patient's symptoms of cubital tunnel syndrome persist after more than 3 months of conservative treatment, and there is a decrease in conduction velocity during ENMG, the patient is indicated for one of the options for surgical decompression of the ulnar nerve.
SURGICAL TREATMENT OF CUBITAL SYNDROME
The results of surgical treatment depend on a number of factors, which include the age of the patient, the duration of compression and the severity of clinical symptoms. Young patients with cubital syndrome of several months' duration tend to have a better prognosis after nerve decompression.
All operations for decompression of the ulnar nerve can be divided into two groups:
1. decompression without transposition of the ulnar nerve (decompression “ in situ”, medial epicondylectomy)
2. decompression with transposition of the ulnar nerve
- subcutaneous transposition,
- intramuscular transposition,
- submuscular transposition.
Decompression " in situ"
Decompression without ulnar nerve transposition is often called “simple decompression.” Surgery is usually indicated for patients with a mild degree of compression, mild symptoms with relatively short-term compression, and no previous skeletal trauma.
In situ decompression is the least complicated of all the operations performed for cubital syndrome.
Under plexus anesthesia or intravenous anesthesia, the aponeurosis is dissected from the incision in the projection of the ulnar nerve between the olecranon process and the medial epicondyle and the heads of the flexor carpi ulnaris are separated. The nerve is isolated distally, preserving the branches of the nerve to the flexor carpi ulnaris and the capsule of the elbow joint.
The advantages of in situ decompression are the simplicity of the surgical technique, minimal dissection of the ulnar nerve while maintaining its blood supply, rapid reduction of postoperative pain, the possibility of using local anesthesia, and the absence of the need for postoperative immobilization.
Potentially insufficient decompression, higher recurrence rates, ulnar nerve subluxation, and the ability to use this technique in patients with abnormal bony anatomy (eg, cubitus valgus) limit its use.
Medial epicondylectomy
Resection of the medial epicondyle provides expansion of the cubital canal. And in combination with its dissection, it reduces compression of the nerve during flexion of the limb at the elbow joint, eliminating the need for anterior transposition of the nerve.
Under plexus anesthesia or intravenous anesthesia, decompression of the ulnar nerve is performed, as in the case of in situ decompression. The ulnar nerve remains in its bed. There is no need to perform intrastem or external neurolysis. The medial epicondyle is approached subperiosteally, preserving the attachment of the flexor and pronator teres muscles to the periosteal coupling.
Care should be taken not to open the elbow joint capsule or detach the ulnar collateral ligament. To avoid detachment and damage to the anterior medial band of the ulnar collateral ligament, the resection plane should not be along the medial edge of the trochlea of the humerus, as traditionally described earlier, and should be carried out to no more than 20% of the total depth (average 5 mm of the protruding edge of the epicondyle) . The epicondyle fragment with the attached medial intermuscular septum is removed. The raw edges of the bone are then realigned and the periosteal flap is sutured in an overlapping manner with immersed 3-0 nonabsorbable sutures.
The full range of movement in the elbow joint is checked and the sliding of the ulnar nerve and the absence of compression zones in the distal and proximal directions are monitored. Skin sutures and a cotton-gauze bandage are applied. On days 2-3 after surgery, early active and passive development begins.
Possible complications of this technique are:
— Medial instability of the elbow joint, which is a consequence of “excessive” resection of the epicondyle
- Long-term pain in the area of the medial epicondyle.
– Decreased grip strength and wrist flexion
— Stiffness of the elbow joint (mainly due to prolonged immobilization)
— Formation of bone exostoses
Ulnar nerve decompression with transposition is performed more often than without transposition for two main reasons.
The first is that the nerve moves to a new favorable bed, which is devoid of scars. The second reason is that by moving the nerve, the tension on the nerve that usually occurs when the limb is flexed at the elbow joint is reduced.
Anterior transposition of the ulnar nerve is indicated in pathological conditions accompanied by subluxation of the nerve, valgus deformity of the elbow joint, and in patients with persistent symptoms of nerve compression after simple decompression.
Anterior subcutaneous transposition
The subcutaneous transposition is the most commonly performed of the three types of anterior ulnar nerve transposition. It is used for open surgical treatment of fractures and dislocations of the elbow joint, during joint replacement. Anterior transposition is performed when the nerve is suture, in conditions of a deficiency in its length (during excision of nerve tumors or old injuries).
