Facet syndrome
When intervertebral discs change due to disease or injury, increased stress is placed on the facet joints.
As a result, inflammation occurs in these joints (spondyloarthritis), and then a degenerative process develops (spondyloarthrosis). The pain syndrome that accompanies them is called facet pain. Depending on the most affected part of the spine, it manifests itself as pain in the neck, back and limbs. The most common form is lumbar facet syndrome, the symptoms and treatment of which are also covered in this article. It is believed that up to 80% of people suffer from this pathology in old age, and up to 40% of adults in general experience back and neck pain.
Often, symptoms of the disease appear when the facet joints are already seriously affected. So surgery is sometimes practically the only way to achieve lasting pain relief. In any case, they provide 5-6 times longer remission of the disease than conservative treatment methods.
FACETOPLASTY
A minimally invasive innovative technology for introducing ViscoPlus synovial fluid prosthesis into the joint cavity is called facetoplasty. The main component of the complex liquid is hyaluronic acid.
The procedure helps restore the normal structure of the affected joint, “attracts” (sorbs) additional water molecules and retains them in the joint cavity. As a result of the operation, the normal volume of the joint is restored, pain and limitation of movement are reduced. There is evidence of stimulation of regeneration of cartilage surfaces.
Unfortunately, the administration of ViscoPlus and other similar drugs is possible only in cases where there are no signs of abnormal joint shape or bone growths. In practice, facetoplasty in the treatment of the spine is used for patients in the middle age group up to 60 years.
Facet joint block
Effectively relieves pain by administering local anesthetic drugs in combination with a glucocorticoid hormonal agent directly into the cavity of the facet joint, or into the area where the sensory nerve passes. The anesthetic temporarily blocks the transmission of impulses along the nerve, instantly relieving pain, while the glucocorticoid hormone, having a pronounced anti-inflammatory effect, quickly eliminates the inflammatory process, swelling and compression of tissue (the main causes of pain), thereby prolonging the effect of the blockade.
Causes of the disease
This syndrome can occur due to various reasons. Their identification plays an important role, since it directly affects the treatment method. In order to correctly identify the cause of the disease, contact the CELT Pain Clinic. We have modern diagnostic methods and will direct every effort to return you to normal life.
At CELT you can get advice from a specialist algologist.
- Initial consultation – 4,000
- Initial consultation with the head of the Pain Clinic - 4,500
Make an appointment
RADIO FREQUENCY DENERVATION OF SPINAL JOINTS
In cases where the facet joints are changed and surrounded by bone growths (osteophytes), the most suitable minimally invasive surgical method for permanent relief from pain is denervation. Various methods of influencing the own nerve of the joint are used - mechanical, thermal destruction. The most advanced technique that provides minimal damage with maximum efficiency and predictability is radio frequency.
With radiofrequency denervation, thermocoagulation of tissue occurs under the influence of ultra-high frequency electric current. Special needles are applied to the nerves of the diseased joint and an electric current is passed, causing the tissue to heat up to 70 degrees. The nerves are actually cauterized, blocking the passage of pain impulses. At the Yauza Clinical Hospital, denervation of vertebral joints is carried out using a Stryker radiofrequency generator.
The method can be applied in all cases except those when the spinal canal is narrowed or the joint is severely deformed. It is used to treat elderly and even elderly patients. There are practically no complications observed, the duration of pain relief is more than a year.
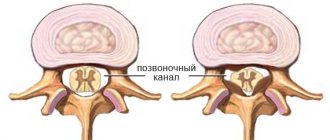
Articulating surfaces
The facet joint is formed by the articular surface of the superior articular process of the underlying vertebra and the articular surface of the inferior articular process of the overlying vertebra. In the cervical and thoracic spine, the articular surface of the upper articular process of the underlying vertebra is flat, in the lumbar region it is convex (the articular surface of the lower articular process of the overlying lumbar vertebra is concave and forms an arc, the apex of which faces the vertebral body).
Friends, the seminar “Joint mobilizations (lower quadrant)” will take place very soon. Find out more...
The facet joints have different orientations depending on the part of the spine:
- Cervical: 45 degrees; frontal plane; All movements are possible, such as flexion, extension, lateral bending and rotation.
The articular surfaces of the facet joints of the cervical spine are located at an angle of 45 degrees to the horizontal plane, with the articular surface of the upper articular process oriented upward and backward, and the lower - downward and forward.
- Thoracic region - 60 degrees; frontal plane; lateral flexion and rotation; minimal flexion/extension.
