Are you experiencing back pain and numbness in your limbs? These are the first signs of osteochondrosis. Insufficient mobility in lifestyle, sedentary work, stress on the neck and spine lead to cartilage wearing out, losing moisture, resulting in micro-tears.
With cervical osteochondrosis, degenerative changes occur in the intervertebral discs. Not only the discs are damaged, but also the vertebrae and joints in the cervical region. If the disease is not treated for a long time, the patient’s general well-being worsens: constant headaches, the appearance of a vertebral hernia, deterioration of cerebral circulation, as a result of which cognitive functions decrease.
Reasons for the development of osteochondrosis
An incorrect sitting position, in which the neck is pulled forward, leads to the development of cervical disease. In this case, excessive pressure occurs on the intervertebral discs, which leads to changes in the nuclei pulposus and compression of blood vessels. This is the position a person takes at a workplace in front of a computer. Therefore, office workers are most often exposed to the development of osteochondrosis of the cervical spine.
In addition, the reasons for the development of pathology may be:
- improper load distribution when carrying bags;
- excessively soft sleeping place (the spine bends in an unnatural shape);
- genetic predisposition;
- lack of vitamins and microelements in the diet;
- endocrine system disorders;
- curvature of the spine and poor posture during active growth of the body;
- cervical vertebrae injuries;
- presence of bad habits.
Does osteochondrosis cause spasm and tightness in the throat?
Constant constriction in the throat with osteochondrosis is a consequence of impaired innervation of soft tissues. They can react to this with changes in trophism, atrophic processes and a decrease in the tone of the muscle wall.
Very often, osteochondrosis causes throat spasm at the humoral (cellular) level. This happens as follows:
- a decrease in the height of the intervertebral disc and the proliferation of osteophytes entail compression of the radicular nerves, their branches and the cervical plexus;
- static tension of the muscle fiber develops as a compensatory reaction;
- it blocks microcirculation of blood and lymphatic fluid;
- stagnation and effusion of fluid into the intercellular space are provoked;
- swelling of soft tissues (subcutaneous fatty tissue) develops;
- it begins to put pressure on the structures of the throat;
- this condition often develops into true laryngeal edema, which can cause serious breathing problems.
If you experience a feeling of tightness in the throat area, you should seek medical help as soon as possible. It is important to make an accurate diagnosis and carry out the correct treatment. This way you can avoid the development of dangerous complications of cervical and thoracic osteochondrosis.
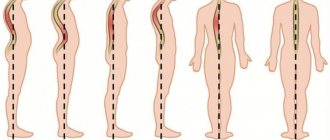
Stages of the disease
Determining whether your pain symptoms are signs of the development of cervical osteochondrosis and what stage of development of the disease can only be determined by an experienced doctor after examination and palpation. In total, cervical osteochondrosis goes through four stages of development:
- The nucleus pulposus, the central part of the intervertebral disc, undergoes moderate dehydration during the first stage. As a result, the supporting and shock-absorbing functions of the intervertebral discs are gradually lost. During the first stage, you will experience pain with sudden movements, hypothermia, and staying in one position for a long time.
- The second stage of development is characterized by the appearance of congestion and spasms, which compress capillaries and blood vessels, preventing normal blood circulation. As a result, the frame of the intervertebral disc becomes thinner, forming a protrusion (bulging forward or backward). Under the influence of excessive load, osteophytes are formed on the cervical vertebrae - bone growths. Pain sensations are localized in one place; with sudden turns and tilts of the head, dislocations of the cervical vertebrae can occur.
- Extrusions are formed as a result of thinning of the intervertebral discs. The edge of the nucleus pulposus breaks the fibrous ring and extends beyond the edges of the vertebral body. Muscles and nerve endings are compressed. Pain is felt in the neck, back and limbs.
- At the fourth stage of the disease, the intervertebral discs are displaced and central and lateral hernias form. In addition, scars form on the discs, which leads to immobility of the affected joint. The patient experiences persistent back pain that radiates to other parts of the body, a constant feeling of fatigue, and asymmetry of parts of the body occurs.
Symptoms of cervical osteochondrosis
Symptoms of osteochondrosis of the cervical spine manifest themselves differently depending on the stage of development of the pathology. In the early stages it can occur with virtually no symptoms. Pain in the neck and back can only appear if you stay in one position for a long time, sharply bend or turn.
