Nucleoplasty is a modern minimally invasive technique used in the surgical treatment of untreated herniated intervertebral discs. The essence of the innovative technology is to insert a puncture needle into the disc, at the end of which a cloud of cold plasma, laser energy or radio frequency waves is generated, due to which part of the nucleus pulposus is destroyed and the so-called “retracting effect” of the pathological displacement into the framework of the normal disc occurs. Thus, equalization of the proportions of fibrocartilaginous formation is achieved, and at the same time the release of the nerve roots from the irritating factor and the long-awaited disappearance of the pain syndrome.
Scheme of the procedure.
There are several types of surgical intervention, technically they are almost identical. However, what distinguishes them from each other is the main biological component of the effect on the gelatinous substance located inside the fibrous ring. In this connection, each of the tactics has its own name:
- cold plasma;
- laser;
- radiofrequency.
Their efficiency rate is about 80%. The operations are low-traumatic, bloodless, easily tolerated and are as safe as possible in terms of the development of postoperative complications. In addition, they are performed under local anesthesia, after which, as a rule, hospitalization of the patient is not required (not always), you can walk after 2 hours, and recovery takes from 2 to 4 weeks.
A set of instrumental needles for the procedure.
All of these advantages naturally increase interest in minimally invasive innovations. And we understand patients perfectly well, because no one wants to endure a more complex scalpel intervention, if today it is possible to eliminate pulpal displacement through a miniature puncture in a matter of minutes, without exposing the body to stress. But here the question is different: is this treatment suitable for you? Our article is dedicated to nucleoplasty and everything connected with it, in which you will find answers to this and other questions that interest you.
Statistics and description of nucleoplasty
At the moment, intervention using the cold plasma coblation method has become most widespread in clinical practice. This is the “youngest” technology among all its existing analogues, recognized in leading European countries (Czech Republic, Germany, etc.) and the USA. The number of such interventions performed worldwide is in the tens of thousands. So why is this particular method singled out among all possible analogues? It, as evidenced by reviews from many specialists, does not have an aggressive effect on the disc tissue and neighboring structures.
Thus, the process of disintegration of the gelatinous mass through plasma is not accompanied by such high temperatures as in other types, that is, the thermal field created in a series of intradiscal passages does not exceed 45-50 °C. Physical exposure to a laser and radio frequency electromagnetic field involves heating to approximately 60-67 degrees. Thus, there is no risk of burns to the fibers of the fibrous ring and neurovascular formations in the case of cold plasma.
Despite the increased popularity of c/p coblation, randomized studies show approximately the same results of effectiveness and complications for all tactics with a slight percentage gap. According to multicenter clinical observations, in 78%-80%, regardless of the chosen tactics, good or excellent results are noted; complications are quite rare (0.1%-0.4%). However, in approximately 18%-20% of patients who underwent vaporization, the treatment had no effect at all. The duration, technique (see video), anesthesia, and requirements for rehabilitation after surgery are the same for all types.
From here it is worth concluding that the final result is influenced not so much by the method of influence, but by the professionalism of the neurosurgeon and a competent differentiated approach regarding the advisability of using puncture decompression in each individual clinical case.
Experts warn that such treatment, even if successful, does not guarantee long-term preservation of the effect. Postoperative relapses occur in everyone at different times. In other words, you do not completely get rid of the pathology, but only temporarily make your life easier. The radiographic and symptomatic picture of the disease usually resumes approximately within 1-3 years (sometimes after six months), and only then again does the need arise for a similar session or a complete resection of the hernia formation. It is also worth considering that nucleoplasty will most likely be generally ineffective for large hernias.
Positioning of the patient during surgery.
This type of operation is performed in many countries and is not cheap. In advanced countries, it has been perfectly mastered and honed to the smallest detail, since it was introduced into clinical practice more than 15 years ago. In addition, in countries with highly developed medicine, doctors with a capital “D” practice, which significantly increases the chances of success. Therefore, many Russians more often choose Israel or some other foreign country that ranks high in spinal surgery and orthopedics. In Israel, the procedure will cost an average of 17-20 thousand dollars.