The facet joints between adjacent thoracic vertebrae are located at an angle of 60 degrees to the horizontal plane and 20 degrees to the frontal plane, with the upper facets oriented posteriorly, superiorly, and laterally, and the inferior facets oriented anteriorly, inferiorly, and medially.
- Lumbar - 90 degrees; sagittal plane; mainly flexion and extension.
The articular surfaces of the lumbar facet joints lie in the sagittal plane; the articular surfaces of the facets are located at right angles to the horizontal plane and at an angle of 45 degrees to the frontal plane. The upper facets are oriented medially, the lower facets are oriented laterally. This changes at the lumbosacral joint, where the articular surfaces are located in the frontal plane, with the lower facet of the L5 vertebra oriented anteriorly. This keeps the spine from sliding forward relative to the sacrum.
PROGRESS OF MINIMALLY INVASIVE OPERATIONS FOR FACET JOINT SYNDROME
- For visual control of operations on spinal joints, the Clinical Hospital on Yauza uses a C-arm intraoperative control complex manufactured by Philips.
- Both facetplasty and facet joint denervation are virtually outpatient procedures. They last less than an hour and do not require hospitalization.
- Anesthesia is used both local and general. The latter is necessary for immobilization and ensuring the patient's immobility. This requires precision manipulation.
- The operation is usually performed at several levels (segments), often on both sides.
- The postoperative period is up to 2 days. Of these, 1-2 hours of bed rest, then, on the same day, the patient can return home, and after a couple of days - to their normal lifestyle. True, you should not drive immediately after surgery, and elderly patients should benefit from the help of an accompanying person on the way home. Sometimes it is recommended to wear a semi-rigid corset for a week.
Using modern diagnostic equipment, specialists from the Yauza Clinical Hospital will quickly and accurately determine the cause of back pain and carry out adequate, gentle surgical intervention that will relieve pain for a long time.
You can make an appointment with specialists at the Center for Vertebrology and Endoscopic Spine Surgery at the Yauza Clinical Hospital using a special form on the website or by calling the phone number indicated on this page.
Facet syndrome at the lumbar level in elderly patients: diagnosis and treatment
Chronic back pain is an important medical and social problem due to its persistent course, frequent lack of significant effect from therapy, and high costs associated with treatment. The relevance of the problem is also due to the fact that, like any chronic pain syndrome, back pain contributes to excessive stimulation of the sympathoadrenal system, which significantly increases the risk of cardiovascular accidents, and negatively affects not only the quality of life, but also its duration. Modern studies have shown that a decrease in life expectancy in older people depends more on the presence of chronic pain than on the presence or absence of life-threatening diseases [1].
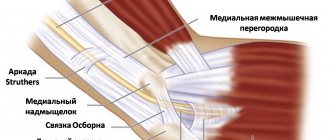
The most common source of chronic back pain, especially in older patients, is the facet joints. Facet joints (synonyms - facet joints, intervertebral joints, articulationes zygapophysiales) are formed at the connection of the lower and upper articular processes of the vertebrae and have a typical structure: articular processes covered with a layer of hyaline cartilage, synovial membrane, synovial fluid and a capsule reinforced by fibers of the multifidus muscle. The orientation of the articular cavities in the cervical region approaches the horizontal plane, in the thoracic region - to the frontal and in the lumbar region - to the sagittal plane. Facet joints have complex and extensive nociceptive and proprioceptive innervation: each joint is innervated from 2-3 segments of the spinal cord, which provides “overlapping” areas of pain. Four mechanisms of irritation of nerve endings in the motor segment have been identified: 1) mechanical or disfixation - due to displacement of the vertebral bodies and articular processes in relation to each other; 2) compression - exostoses, when the joint capsule, meniscoids or free cartilaginous segments in the joint are pinched; 3) dyshemic - due to swelling of periarticular tissues, microcirculation disorders, venous stasis; 4) inflammatory - due to aseptic (reactive) inflammation in the tissues of the motion segment [2].
The incidence of degenerative changes of the facet joints in the population varies widely (from 40% to 85%) due to the use of different diagnostic criteria by different authors and increases with age. For chronic back pain, according to the results of studies conducted using diagnostic blockades, damage to the facet joints is the cause of pain at the lumbar level in 30–60% of cases, at the cervical level in 49–60%, at the thoracic level in 42–48% cases [3].