At later stages of development, a crunching sound is heard in the spine, back pain radiates to other limbs, and numbness occurs in parts of the body. When osteophytes and extrusions form, the following occurs:
- headaches in the back of the head and parietal part;
- speech disorders and numbness of the tongue;
- decreased sensitivity of the skin of the neck;
- breathing disorders;
- changes in blood pressure;
- heartbeat disturbances;
- noise and congestion in the ears;
- fainting.
Symptoms of osteochondrosis of the cervical spine in women are much more pronounced than in men. This is due to the fact that women have a predisposition to vascular diseases and a more fragile structure of the bone segments of the spine. Signs of the disease begin to appear when intervertebral discs change. This leads to disruption of normal blood circulation and causes severe headaches, dizziness, and neuroses. An exacerbation of the disease in women often occurs during menopause, when the body is subject to hormonal changes.
The symptoms of cervical osteochondrosis in men are similar to those in women; erectile dysfunction can be observed separately.
Headache with cervical osteochondrosis is caused by poor circulation in the brain and spinal cord. When the vertebrae become misaligned, they compress the arteries and the oxygen content in the blood decreases. Unfortunately, such pain may not go away even after taking strong painkillers. Therefore, it is important to approach solving the problem comprehensively. Dizziness with cervical osteochondrosis may be accompanied by darkening of the eyes and the appearance of tinnitus. This happens because spasming muscles cause a reduction in oxygen supply to the brain.
A lump in the throat with osteochondrosis of the cervical spine, as well as burning, difficulty breathing and muscle spasms are a common occurrence. The disease provokes compression of the nerve fibers of the cervical spine to the head and neck. Disturbances in nerve impulses cause sore throat.
Due to spasms of blood vessels and irritation of nerve endings, jumps in blood pressure occur. Increased lower pressure in osteochondrosis indicates that the blood supply to certain areas of the brain is impaired, since the vertebral artery is compressed by the intervertebral discs. As a result, oxygen starvation occurs and blood pressure rises.
Sore throat: possible causes, diagnosis and treatment
Sore throat is a common complaint of patients when visiting an otolaryngologist, therapist, pediatrician and general practitioner. The causes of sore throat can be infectious and inflammatory diseases of bacterial and viral etiology, inflammatory processes in the pharynx, larynx and surrounding organs caused by non-infectious factors, and non-infectious pathology (
). Before proceeding with pharyngoscopy, it is necessary to carefully detail the patient’s complaints and collect an anamnesis. The patient can call a sore throat the unpleasant sensations of scratching, burning, soreness, rawness, the feeling of a “foreign body,” the intensity of which is conveniently assessed on a 10-point scale, where the maximum manifestation of pain is rated at 10 points, the minimum at 1 point.
It is important to determine what, in the patient’s opinion, preceded the onset of pain and what other symptoms it is accompanied by. If there is hyperthermia, then the inflammatory nature of the disease is most likely: pharyngitis, tonsillitis (tonsillitis) [16]. Refusal of food and water can provoke severe pain in aphthous stomatitis (Fig. 2), tonsillitis of the lingual tonsil, paratonsillar and retropharyngeal abscess, Ludwig's angina (phlegmon of the floor of the mouth). With these diseases, drooling is possible, and inflammation of the paramygdaloid tissue and tissues of the floor of the mouth leads to trismus of the masticatory muscles (inability to open the mouth), a forced position of the head tilted to the painful side.
The occurrence of such a condition requires immediate contact with a medical specialist to sanitize the area of inflammation. Epiglottitis, an inflammation of the epiglottis caused by Haemophilus influenzae (more common in young children), gives similar symptoms. Along with refusal to eat, salivation, pain and hyperthermic symptoms, epiglottitis is accompanied by voice disturbance (it becomes dull, hoarse) and difficulty breathing. There is a forced position of the patient in a sniffing position, as if holding porridge in the mouth, the mouth opens freely, but a rough examination of the pharynx with a spatula can lead to laryngospasm and death. Therefore, with the above symptoms, pharyngoscopy is performed carefully; during it, you can see a hyperemic, edematous epiglottis behind the root of the tongue.
Other causes of sore throat accompanied by sore throat and cough can be in children and young people: drainage of discharge from the nasopharynx due to adenoiditis or sinusitis; irritation of the respiratory tract by dry air, smoke, including active and passive smoking; childhood infectious diseases [9]. In adults, a common cause of such complaints, often with a feeling of a lump in the throat, a “foreign body,” is an exacerbation of chronic pharyngitis associated with pathology of the gastrointestinal tract: gastritis, esophagitis, gastroesophageal reflux, cholecystitis, gastric ulcer. Severe dysphagia, regurgitation and pain when swallowing can be caused by esophageal varices [14].