In Russia, Moscow began to provide the first services in 2011. In other Russian cities it will be even later. Today, therapy for intervertebral hernia using an innovative method can be performed not everywhere, but only in some large regional centers and metropolitan regions. For example, in Orekhovo-Zuevo, by the way, the cost of medical services there will be slightly lower. The price criterion depends on the location of the problem segment. It is highest if manipulations on the cervical spine are expected, and can reach up to 120 thousand rubles in medical centers of the Russian Federation. However, microinvasive surgery is recommended only for slight displacements of the nucleus pulposus - protrusions not exceeding 6 mm.
Recovery after endoscopic radiofrequency annulonucleoplasty
The postoperative wound (only 7 mm) does not require specific care; it is enough to change the antiseptic bandage once every 2-3 days. The suture is removed 10 days after annulonucleoplasty. Recovery after minimally invasive surgery is comfortable. The patient can return to normal activities the very next day after the intervention, however, we recommend abstaining from non-physical work for 1 week and from physical work for 1 month. Also, after 1 month, the patient comes for a follow-up examination with a neurosurgeon or at least keeps in touch with the attending physician to talk about the progress of recovery and his feelings. To avoid recurrence of a spinal hernia or protrusion, correction of motor habits is necessary. Daily walking of 3-4 km and swimming are recommended (1 month after annulonucleoplasty). Prolonged static load on the spine should be avoided.
Cold plasma type of nucleoplasty
This is one of the most modern types of puncture treatment of intervertebral discs; the lesion is localized using cold plasma. Since it is recognized as the most popular and promising, we will begin the description with it. Its goal is to eliminate painful discogenic syndrome due to partial evaporation of tissues of the nucleus pulposus with low-temperature ionized plasma (t≈50 ° C), which helps to reduce intradiscal pressure and, as a result, eliminate compression of the nerve root and spinal cord. Numerous patient reviews show that the cessation of pain occurs within the first hours after the end of the session. However, out of approximately 100 people undergoing surgery, 10-15 people feel better by the end of 1-2 weeks.
Quite rare honey for Russia. The service is paid, the cost ranges from 35,000-120,000 rubles. Estimated prices for the Moscow region: restoration of the cervical spine (1 element) – from 67,000 rubles. and above, lumbar – 35-67 thousand rubles. Plus, you need to add to any amount an examination by a neurosurgeon (about 4-5 thousand rubles), preoperative diagnostics (from 6 thousand rubles), hospital stay (1 day - from 5 thousand rubles).
Informative! Another name for the method is coblation, which literally means “cold destruction.” A method that uses cold plasma was introduced into medical practice in 1995. Its founders were American specialists, who performed the world's first operations of this type using a HP generator from ArthroCare (USA). The method has entered European practice on a large scale since 2000.
The technology in question is a percutaneous procedure, which means there will be no incisions. To enable corrective manipulations, only a local micropuncture will be made. The progress of the process will be monitored by an electron-optical converter in the near-X-ray spectrum. In addition to the image intensifier, the operating equipment of the operating surgeon includes:
- neurosurgical generator that produces cold plasma;
- working bipolar electrode emitting ionized low-temperature plasma flow;
- a thin spinal needle for approaching the problem object and inserting an electrode into it.
Operating field.
A non-traumatic session is performed on an outpatient basis under local (regional) anesthesia. Sometimes, as evidenced by patient reviews, an additional sedative is administered intravenously to put the person into a state of medicated sleep. Therapeutic measures are almost painless and fairly quick: the coblation process itself lasts 1-2 minutes, but in total all preoperative and intraoperative actions take from 15 to 25 minutes. Restoring the shape of intervertebral discs using gas-discharge plasma is implemented according to the scenario below.
- If treatment is planned in the lumbar segment, the patient's position is lying on his stomach; a posterolateral approach is used to perform manipulations.