Facet syndrome, as a rule, refers to painful manifestations of spondyloarthrosis, in which there is no compression of the spinal nerve root or other neurovascular formations by elements of the pathologically altered motion segment. Instead of the term “facet syndrome”, “spondyloarthralgia syndrome”, “small joint inflammation syndrome of the spine” or “mechanical low lumbar syndrome” are also used. Many authors consider the terms “facet syndrome” and “spondyloarthrosis” as synonyms. Spondyloarthrosis, which is the morphological basis of facet syndrome, is a particular form of osteoarthrosis, which is a heterogeneous form of diseases with different clinical presentations and outcomes, which are based on damage to all the constituent elements of the facet joints - cartilage, subchondral bone, ligaments, capsule and periarticular muscles. In lumbar spondyloarthrosis, a sharp decrease in the thickness of the articular cartilage was found, up to its complete disappearance in certain areas where bone tissue proliferation was noted. Spondyloarthrosis can develop in isolation, but much more often it develops against the background of degeneration of the intervertebral discs, leading to increased load on the facet joints and their chronic traumatization. Like disc damage, spondyloarthrosis is more often observed in elderly patients, but can also develop in young people, which is facilitated by hereditary predisposition, congenital anomalies, spinal injuries, hypermobility of spinal motion segments (SMS), and excess body weight. In case of injuries (whiplash type, traction, rotation), facet syndrome can develop acutely.
The development of spondyloarthrosis is associated with disturbances in the functional anatomy of the spinal column, the anterior sections of which (including the intervertebral discs) are intended mainly to resist gravity (compression), and the posterior sections (including facet joints) are intended to stabilize the spine during rotation and displacement of the vertebrae in the anteroposterior direction. Normally, 70–88% of the axial compression load falls on the anterior sections and only 12–30% on the posterior sections. With the development of degenerative changes in the discs, their height decreases, the shock-absorbing function is impaired, and the proportion of the axial compressive load falling on the facet joints gradually increases. Overload of the joints against the background of developing instability of the joint joint leads first to inflammatory changes (synovitis), and then to degeneration of the articular cartilage, deformation of the joint capsules and subluxations in them. This pathological process is asymmetrical in nature, which may be due to uneven load on paired facet joints. Repeated microtraumas, compression and rotatory overloads lead to the progression of degenerative changes in cartilage up to its almost complete loss, the development of periarticular fibrosis and the formation of osteophytes, which leads to an increase in the size of the upper and lower facets, becoming pear-shaped. Under the influence of impulses from the affected PMS, especially from the posterior longitudinal ligament, reflex tension occurs in the intertransverse, interspinous and rotator muscles, which, in the case of their asymmetrical involvement, causes the formation of scoliosis. The combination of changes in the disc, facet joints and muscle-tonic disorders leads to a sharp limitation of movements in the corresponding SMS.
The pain that occurs with facet syndrome is an example of nociceptive pain associated with symptoms of synovitis, direct mechanical irritation of the nociceptors of the joint capsule against the background of instability and muscle-tonic disorders. Most often, spondyloarthrosis develops in the lumbar spine, mainly in the L4-L5 and L5-S1 SDS, which experience the greatest overload. The maximum risk of injury to the facet joints occurs with sudden twisting movements in the lower back. An additional factor contributing to the development of spondyloarthrosis is weakness of the abdominal wall, accompanied by an increase in the severity of lumbar lordosis and compressive load on the facet joints. Much less often, damage to the facet joints is observed in the cervical (mainly at the levels C2-C3 and C5-C6) and thoracic spine. Facet syndrome is characterized by a recurrent course, gradual development and slow regression of each painful episode and a tendency to lengthen and worsen each subsequent exacerbation [4].
The main component of the joint that undergoes degeneration in osteoarthritis is cartilage, consisting of matrix and chondrocytes, in which there is excessive local release of proteolytic enzymes and a progressive slowdown in cartilage repair. This leads to an imbalance between the synthesis and degradation of the extracellular matrix. The matrix contains glycosamines (proteoglycans) and collagen. As the matrix degrades, glycosamines are lost, the resistance of the cartilage matrix to physical stress decreases, and the cartilage surface becomes susceptible to damage. In addition, a wide range of bioactive molecules are synthesized at the chondral level: pro-inflammatory cytokines, free radicals, growth factor, prostaglandin E2, leukotriene B4. This inflammatory component enhances degenerative mechanisms. Inflammation develops primarily in the synovium, leading to impaired filtration of hyaluronic acid through the membrane, its leaching from the joint cavity and the progression of cartilage degeneration. Proinflammatory cytokines are synthesized in the synovium and then diffuse into the articular cartilage through the synovial fluid and are responsible for increased synthesis and expression of matrix metalloproteinases that destroy articular cartilage [5]. Synovial inflammation is directly associated with the occurrence and development of osteoarthritis. Uncontrolled angiogenesis is an important component of synovial inflammation, and these two interdependent processes, angiogenesis and inflammation, are major contributors to the development of osteoarthritis [6]. Thus, the pathophysiological mechanisms of the development of osteoarthritis include not only mechanical damage to the joint and the degenerative process, but also concomitant chronic inflammation, which contributes to the destruction of hyaline cartilage. The structures of the central nervous system associated with the formation of chronic pain syndrome are also involved in the pathological process. Therefore, the leading directions in the pathogenetic treatment of osteoarthritis are modulation of inflammation, regulation of chondrocyte metabolism and stimulation of cartilage synthesis [7].