A carefully collected anamnesis allows us to find out the dynamics of complaints, the time of their appearance, the connection with a previous injury or medical examination (gastroscopy), foreign body entry, contact with an infectious patient, hypothermia (drinking cold beer, ice cream), occupational or household hazards (irritants, dust , hot air, taking concentrated solutions of vinegar, spices, medications: corticosteroids, antibiotics, diuretics, local decongestants and others). Sore throat can occur as a manifestation of sexually transmitted diseases: gonococcal pharyngitis, syphilis, chlamydia of the respiratory tract. Infection with the human immunodeficiency virus contributes to the formation of inflammatory viral, tumor and mycotic lesions of the mucous membranes [3].
Chronic pathology of the kidneys, endocrine system, blood, previous radiation and chemotherapy can lead to the formation of a chronic inflammatory and atrophic process in the pharynx. The first manifestation of hyperglycemia [5] may be thirst and dry mouth, accompanied by catarrhal changes in the pharynx. Similar complaints occur with Itsenko–Cushing syndrome [5]. In patients with hypothyroidism, swallowing is often impaired, speech becomes slurred due to swelling and dryness of the tongue and lips, and it is difficult to perform pharyngoscopy.
Non-infectious pathology of the organs of the neck and chest cavity - angina pectoris, myocardial infarction - can manifest itself as intense pain in the pharynx and behind the sternum. Long-lasting dysphagia and unpleasant sensations in the form of a lump or foreign body in the throat, which are not amenable to anti-inflammatory therapy, can cause [14] tumors of the larynx, laryngopharynx, thyroid gland, and pharyngoesophageal (Zencker) diverticula. Many days of fasting, dieting, dyspepsia and heavy menstruation lead to a deficiency of vitamins and minerals. Vitamin A deficiency [5] causes dryness and erosion of the mucous membranes.
Vitamin B2 deficiency produces a triad of symptoms: dermatitis, cheilitis and glossitis (bright red, smooth and shiny dry tongue), accompanied by burning and pain in the mouth when talking and eating. Vitamin C hypovitaminosis occurs with dietary deficiency of ascorbic acid, inflammatory processes in the intestines and is manifested by pain, hemorrhagic and ulcerative-necrotic manifestations in the oral cavity and in the area of the palatine tonsils, mobility and tooth loss. Similar changes in the oral cavity and pharynx give rise to blood diseases (leukemia). Against the background of iron loss (with hyperpolymenorrhea), Plammer-Vinson syndrome is formed, characterized by superficial glossitis, dysphagia, cracks in the corners of the mouth, nail dystrophy, seborrheic dermatitis of the face, blepharitis, conjunctivitis, and decreased vision at dusk. B12 deficiency anemia associated with impaired absorption of this vitamin in the stomach due to anacid gastritis, tapeworm infestation, or increased consumption in pregnant women, manifested by Möller-Gunter glossitis (bright red tongue with smoothed papillae) and atrophy of the pharyngeal mucosa, burning pain in the tongue, weakness, crawling sensation in the limbs. A blood test reveals macrocytes, megalocytes, hyperchromic anemia, leukopenia.
Diseases of the spine [2] (cervical osteochondrosis, tuberculous spondylitis, radiculitis) can cause pain in the pharynx. Neuralgia of the glossopharyngeal nerve manifests itself as intense pain in the pharynx, especially against the background of chronic stress in anxious and suspicious patients. Metabolic disorders, intoxication, and trauma contribute to its occurrence. Characterized by unilateral pain in the root of the tongue, tonsil, lasting several minutes, accompanied by dry throat and subsequent hypersalivation. The therapeutic effect is achieved by lubricating the root of the tongue and pharynx with local anesthetics. Neuralgia of the superior laryngeal nerve [1, 6] gives similar symptoms, but also includes a painful dry cough and spasm of the vocal folds during inspiration [6].
Pain in the pharynx can be caused by an odontogenic process: periodontitis, teething pathology, galvanism [4, 17]. Rarely, unilateral pain in the pharynx occurs, the cause of which is the long styloid process (Eagle syndrome), accessible to palpation in the area of the palatine tonsil [15].
Rare causes of pain in the pharynx are ulcerations on the mucous membrane of tuberculous etiology [14]. In this case, there is a prolonged cough, weight loss, and swollen lymph nodes.