- If it is necessary to restore an element located in the cervical spine, the person lies on his back, with his head slightly tilted back, using the anterolateral approach technique.
- Next, anesthesia and antiseptic treatment of the skin are performed. Then, under visual image intensifier control, a 2-3 mm conductor needle is clearly inserted into the central part of the disc.
- When the needle is in the right place, an electrode (diameter 1.1 mm) is carefully inserted into it so as not to disturb the point of its active contact. Then the electrode is connected to the main device, that is, the x/plasma generator.
- A thin, narrowly focused cloud of cold plasma is formed around the working end of the electrode, which will evaporate the disc from the inside due to the physical dissociation of the molecules that make up the biological tissue of the cartilage.
- The neurosurgeon performs certain rotational-translational movements with the electrode, creating several (2-6 pieces) diverging passages in the nucleus, due to which the volume of the gelatinous mass decreases and the intervertebral layer returns to its normal state. Each area is processed for 5-10 seconds.
- At the end, all surgical instruments are carefully removed, and a sterile plaster is applied to the miniature wound. Sutures are usually not necessary.
The patient is activated 2-3 hours after the intervention; in the initial period, cold dry (!) compresses are applied locally and antibiotic therapy is prescribed. Calm walking is allowed, physical activity is limited, but special exercise therapy is required. You can perform simple household activities, but you should completely eliminate heavy lifting and not overload the operated area. During the rehabilitation period, wearing an orthopedic bandage for the lower back or neck is recommended. After 2 months, physiotherapy procedures are necessarily recommended to consolidate the result and exclude the development of possible long-term consequences.
Such medical care is not available in every city. Take the city of Vladivostok, for example, cold plasma is not used for treatment in any medical institution. Therefore, some residents of the Russian Federation are forced to go to clinics in Moscow, St. Petersburg, etc. However, many citizens do not consider the services of domestic doctors, preferring to be treated by proven, reliable neurosurgeons from foreign countries.
Thanks to their high professionalism and impeccable reputation for more than 10 years, Czech neurosurgeons have maintained a leading position in demand both within their republic and abroad. Czech specialists Artusmed are highly specialized in spinal neurosurgery, orthopedics, traumatology, and rehabilitation of the musculoskeletal system. The honorable state is in no way behind Germany or Israel in the development of these areas of medicine, and therefore stands on the same level with them. In the Czech Republic, aggressive orthopedic techniques are not used in the surgical treatment of the spinal system; exclusively new high-tech operations with minimal invasiveness have long been used here, and most importantly, they are performed with high precision down to the millimeter, which guarantees the safety of the anatomical structures of the spine and does not threaten human life.
Key facts: endoscopic nucleoplasty
- Indications:
Painful protrusion of the intervertebral disc - Strategy:
Through a minimal incision, a small expanding coil is directed to the damaged intervertebral disc, which rotates to remove part of the herniated disc that is putting pressure on the nerve. - Hospital stay:
3 days - Rehabilitation treatment:
14 days outpatient - Recommended time to fly home:
14 days after surgery - Showering:
1 day after surgery - Duration of disability:
1 week - Bibliography:
Endoscopic nucleoplasty using radiofrequency irradiation - Literature
medical request
Price for nucleoplasty: costs in Russia, Moscow and abroad
Most hospitals where nucleoplasty is performed are concentrated in Moscow (price in the table) and St. Petersburg. Let's just say that such operations are not common on Russian territory, so finding in any other locality, except for regional and regional centers, and even then not all, a medical institution that has laser, radio frequency vaporization or plasma coblation in its range of services, is very problematic .