Features of the clinical picture of facet syndrome at the lumbar level are described in detail [8]. The pain, as a rule, is of moderate intensity, is diffuse, poorly localized, and is described by patients as “deep,” “aching,” “pressing,” “twisting,” “squeezing.” The phenomenon of “morning stiffness” and the maximum severity of pain in the morning (signs reflecting the inflammatory component), as well as after exercise at the end of the day (which is due to the phenomena of instability and disfixation in the area of the affected SMS) are characteristic. The pain is localized paravertebrally and can be bilateral or lateralized. Pain emanating from the facet joints of the lower lumbar level (L4-L5, L5-S1) can be reflected along the sclerotomes in the gluteal region, coccyx area, hip joint, groin, in the thigh (along the posterior surface) and, as a rule, does not “descend” below the knee. Pain from the joints of the upper lumbar level (L1-L2, L2-L3, L3-L4) can spread to the chest area and the lateral surface of the abdomen. Pain with facet syndrome at the cervical level can be reflected in the area of the shoulder girdle and/or upper back and much less often - in the shoulder, forearm, hand (more typical for discogenic radiculopathies). From exacerbation to exacerbation, the pain pattern (its location, nature and intensity) may change. A characteristic feature of facet pain syndrome at the lumbar level is the appearance or intensification of pain during extension and rotation of the lumbar spine, which occurs when moving from a sitting position to a standing position, during prolonged standing, or “twisting” in the lower back. In this case, bending and tilting in the lumbar region can lead to a decrease in pain. The pain decreases while “unloading” the spine - lying down or when bending the spine with support on the hands (stand, railings). Unlike pain syndrome with radiculopathy, referred pain with facet syndrome does not reach the fingers, is poorly localized, does not carry the patterns of neuropathic pain syndrome (sensations of “electric current”, burning, paresthesia, etc.), intensifies with extension (and not flexion) ) of the spine, is not accompanied by the appearance of pronounced symptoms of tension (Laseg, Matskevich, Wasserman), as well as symptoms of loss in the motor, sensory and reflex spheres. A neurological examination reveals smoothness of the lumbar lordosis, scoliosis in the thoracic and lumbar regions, local pain in the Kemp test, local pain on palpation in the projection of the “problem” facet joint, tension in the paravertebral muscles and quadratus dorsi muscle on the affected side, discomfort and limited range of motion during bending back. The muscle tension around the intervertebral joint is determined by palpation. As a rule, there are no neurological sensory, motor or reflex disorders. Unlike radicular syndrome, the symptoms of “tension” are not typical, nor is there any restriction of movement in the legs.
X-ray examination is sufficiently informative, but the detection of degenerative changes in the facet joints does not mean that these changes are the cause of the pain syndrome. In an asymptomatic population, dystrophic changes in the facet joints are detected in 8–12% of cases [9].
The generally accepted standard and the only evidence-based method for confirming the connection of pain with the pathology of the facet joints is the disappearance (or significant reduction) of pain a few minutes after blockade of the medial branch of the posterior primary branch of the spinal nerve under visual control [10]. But diagnostic medial branch blocks are not a widely used method in routine clinical practice.
The main treatment for facet syndrome is the use of painkillers and nonsteroidal anti-inflammatory drugs (NSAIDs), and the issue of treatment safety is of particular relevance. This is due to the chronic recurrent nature of the pain syndrome, requiring repeated, often long courses of therapy, as well as the fact that most patients are elderly and senile, which significantly increases the risk of developing gastrointestinal and cardiovascular side effects. According to existing recommendations, patients at risk of developing such gastrointestinal (GIT) events should be prescribed non-selective NSAIDs together with gastroprotectors (proton pump blockers) or selective NSAIDs. In patients at high risk of developing cardiovascular side effects, parallel administration of low doses of acetylsalicylic acid is recommended. In addition, elderly patients often suffer from diseases requiring the use of indirect anticoagulants (atrial fibrillation, recurrent thrombotic syndrome), which, as a rule, is incompatible with the use of NSAIDs. It is also necessary to take into account that not all drugs of the NSAID group can be used for osteoarthritis - an adverse effect on cartilage tissue of NSAIDs such as indomethacin, piroxicam, and naproxen has been identified.