Under plexus anesthesia or intravenous anesthesia from the posteromedial approach, while preserving the branches of the medial cutaneous nerve of the forearm, access is made to the ulnar nerve, which is allocated along the entire length from the arcade of Struthers to the flexor-pronator aponeurosis. The nerve travels subcutaneously to the anterior surface of the elbow joint. It has been proposed to use a special fasciodermal flap to retain the displaced nerve.
The main advantages of subcutaneous transposition include ease of implementation and relative lengthening of the nerve, which reduces its tension when flexing the elbow joint.
The main disadvantages of the technique are devascularization of the nerve over a large extent and damage to some of its branches during wide mobilization. Susceptibility to injuries of the displaced nerve (especially in active people, athletes).
Anterior intramuscular transposition
While subcutaneous transfer is the most commonly used procedure for compressive ulnar nerve neuropathy, intramuscular transfer is the most controversial. The authors of the method propose immersing the ulnar nerve into a canal specially formed in the pronator teres muscle. After surgery, 3 weeks of immobilization and limitation of vigorous activity for up to 10 weeks are recommended.
It is the technical part of the method that makes it controversial. The formed intramuscular canal is located at a right angle to the displaced nerve. And, therefore, periodic contractions of the muscle will lead to increased traction forces on the ulnar nerve, which ultimately will further aggravate compression of the nerve. Dissection of the muscle also leads to the formation of a scar and secondary compression of the nerve.
Although proponents of this technique report good results in their studies, complications are common.
Submuscular transposition
This operation has a number of advantages compared to the other two types of ulnar nerve transposition - guaranteed decompression of the nerve at all potential points of compression, the nerve is moved to an area free of scar changes, and anterior, deep transposition creates its maximum relative lengthening. Since the nerve is covered by muscle mass, it is well protected from external influences, which is an important factor in active people. This method is also recommended for use in cases of ineffectiveness of other previously performed operations for cubital syndrome. Submuscular transfer is considered the most predictable of all ulnar nerve decompression procedures.
Under plexus or general anesthesia on the exsanguinated limb, from an incision in the projection of the cubital canal, access is made to the ulnar nerve, preserving the branches of the medial cutaneous nerve of the forearm, a nerve that extends along the entire length from the arcade of Struthers to the flexor-pronator aponeurosis. The proximal edge of the pronator teres muscle is then identified and cut away, and the brachialis muscle is further visualized. The medial collateral ligament of the elbow joint is isolated and preserved, and the mass of the flexor-pronator group is cut off from the medial epicondyle and retracted. The ulnar nerve moves anteriorly and is placed on the brachialis muscle. The motor branch to the flexor carpi ulnaris muscle is preserved and mobilized by intrafascicular dissection. Using transosseous sutures, the flexor-pronator group muscles are again fixed to the medial epicondyle under visual control to prevent the nerve from entering the suture. The fibrous covering of the epicondylar groove and the fascia between the heads of the flexor carpi ulnaris are sutured with separate sutures.
After surgery, the limb is fixed in a posterior plaster splint in a position of flexion at the elbow joint of about 35 degrees, the forearm and hand in a neutral position for a period of 3 to 4 weeks.
Regardless of the method used for decompression, almost all studies report that good results with restoration of limb function are observed in patients with a relatively short medical history and minimal degree of compression (ie, intermittent symptoms without weakness and with normal two-point discrimination).
In patients with severe ulnar nerve compression (ie, those with abnormal two-point discrimination and/or muscle atrophy), regardless of the technique used for decompression, success rates range from 60% to 80%, and recurrence rates range from 25% to 33 %.
Cubital tunnel syndrome – treatment at the Surgery Center
Ulnar nerve tunnel syndrome can be successfully treated with timely referral to specialists. The Surgery Center offers a full range of services necessary for the diagnosis and successful treatment of the disease.
Why patients choose us:
- Surgeons with more than 8 years of experience.
- We specialize in hand surgery.
- Painless surgery without discomfort.
- There are no hidden fees - the price already includes examination, diagnosis, surgery and subsequent hospital care.
- Convenient work schedule.
- Modern equipment.
- Full support after surgery, including communication with the surgeon or a specialized specialist.
- Possibility of cash and non-cash payments.
Patients of our clinic receive qualified medical care and a comfortable stay within the walls of the center. We will help you regain your health! You can sign up for a consultation by ordering a call back on the website.