A final diagnosis is possible based on oropharyngoscopy. The main differential diagnosis for pain in the pharynx is between its most common causes - acute (or exacerbation of chronic) pharyngitis and sore throats caused by streptococcal infection (group A beta-hemolytic streptococcus - GABHS).
Acute pharyngitis is a viral infection of the pharynx in 90% of cases. Its main symptoms are: increased body temperature, sore throat when the throat is empty, when eating, soreness and a dry cough that does not bring relief. Patients indicate the localization of unpleasant sensations on the back wall of the pharynx. In the pharynx (Fig. 3), hyperemia of all parts is detected: the posterior wall, arches, tonsils, and there may be vesicular rashes (herpes, enterovirus). Plaques are not typical, there is often a runny nose and other catarrhal phenomena - nasal congestion, sneezing. If a rash is detected on the skin and mucous membranes, it is necessary to exclude an infectious disease - measles, scarlet fever, rubella [8]. Adenoviral infection manifests itself in the form of conjunctivitis, enlarged lymph nodes, fever, runny nose, and there may be plaque in the throat.
The disease progresses in waves: on the 7th–10th day of illness, a repeated increase in body temperature and a return of symptoms are possible. Enterovirus infection (“summer flu”) manifests itself in the form of dyspeptic, myalgic, and meningeal syndromes. Pharyngoscopy reveals bubbles on the mucous membrane of the oropharynx. In making the diagnosis of viral pharyngitis, the following help: knowledge of the epidemiological situation, dynamic observation of the patient, a variety of clinical manifestations (abdominal pain, vomiting, eye damage, meningeal symptoms, myalgia), lymphocytosis in the blood with normal ESR, lack of effect from antibacterial therapy, serological data research, polymerase chain reaction and others.
Sore throat is a general infectious disease with local manifestations in the form of acute inflammation of one or more components of the lymphadenoid pharyngeal ring, most often the palatine tonsils (tonsillitis), pharyngeal tonsil (adenoiditis), lingual tonsil, lateral ridges of the pharynx and larynx.
The classification of acute tonsillitis (according to I.B. Soldatov, 1975) involves the division into primary tonsillitis: catarrhal, lacunar, follicular, ulcerative-membranous; and secondary: for acute infectious diseases (diphtheria, scarlet fever, measles, tularemia, typhoid fever, infectious mononucleosis) and diseases of the blood system (agranulocytosis, alimentary-toxic aleukia, leukemia). There are special forms of tonsillitis [10]: viral, fungal, syphilitic.
With catarrhal tonsillitis, there is hyperemia and enlargement of the palatine tonsils, regional lymphadenitis, no plaque, a blood test shows slight leukocytosis, increased ESR. Catarrhal sore throat often has to be differentiated from viral pharyngitis, in which there is a cough, there may be a runny nose, and there is no enlargement or tenderness of the lymph nodes.
Follicular tonsillitis is manifested by bright hyperemia and swelling of the tonsils, subepithelial rounded yellowish elevations (follicles).
With lacunar tonsillitis, white-yellow plaques appear at the mouths of the lacunae of the tonsils (Fig. 4), which can merge with each other and cover the entire surface without going beyond the tonsils, being removed without leaving a bleeding surface, rubbing between two spatulas, dissolving in the vessel with water.
It is important to determine the streptococcal etiology of acute tonsillitis. This can be done using the McIsaac screening scale [12], which includes symptoms and their assessment in points (
).
A patient’s symptoms with a score of 3 means the probability of streptococcal etiology is 30%, and a score of 4 means about 70%. If the clinical picture is determined to be 0–1 points, then systemic antibiotic therapy is not indicated. At 2–3 points, antibiotics are necessary only if the infection is bacteriologically confirmed. Antibiotics should be prescribed when symptoms of 4–5 points are detected.
Diphtheria of the pharynx occurs in the form of localized, widespread, toxic I, II, III degrees and hypertoxic forms. With it, gray plaques are detected on the surface of the tonsils, tightly fused with the underlying tissues, they may spread to the arches, the mucous membrane of the posterior pharyngeal wall, the uvula (Fig. 5), and when you try to remove them, the mucous membrane bleeds. Plaques do not rub down and do not dissolve in water. In the toxic form, the neck is noticeably thickened due to swelling of the subcutaneous fat, pressure is painless and does not leave pits.