The participation of the articular component in the formation of back pain suggests the inclusion in therapy of drugs that have a symptom-modifying (chondroprotective) effect - symptomatic slow acting drugs for osteoarthritis - SYSADOA. Outside of exacerbation, monotherapy with SYSADOA is recommended. In case of exacerbation of the process and severe pain, it is recommended to combine SYSADOA with NSAIDs, the analgesic effect of which develops much faster. Combined use allows you to reduce the dose of NSAIDs and thereby prevent a number of unwanted drug reactions. SYSADOA group drugs are biologically active substances consisting of cartilage tissue components necessary for the construction and renewal of articular cartilage. SYSADOA are able to influence the metabolism of bone and cartilage tissue and stimulate its regeneration, have a moderate analgesic and anti-inflammatory effect and are devoid of side effects characteristic of NSAIDs, since their mechanism of action is not associated with suppression of prostaglandin synthesis and blocking cyclooxygenase, but is based on inhibition of nuclear factor kB, stimulating the breakdown of cartilage tissue in the body. Among the drugs belonging to this class, only cartilage-related components - glucosamine (GA) and chondroitin sulfate (CS) - have a high level of evidence (1A) of effectiveness over placebo, and also have high bioavailability and good tolerability (EULAR, 2003). GA and cholesterol are natural metabolites of cartilage tissue. HA is an aminomonosaccharide; in the body it is used by chondrocytes as a starting material for the synthesis of proteoglycans, glycosaminoglycans and hyaluronic acid. CS is a key component of the extracellular matrix of cartilage tissue, responsible for maintaining its elasticity and resistance to stress. The anti-inflammatory properties of cholesterol have been well studied [11], but little is known about its effect on angiogenesis. CS affects the production of pro- and antiangiogenic factors by synovial fibroblasts in the synovial membrane affected by osteoarthritis and is able to restore the balance between them. Since angiogenesis is one of the key processes in the development of osteoarthritis, the beneficial effects of cholesterol can be explained precisely by the antiangiogenic properties of this substance [12].
Studies have shown comparable and even more pronounced anti-inflammatory activity of GA and cholesterol to NSAIDs [13]. CS, GA, and their combination demonstrated a structure-modifying effect [14, 15]. When CS and GA are taken simultaneously, their action is synergistic, since both drugs have anti-inflammatory activity, and also have an anabolic effect on the metabolism of cartilage tissue and inhibit catabolic processes in it, simulating the most important functions of chondrocytes in damaged cartilage. However, there are some peculiarities in the mechanisms of action of these two salts. Thus, cholesterol optimizes the composition of synovial fluid, and GA independently stimulates the production of cholesterol [16]. In this regard, combination drugs containing both cholesterol and GA have become most popular. The most studied, of course, is Teraflex. The advantage of Theraflex is the combination of two active ingredients: chondroitin sulfate (400 mg) and glucosamine hydrochloride (500 mg) in one capsule. There is another form of release of the drug for oral administration: Teraflex Advance, which contains chondroitin sulfate 200 mg, glucosamine sulfate 250 mg and ibuprofen 100 mg. Ibuprofen is a safe standard NSAID with a short half-life (less than 6 hours), which does not accumulate and leads to a rapid analgesic effect [17]. The effect of the combination with ibuprofen is recognized as synergistic, and the analgesic effect of this combination is provided by a 2.4 times lower dose of ibuprofen [18]. The mechanism of action of Theraflex is associated with activation of proteoglycan synthesis, inhibition of the action of enzymes that destroy hyaline cartilage, increased production of synovial fluid, decreased leaching of calcium from bones and improvement of phosphorus-calcium metabolism. The indication for the use of Teraflex is pathology of the musculoskeletal system associated with degenerative changes in cartilage tissue. It is recommended to start treatment with the drug Teraflex Advance, 2 capsules 3 times a day, duration of administration - up to 3 weeks, and then switch to taking the basic drug Teraflex, which does not contain NSAIDs (2-3 capsules per day, course 3 months), for prolonging the analgesic effect and protecting cartilage. We conducted our own clinical observation of the effect of the drug on chronic pain syndrome in the lower back.
Purpose of the study: to study the effectiveness and tolerability of Theraflex Advance for facet syndrome in an outpatient setting in elderly patients.