But let's get straight to prices, jumping ahead a little, because the issue of cost is no less important for you. And then we will highlight the indications, contraindications, characterize all the remaining methods and list the possible consequences. So, we bring to your attention an overview of approximate prices within the Russian state (St. Petersburg, Moscow) and leading foreign countries.
| Nucleoplasty method | Russia (in rubles) | Czech Republic (in euros) | Israel (in $) | Germany (in euros) | |
| Moscow | Saint Petersburg | ||||
| Cold plasma coblation | from 35000 to 120000 | from 47500 to 110000 | 2500-3000 | 12000-20000 | from 6000 |
| Laser treatment (vaporization) | 42000-55000 | 41300-50000 | up to 3000 | 13000 | 5500-7000 |
| Radiofrequency (RF) destruction | from 22000 | from 20000 | 1500-2000 | 5000 | 5200 |
Advantages of endoscopic radiofrequency annulonucleoplasty at the Pirogov Clinic
- Technological equipment of the clinic with modern endoscopic, radiofrequency, and X-ray equipment;
- Spinal surgeries and minimally invasive interventions are performed by a leading neurosurgeon with more than 10 years of experience, Candidate of Medical Sciences. Sciences Amir Muratovich Mereji;
- Availability of our own laboratory and highly specialized doctors in one place;
- The opportunity to consult with a doctor in absentia on MRI images and complaints and get a “second opinion” from a neurosurgeon on your diagnosis (free of charge).
- Affordable prices for operations for spinal hernias, protrusions and stenoses, the possibility of obtaining a loan or interest-free installment plan in the clinic;
- We do not perform spinal surgeries under a quota, since we are a private clinic, but we can provide services under VHI policies.
To undergo spinal surgery at the Pirogov Clinic means to make a choice in favor of high standards of diagnosis, effective treatment and quick recovery!
Make an appointment
Indications and contraindications for nucleoplasty for intervertebral hernia
Vaporizing the intervertebral disc tissue, taking into account the reviews, can help a lot. However, you need to know that gentle tactics are not without contraindications. This suggests that not everyone will be able to alleviate their suffering associated with a hernial protrusion through all known percutaneous decompression options. There are a number of conditions when percutaneous decompressive surgery is indicated and contraindicated. By neglecting them, hernias of the cervical spine or other localization will not decrease, pain will not regress, and the risks of consequences will only increase significantly. Therefore, the principle of clinical and morphological compliance and non-compliance of degenerative-dystrophic changes with existing recommendations and restrictions is important here.
Indications for such surgery are:
- insignificant sizes of protrusion - up to 6 mm inclusive (only with a “fresh” degenerative process can it really be improved the condition of the fibrocartilaginous unit, that is, when the hydration and elasticity properties of functional tissues are not critically impaired);
- local and/or pain radiating to the limbs of moderate intensity, which does not respond well to standard painkillers from the NSAID category;
- the absolute ineffectiveness of a well-conducted course of conservative treatment in combination with physical therapy for 3-6 weeks.
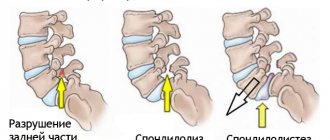
It is strictly contraindicated to resort to the procedure if at least one of the following problems is diagnosed:
- sequestered hernia;
- large hernial protrusion – 7 mm or more;
- loss of integrity of the annulus fibrosus;
- reduction of the height between the vertebral bodies by half or more;
- combined stenosis of the spinal canal;
- adhesions in the area of the spinal root cuff;
- compression of the spinal canal by bone structures;
- infectious and inflammatory processes within the operated area;
- all kinds of active infections in the body and chronic pathologies in the acute phase;
- neoplasms at any level of the spine and spinal cord (with a vertebral hemangioma combined with a hernia on the same segment, you need to look for a good neurosurgeon to resolve the difficult situation);
- spinal cord injury, paralysis, paresis of the upper or lower extremities;
- dysfunction of the pelvic and intestinal organs due to a complicated form of the disease (in this case, a full microdiscectomy is urgently required!).
In such advanced cases, nucleoplasty is not performed.
When studying the reviews and advantages of the technique, you should clearly understand that nucleoplasty is not a panacea and not a universal tactic that is equally suitable for all patients. Yes, it helps to reduce intradiscal pressure and thereby reduces painful neurological symptoms, but only if the pathology is uncomplicated and in the absence of ruptures of the fibrous ring. In addition, one should take into account the fact that protrusion, even minor, in patients over 50 years of age, as clinical observations indicate, most often does not retract back when the appropriate conditions are created, since the elasticity of cartilaginous tissue is greatly reduced in this age period.