Infectious mononucleosis is an acute infectious disease caused by the Epstein-Barr virus, characterized by fever, sore throat, enlarged lymph nodes, pharyngeal tonsil, liver, and spleen. Plaques on the tonsils, as in lacunar tonsillitis (Fig. 6), but can spread beyond them. A general blood test (the appearance of atypical mononuclear cells), serological research methods (enzyme-linked immunosorbent assay (ELISA), Paul-Bunnel-Davidson reaction) help in diagnosing the disease.
Fungal infections of the pharynx in the form of curdled films, easily removed when scraped with a spatula, are caused mainly by yeast-like fungi of the genus Candida (about 90% of cases); less commonly, there are mold fungi of the genus Aspergillus, Penicillium [7]. C. albicans permanently or temporarily lives on human mucous membranes, skin and intestines. Factors contributing to the development of mycoses are: treatment with broad-spectrum antibacterial drugs, cytostatics and corticosteroids, diabetes mellitus, blood diseases, tumors, gastrointestinal diseases, vitamin imbalance. Candidiasis of the oral cavity, pharynx and esophagus occurs in more than 90% of AIDS patients (Fig. 7) [3].
Diagnosis of sore throats should include throat and nasal swabs for diphtheria (BL). Express determination of streptococcal antigen using test strips from the surface of the tonsils makes it possible to justify antibacterial therapy. A general blood test facilitates the differential diagnosis of primary and secondary acute tonsillitis. Opinions on the question “Should I do a smear?” controversial. It is needed to confirm the GABHS etiology of the disease in doubtful cases [16].
Therapeutic tactics for pain in the pharynx can be presented in the form of a diagram ().
For the treatment of acute pharyngitis, a gentle diet, hot foot baths, warm compresses on the front surface of the neck, warm alkaline drink (mineral water, milk with honey), steam inhalations, and smoking cessation are recommended. The attitude towards gargling is ambiguous [16]. Fresh infusions of mint, chamomile, calendula, eucalyptus, sage, and caragana are effective for relieving sore throat. Antiseptics of artificial origin (dichlorobenzene, metacresol, hexethidine, benzalkonium, thymol, ambazone, chlorhexidine) are bactericidal in their mechanism of action, which can lead to suppression of the normal microflora of the oral cavity, so they should be used with caution in children under 6 years of age [9]. For the treatment of sore throat, the most important painkillers are those containing menthol, tetracaine, lidocaine or flurbiprofen. Children from 6 months of age can use the herbal preparation Tonsilgon, which has an antiseptic and analgesic effect, but does not contain either menthol or lidocaine.
Menthol preparations and any sprays cannot be used before 3 years of age due to the possible development of laryngospasm.
Local combination drugs (antiseptics and painkillers) in the form of finished dosage forms are the most popular for the treatment of sore throat. One of them is TheraFlu LAR, a universal and highly effective local drug with an antiseptic and analgesic effect. TheraFlu LAR contains benzoxonium chloride and lidocaine. Available in the form of a spray and tablets, the content of lidocaine in which is 0–75 mg and 1 mg, respectively.
Recent in vitro and in vivo studies confirm the broad antiseptic spectrum of benzoxonium chloride and its activity against the main pathogens of the most common diseases of the oral cavity and pharynx. At the same time, the balance of the bacterial flora in the mouth is not disturbed, even with prolonged use of benzoxonium chloride.
Benzoxonium chloride has:
- bactericidal effect against aerobic and anaerobic gram-positive and gram-negative bacteria;
- fungicidal effect against Candida albicans, Aspergillus spp. and yeast fungi;
- antiviral activity against membrane viruses, including herpes virus, influenza virus, parainfluenza viruses, the causative agent of vesicular stomatitis.
Lidocaine is a local anesthetic that reduces pain in the throat when swallowing.
Adults should take the drug 1 lozenge every 2–3 hours (no more than 10 tablets per day) or as a spray, 4 sprays 3–6 times a day. Children aged 4 years and older are prescribed 1 lozenge every 2-3 hours (no more than 6 tablets per day) or as a spray, 2-3 sprays 3-6 times a day. The required duration of treatment, as a rule, does not exceed five days. The drug is well tolerated by patients, side effects are recorded extremely rarely. Possible short-term local irritation of the mucous membrane, allergic reactions.
Indications for its use are: pharyngitis, laryngitis, catarrhal tonsillitis, stomatitis, ulcerative gingivitis. Contraindications to the use of TheraFlu LAR: pregnancy (first trimester), breastfeeding, hypersensitivity to lidocaine, children under 4 years of age. TheraFlu LAR can be used by people with diabetes, as it does not contain sugar. Thanks to the combined effect - antibacterial and analgesic, TeraFlu LAR can relieve all symptoms of viral pharyngitis and be used in the complex therapy of bacterial sore throats.