Materials and research methods
We examined 40 patients (12 men and 28 women) suffering from chronic back pain, aged from 60 to 75 years (old age according to WHO classification). The selection criterion was the presence of chronic pain syndrome in the lower back in the acute stage, the cause of which was arthrosis of the facet joints. The diagnosis was confirmed by a comprehensive examination of patients. The neurological and neuroorthopedic status of patients was assessed and clinical manifestations of facet syndrome were identified. The intensity of the pain syndrome was assessed using a visual analogue scale - VAS (Association for the Study of Pain, 1986). Treatment results were assessed by changes in symptoms and the Oswester Disability Questionnaire for Back Pain [19], before drug use and on the 21st day of the study. Plain radiographs of the lumbar spine were evaluated to exclude specific spinal lesions. To clarify pathological changes in the bone structures of the spine and study structural changes in the intervertebral discs and spinal cord, magnetic resonance imaging (MRI) was performed. For diagnostic purposes, blockades with 0.5% novocaine were performed in the affected area of the facet joint (paravertebral). Exclusion criteria were: the presence of organic diseases of the nervous system, mental illness, a history of spinal injuries, somatic diseases in the stage of decompensation. Additional exclusion criteria: sequestered hernias and disc herniations larger than 8 mm; severe hypermobility, spondylolisthesis more than 5 mm; the presence of destructive changes in the vertebral bodies. The patients were divided into two groups: main (n = 16) and control (n = 14). The groups of patients were comparable in terms of gender, age, duration and severity of chronic pain syndrome (VAS scale). X-ray examination of all patients in the affected area revealed a decrease in the height of the intervertebral discs, subchondral sclerosis of the vertebrae, narrowing of the joint space, incongruence of the articular surfaces, and the formation of osteophytes. All patients were prescribed standard drug therapy, which included muscle relaxants, B vitamins, exercise therapy, massage, and an optimal motor regimen was recommended. Patients in the main group were prescribed Teraflex Advance 2 capsules 3 times a day. Patients in the control group received enteric-coated diclofenac 50 mg twice daily and proton pump inhibitor omeprazole 20 mg daily. Considering that side effects, among which the primary concern should be ulceration of the gastrointestinal mucosa, develop more often in people over 65 years of age, the daily dose of diclofenac did not exceed 100 mg. The course of treatment in both groups was 3 weeks. The criterion for the effectiveness of treatment was the absence of pain or a change in its intensity.
Results and discussion
During the therapy, patients in both groups achieved a good analgesic effect: patients noted a decrease in pain along the spine, a decrease in morning stiffness and an increase in mobility.
The severity of pain according to the VAS scale in patients of the 1st group decreased from 4.3 ± 0.9 points to 1.7 ± 0.6 points, in patients of the 2nd group - from 4.2 ± 0.8 points to 1 .8 ± 0.8 points. In patients of both groups, the greatest dynamics according to the Oswestry questionnaire were noted on the scales “pain intensity”, “ability to walk”, “ability to sit”, “self-care” and “ability to travel”, which is associated with a decrease in pain syndrome, “sleep” was less affected " and "the ability to lift objects." There were no significant differences in the analgesic effect between the groups. The study established that Theraflex Advance was well tolerated; no side effects were observed in patients. In patients of the 2nd group, adverse events were observed much more often, while diclofenac was discontinued in 5 patients: 1 patient developed nausea, 2 - pain in the epigastric region, 2 patients suffering from hypertension and receiving antihypertensive drugs - increased blood pressure. pressure, which required discontinuation of diclofenac.
The results obtained are comparable with studies of the clinical effectiveness of chondroprotectors in patients with nonspecific pain in the lower back. For the first time, cholesterol was used for vertebrogenic pathology by KD Christensen et al. in 1989 [20]. Many authors have shown the feasibility of using chondroprotectors in complex therapy of patients with nonspecific back pain [21, 22]. With long-term course treatment of CS, a decrease in the fragmentation of the fibrous ring of the upper intervertebral discs of the lumbar spine was noted [23], a case of regeneration of the intervertebral disc in a patient suffering from back pain associated with degenerative disc disease was described [24], not only a symptom-modifying, but also structural-modifying effect of cholesterol in degenerative-dystrophic pathology of the spine. The safety of cholesterol in patients with concomitant pathology of the cardiovascular system was studied; no occurrence of anginal pain, arrhythmias, or severity of chronic heart failure was noted, and a decrease in blood pressure was noted in patients with arterial hypertension, which made it possible to reduce the average daily dose of antihypertensive drugs [25]. Considering the synergy in the action of GA and cholesterol, a number of researchers recommend prescribing a combination of these drugs for dorsopathies [26, 27]. The optimal synergistic effect is achieved when using GA and cholesterol in a ratio of 5:4; This is the proportion in which these substances are contained in Theraflex. According to the prognostic model, the maximum effect of Theraflex should be expected in the initial stages of degenerative-dystrophic lesions of the spine; clinically, this means using the drug after the first relapse of nonspecific back pain, especially in the presence of symptoms of spondyloarthrosis. In this case, a course of treatment has a preventive effect regarding the chronicity of pain. There is data [28] on the effectiveness of Theraflex in young patients with degenerative-dystrophic diseases of the cervical, thoracic and lumbar spine with acute and chronic pain of varying intensity, both in combination with NSAIDs and as monotherapy. However, the drug can also be useful in cases of advanced spondyloarthrosis; in this case, one can expect stabilization of the condition and a slowdown in the progression of the process [26].