In advanced forms, a mini-operation based on a thermal effect will not replace a normal operation and will not help achieve the desired result. Unfortunately, the specificity of pathomorphological changes in fibrocartilaginous structures is irreversible. And if it is not possible to conservatively stop or significantly slow down their progression in time, completely complete cutting off of the hernia using microdiscectomy or endoscopic ectomy can save you from pathological signs and dangerous consequences.
Important! Percutaneous puncture manipulations are undoubtedly valuable inventions in modern surgical heliology, having an impressive evidence base of effectiveness. But there will be zero benefit from them if diagnostic data contradict established recommendations.
Biaculoplasty
Puncture needles are inserted into the side of the spine on both sides.
A radiofrequency current of moderate temperature is conducted between two straight electrodes along the posterior ring of the disc. Biaculoplasty is aimed primarily at denervation of pain conductors. Due to its gentle effects, the technique has proven itself in the treatment of chronic pain in the spine. However, it also has significant disadvantages: there is no endoscopic visual control, a higher probability of recurrent hernia or protrusion, and the need to insert two puncture needles. Also, this technique may not be suitable for patients who experience multiple degenerative changes at different levels of the spine. Thus, endoscopic radiofrequency annulonucleoplasty shows the best result in comparison with other types of minimally invasive puncture interventions: cold plasma nucleoplasty, laser vaporization (laser hernia removal, laser thermodisplasty, laser disc reconstruction), biaculoplasty.
Long term results
As we previously indicated, based on qualified reviews and statistics from clinical studies, the effectiveness of hernia vaporization is 80%. A successful outcome is influenced by the strict selection of patients with the appropriate diagnosis and the technical impeccability of surgical procedures. People who have had herniated discs removed according to all the rules post reviews with approximately the following content:
- the operation is practically painless, the anesthesia is gentle but effective, however, many feel slight discomfort in the operated area during the session;
- pain that had been tormenting for a long time before the intervention disappeared immediately or within a month after it;
- a short-term increase in pain on days 2-3, but over time it began to regress;
- rapid recovery with a minimum of restrictions regarding daily physical activity;
- Many returned to work, if it did not involve intense physical labor, almost immediately, without even filing a sick leave;
- the cost of one highly productive procedure is not much more than the money spent on conservative treatment, which was ineffective or ineffective.
Since up to 20% of those operated on do not feel the effect after undergoing puncture decompression, it is impossible not to note the reason for the failures. Unfortunately, unsuccessful treatment is most often the price of our naivety and ignorance of medical issues.
Looking through the patient forum, it is extremely outrageous that surgery is allowed in the presence of obvious contraindications. Namely, when diagnostic images clearly indicate the need for more radical intervention. Disorder, no offense intended, is typical of private medical centers in Russia and Ukraine, where such assistance is offered unreasonably often.
Moreover, in domestic medical institutions, due to scant professional experience, unforgivable mistakes are often made during an important mini-surgical session, and the patient pays for them with his own health. Fortunately, we have conscientious and highly specialized clinics, but there are only a few of them. Abroad, in the leading countries of medical tourism, in general, complete order reigns. Therefore, it makes sense to think about it and approach very scrupulously the choice of a medical institution where they will help you, albeit not with such a lightweight type of surgery (if the indications do not allow it), but rightly and for good reason.
Attention! Pain in the spine, paresthesia and pain in the legs and arms are symptoms inherent in many diseases. And it is not a fact that it is a protrusion or disc herniation that creates discomfort. Therefore, in order to accurately establish the cause of painful symptoms and competently develop a treatment program, a high-quality comprehensive diagnosis of the musculoskeletal system and the body is of utmost importance. Get it done in good clinics!
How effective is endoscopic radiofrequency annulonucleoplasty?