conclusions
Thus, the combination of chondroitin sulfate, glucosamine and ibuprofen (Teraflex Advance) is effective in the treatment of facet syndrome of the lumbar spine in the acute stage in elderly patients. Teraflex Advance has a significant symptom-modifying effect (reducing pain, reducing stiffness, improving motor activity). Teraflex Advance is well tolerated by patients, which helps improve patient adherence to treatment and makes it possible to recommend switching to Teraflex for a long-term symptom-modifying effect.
Literature
- Breivik H., Collett B., Ventafridda V. et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment // Eur. J. Pain. 2006. Vol. 10, No. 4. P. 287–333.
- Lutsik A. A. Pathogenesis of clinical manifestations of spondyloarthrosis // International Neurological Journal. 2009. No. 3 (25). pp. 130–135.
- Brummett CM, Cohen SP Facet joint pain in Benzon: Raj's Practical Management of pain. 4 th ed. Mosby, 2008.
- Cohen S., Raia S. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet joint pain) // Anesthesiol. 2007. Vol. 106. P. 591–614.
- Turovskaya E. F., Filatova E. G., Alekseeva L. I. Dysfunctional mechanisms of chronic pain syndrome in patients with osteoarthritis // Treatment of diseases of the nervous system. 2013. No. 1. pp. 21–28.
- Bonnet CS, Walsh DA Osteoarthritis, angiogenesis and inflammation // Rheumatology (Oxford). 2005. Vol. 44, No. 1. P. 7–16.
- Hassanali SH, Oyoo GO Osteoarthritis: a look at pathophysiology and approach to new treatments: a review // East African Orthopedic Journal. 2011. Vol. 5. R. 51–57.
- Helbig T., Lee C.K. The lumbar facet syndrome // Spine. 1988. Vol. 13. P. 61–64.
- Wiesel SW, Tsourmas N, Feffer HL et al. A study of computer-assisted tomography. The incidence of positive CATscans in an asymptomatic group of patient // Spine. 1984. Vol. 9. P. 549–551.
- Dreyfuss PH, Dreyer SJ Lumbar zygapophysial (facet) joint injections // Spine J. 2003. Vol. 3. P. 505–595.
- Hochberg MC Structure-modifying effects of chondroitin sulfate in knee osteoarthritis: an updated meta-analysis of randomized placebo-controlled trials of 2-year duration // Osteoarthritis Cartilage. 2010. Vol. 18, Suppl. 1. P. S28-S31.
- Lambert C., Mathy-Hartert M., Dubuc J.-E. et al. Characterization of synovial angiogenesis in osteoarthritis patients and its modulation by chondroitin sulfate // Arthritis Research & Therapy. 2012. Vol. 14, No. 2. P. R58.
- Hochberg MC, Martel-Pelletier J., Monfort J. et al. Randomized, double-blind, multicenter, non inferiority clinical trial with combined glucosamine and chondroitin sulfate vs celecoxib for painful knee osteoarthritis // Osteoarthritis and cartilage. 2014. Vol. 22, Suppl. P. S7-S56.
- Martel-Pelletier J., Roubille C., Raynauld J.-P. et al. The long-term effects of SYSADOA treatment on knee osteoarthritis symptoms and progression of structural changes: participants from the osteoarthritis initiative progression cohort // Osteoarthritis and cartilage. 2013. Vol. 21. S249.
- Fransen M., Agaliotis M., Nairn L. et al. Glucosamine and chondroitin for knee osteoarthritis: a double-blind randomized placebo-controlled clinical trial evaluating single and combination regimens. Ann. Rheum. Dis. Vol. 74, No. 5. P. 851–858. DOI: 10.1136/annrheumdis-2013–203954.