Endoscopic radiofrequency annulonucleoplasty shows excellent clinical results and in practice is more effective than most previously known minimally invasive puncture interventions aimed at treating protrusion and removing spinal hernia. In 90% of cases, this interventional treatment method allows for complete recovery.
Endoscopic radiofrequency annulonucleoplasty is used as the most effective alternative to such interventions as:
Laser type of nucleoplasty
Laser destruction of intervertebral discs was created back in the 80s of the 20th century by European scientific experts in the field of neurosurgery of the spinal column. The outdated method today has practically lost its relevance, as new, more improved percutaneous methods of decompression have appeared. The impact on the biological tissue of the shock-absorbing pad between the two bodies of adjacent vertebrae is carried out by pulses of laser radiation. Therapy takes 20 to 30 minutes.
Laser radiation causes the formation of a vaporization effect in the gelatinous substance and compression of the intervertebral structures. As a result of the created thermal collapse, intradiscal pressure is reduced, the size of the hernia is reduced and, thus, the irritating factor that excites the sensitive nerve endings that stimulated pain is eliminated. The procedure is performed as follows:
- under regional anesthesia, using fluorographic x-ray control, a thin hollow cannula-needle is installed into the disc through a small puncture (posterolateral access);
- after the needle reaches a given point (the center of the core), a quartz light guide is inserted into it, which emits laser energy, accompanied by internal thermal ablation (t≈70 °C);
- as a result of pulsed laser energy, liquid evaporates in the impact zone, which ensures a 30% reduction in pressure inside the disk element;
- Thanks to the so-called denucleation, the displaced part of the nucleus pulposus, together with the fibrous ring, is retracted back over time, and radicular pain ceases to bother.
You've probably read reviews that functional laser decompression has a strong thermal effect. What is not good. This is true; there is a risk of burning nearby structures and disrupting their normal morphology and unity. But again, such an unfavorable outcome is possible if errors are made in the introduction and fixation of the working instrument in the desired area, in controlling the temperature and time of exposure of the radiating flow to soft tissues.
Therefore, this approach, like any related technique, implemented unskillfully and not in accordance with technological principles, of course, is fraught with consequences. However, even with ideally done laser correction, no specialist will give you one hundred percent guarantees that the effect will last long. According to statistics, in approximately 17% of patients, the pathology in the same place recurs within 6 months after successful treatment.
Advantages of intervertebral disc nucleoplasty
Undergoing this procedure at the AXIS clinic has a number of undoubted advantages:
- the procedure is minimally invasive, done on an outpatient basis and does not require extensive surgical intervention;
- does not leave adhesions in the spinal canal, does not damage bone tissue;
- local anesthesia is used;
- absence of complications that may arise as a result of open surgery;
- no hospitalization required: patients return home the same day;
- short duration;
- there is no blood loss;
- after the procedure there is almost no pain;
- fast recovery time.
It is important to note that at the AXIS clinic, cold plasma nucleoplasty of intervertebral discs is performed under the control of high-precision X-ray equipment, which allows one to monitor what is happening in the spine in real time.
The concept of radiofrequency nucleoplasty
The mechanism of radiofrequency treatment of the spinal disc is identical to the methods described above. The therapeutic effect (compression) is also similar. Therefore, we will not go into too much detail about the specifics of this type of minimally invasive intervention. The essence of this therapy is the use of UHF currents, that is, a high-frequency electromagnetic field will act on the degenerated component. UHF radiation causes internal heating (t≈60 °C) of a selected area of the nucleus, which turns the liquid contents of the cartilage into steam, which is safely removed through a special compartment of the working probe.
This approach is considered more gentle and temperature-controlled than laser vaporization, but is noticeably inferior to cold plasma coblation. According to foreign authors, the high-frequency therapeutic principle allows you to repeat sessions on the same problem segment up to 2 times a year if radicular pain returns again, while the likelihood of developing negative phenomena is minimal. Repeated laser therapy is very undesirable, since extremely unfavorable reactions may follow, for example, a burn of the fibrous ring with its further rupture and prolapse of the nucleus pulposus into the spinal canal.
Operation
Before cold plasma nucleoplasty begins, the patient is given local anesthesia, X-ray equipment is installed, which allows the movements of the instruments to be monitored in the smallest detail, in frontal and lateral projections. Then a special puncture needle is inserted through a puncture in the skin. It is placed in the cavity of the intervertebral disc.
An electrode is passed through the needle to the protruding fragment of the nucleus pulposus. Several passes are made sequentially. Inside the disc, they form branched passages (voids), reducing the volume of the nucleus pulposus. The whole procedure lasts 20-30 minutes.
Puncture nucleoplasty
Puncture decompressive tactics for the treatment of intervertebral hernias can have complications, fortunately, in rare cases. Despite the fact that the procedure is characterized by extremely minimal invasion into the human biological system, it is performed on the most complex and vital part of the musculoskeletal system, which contains the main organ of the central nervous system - the spinal cord. Moreover, a nucleoplastic session is a type of spinal surgery, so it should be treated as a serious operation, and not as a simple non-surgical tactic.
Rehabilitation
Patients may require one day of bed rest. The patient can return to the usual rhythm of life after 1-6 weeks. However, do not forget that nucleoplasty is only the first step towards a long-term result. The recovery period, including pain relief, is gradual and can last 8-12 weeks.
A comprehensive rehabilitation program will be needed to achieve a more successful treatment outcome. Physical activity should be monitored and increased gradually. Treat the condition of the spine with special attention - this has been necessary at all times and is necessary now. Strengthening the muscles that support the spinal column is especially important.
medical request
Complications
Any rude and careless actions of a neurosurgeon, non-compliance with intra- and postoperative standards, poor preparation of the patient, lack of proper postoperative rehabilitation - all this can most likely lead to complications. We invite you to familiarize yourself with which ones:
- local infectious process (discitis, purulent focus);
- allergic reaction to anesthesia;
- damage to nervous and vascular formations, nearby internal organs;
- long-lasting hematomas and swelling;
- reflex mediator pain;
- pronounced pain syndrome, manifested by a strong burning sensation when changing posture, during stressful situations and nervous excitability;
- sharp progression of pathology due to burn or mechanical damage to the fibers of the fibrous ring with subsequent rupture.
To be sure that the medical procedure will be successful and will not entail a cascade of unpleasant complications, contact only professional clinical medical-surgical centers that directly specialize in the field of orthopedics and neurosurgery. Cold plasma nucleoplasty, spinal arthroplasty, endoscopic discectomy, microdiscectomy and many other techniques are superbly mastered and perfected in the Czech Republic. The increased demand for treatment of intervertebral hernias in clinics in the Czech Republic is explained by the most reasonable prices with exceptional quality of any procedure and the absence of side effects. At the same time, the treatment program, which is extremely important, always includes rehabilitation. Prices in the Czech Republic are at least 2 times lower than anywhere else abroad.
3.Advantages and disadvantages
No blood loss or scarring, no need for long-term hospitalization and general anesthesia; minimal risk of intra- and postoperative complications; the ability to perform plastic surgery on several discs in one procedure; preservation of the natural mechanics of the spine (the body of the disc remains in place, the operation is performed only on the core) - all this is one of the undeniable advantages of nucleoplasty.
Flaws
Any methodological type of nucleoplasty requires the most thorough laboratory and instrumental (primarily MRI) examination of the patient, highly qualified surgical team and first-class equipment in the clinic, taking into account all individual factors (there are a number of contraindications). Failure to comply with these basic conditions most often leads to complications and therapeutic failures (or to partial success where it could have been complete). Complications themselves, such as infection of the disc or aseptic inflammation, damage to blood vessels or conductive nerves, are very rare; the bulk of the “unsuccessful” 20% are precisely cases of unresolved or incompletely resolved clinical problems.
About our clinic Chistye Prudy metro station Medintercom page!