- Glucosamine for osteoarthritis. Systematic review // Evidence-Based Healhcare & Public Health. 2005. No. 9. P. 322–331.
- Castellsague J., Riera-Guardia N., Calingaert B. et al. Individual NSAIDs and upper gastrointestinal complications: a systematic review and meta-analysis of observational studies (the SOS project) // Drug Saf. 2012. Vol. 12. R. 1127–1146.
- Tallarida RJ, Cowan A., Raffa RB Antinociceptive synergy, additivity, and subadditivity with combinations of oral glucosamine plus nonopioid analgesics in mice // J. Pharmacol. Exp. Ther. 2003. Vol. 307, No. 2. P. 699–704.
- Fairbank J., Mbaot JC, Davies JB, O`Brien JP The Oswestry Low Back Pain Disability Questionnaire // Physiotherapy. 1980. Vol. 66, N 8. P. 271–274.
- Christensen KD, Bucci LR Comparison of nutritional supplement effects on functional assessments of lower back patients measured by an objective computer-assisted tester // Second Symposium on Nutrition and Chiropractic. Davenport: Palmer College of Chiropractic, 1989, pp. 19–22.
- Gorislavets V. A. Structure-modifying therapy of neurological manifestations of spinal osteochondrosis // Consilium Medicum. 2010. No. 9. pp. 62–67.
- Shostak N. A., Pravdyuk N. G., Shvyreva N. M., Egorova V. A. Dorsopathies - approaches to diagnosis and treatment // Difficult patient. 2010. No. 11. pp. 22–25.
- Chernysheva T.V., Bagirova G.G. Two-year experience of using chondrolone for spinal osteochondrosis // Kazan Medical Journal. 2009. No. 3. pp. 347–354.
- Van Blitterswijk WJ, van de Nes JC, Wuisman PI Glucosamine and chondroitin sulfate supplementation to treat symptomatic disc degeneration: biochemical rationale and case report // BMC Complement Altern Med. 2003. Vol. 3. URL: https://www.biomedcentral.com/1472–6882/3/2 (access date: 03/11/2014).
- Mazurov V.I., Belyaeva I.B. The use of structum in the complex treatment of pain syndrome in the lower back // Therapeutic archive. 2004. No. 8. pp. 68–71.
- Manvelov L. S., Tyurnikov V. M. Lumbar pain (etiology, clinical picture, diagnosis and treatment) // Russian Medical Journal. 2009. No. 20. pp. 1290–1294.
- Vorobyova O. V. The role of the articular apparatus of the spine in the formation of chronic pain syndrome. Issues of therapy and prevention // Russian Medical Journal. 2010. No. 16. pp. 1008–1013.
- Chichasova N.V. Treatment of pain in patients with osteoarthritis of various localizations // Treating Doctor. 2014. No. 7. pp. 44–50.
T. L. Vizilo*, 1, Doctor of Medical Sciences, Professor A. D. Vizilo* M. V. Trubitsina** A. G. Chechenin*, Doctor of Medical Sciences, Professor E. A. Polukarova*, Candidate of Medical Sciences
* GBOU DPO "Novokuznetsk GIUV" Ministry of Health of the Russian Federation, Novokuznetsk ** GAUZ KO OKTs OSH, Novokuznetsk
1 Contact information
WHY US
- Experienced doctors. Treatment is carried out by spinal surgeons with extensive experience of successful work in Russia and abroad, doctors of medical sciences. World-renowned orthopedists, including doctors from Germany, Israel and other countries, advise at the Yauza Clinical Hospital.
- Diagnostics. High diagnostic accuracy is ensured by highly qualified doctors and the use of advanced equipment (Philips digital tomographs, which reduce radiation exposure and increase the accuracy of examination by 45-50%). The results of our radiation diagnostics are accepted in all clinics around the world.
- High tech. In the treatment process, doctors use the most modern and effective technologies, making the latest achievements of medical science available to our patients.
- Expert equipment. All interventions are performed in a high-tech operating unit, equipped according to the standards of the best European clinics (equipment from world leaders in the production of medical equipment - Karl Storz, DePuy Synthes, Joimax, Medtronic, Stryker, Zimmer).
- International standards. Treatment is carried out in strict compliance with medical protocols and meets the high requirements of world standards and the Ministry of Health of the Russian Federation.
- We value your time. At your service are the comfortable conditions of a premium-class hospital in the center of Moscow. The best specialists and technologies for getting rid of back pain without the need to travel abroad.
You can see prices for services