Systemic antibiotic therapy in the treatment of patients with “sore throat” is indicated mainly for acute tonsillitis (angina) of suspected or established streptococcal etiology (GABHS) and is carried out with penicillins, and if they are intolerant, with macrolides; cefuroxime (Axetin) is effective. Clindamycin and lincomycin are reserve drugs [11]. Epiglottitis caused by Haemophilus influenzae is effectively treated with protected penicillins.
Literature
- Alimetov Kh. A. Secondary neuropathy of the upper laryngeal nerve / M materials of the anniversary All-Russian. scientific-practical conf. with international participation “Modern aspects and prospects for the development of otorhinolaryngology. M., September 29–30, 2005. P. 46.
- Alimetov Kh. A. Spondylogenic pharyngeal dyskinesia / Materials of the anniversary All-Russian. scientific-practical conf. with international participation “Modern aspects and prospects for the development of otorhinolaryngology. M., September 29–30, 2005. P. 22.
- Bessarab T.P., Yushchuk N.D., Anyutin R.G., Potekaev S.N. HIV infection in otorhinolaryngological practice // Attending Doctor, 2000. No. 1. P. 26–30.
- Inflammatory diseases of the mucous membrane of the pharynx, oral cavity and periodontium. Scientific review. Solvay pharma, 2002. P. 2.
- Diseases of the mucous membrane of the oral cavity and lips / Ed. E. V. Borovsky, A. L. Mashkilleyson. 1984. 400 p.
- Karpova O. Yu. Clinic, diagnosis and treatment of laryngoneurosis / Materials of the anniversary All-Russian. scientific-practical conf. with international participation “Modern aspects and prospects for the development of otorhinolaryngology. M., September 29–30, 2005. P. 53.
- Kunelskaya V. Ya., Kasimov K. On the issue of the clinic, diagnosis and treatment of candidal tonsillitis in children // Vestn. otorhinolaryngology. 1980. No. 4. P. 50–52.
- Nisevich N. I., Uchaikin V. F. Infectious diseases in children. M.: Medicine, 1985. 298 p.
- Acute respiratory diseases in children: treatment and prevention. Scientific and practical program of the Union of Pediatricians of Russia / Ed. A. A. Baranova. M., 2008.
- Otorhinolaryngology: national guide / Ed. V. T. Palchuna. M.: GEOTAR-Media, 2008. 960 p.
- Rational antimicrobial pharmacotherapy: Hand. for practicing doctors. Under general ed. V. P. Yakovleva, S. V. Yakovleva. M.: Litterra, 2003. 108 p.
- Sidorenko S.V., Guchev I.A. Tonsillopharyngitis: issues of diagnosis and antibacterial therapy // Consilium medicum. Infections and antimicrobial therapy. 2004. 4: 36–38.
- Folomeeva O. M., Amirdzhanova V. N., Yakusheva E. O. et al. Incidence of rheumatic diseases in the Russian population (analysis over 10 years) // Ter. Archive. 2002. No. 5. P. 5–11.
- Shevrygin B.V., Mchedlidze T.P. Handbook of otorhinolaryngology. M.: Triada-X, 1998. 448 p.
- Shulga I. A., Zaitsev N. V., Zaitseva V. S. Variants of the structure of the stylohyoid complex / Materials of the Anniversary All-Russian. scientific-practical conf. with international participation “Modern aspects and prospects for the development of otorhinolaryngology. M., September 29–30, 2005. P. 75.
- Etiopathogenetic therapy of diseases of the upper respiratory tract and ear: Methodological recommendations. Compiled by S.V. Ryazantsev, Kotserovets V.I. St. Petersburg: National Register, 2008. 100 p.
- Yakovleva V.I. Diagnosis and treatment of neurogenic diseases of the maxillofacial region: Textbook. manual for institutes and faculties. improved doctors. Minsk: Vysh. school, 1989. 102 p.
M. V. Subbotina , Candidate of Medical Sciences Irkutsk State Medical University , Irkutsk
Contact information about the author for correspondence
How is osteochondrosis of the cervical spine diagnosed?
Diagnosis of pathology begins with consultation with a specialist. At the first manifestations of osteochondrosis, consult a rheumatologist, neurologist, surgeon or orthopedic traumatologist. The doctor will ask about the symptoms and the frequency of their occurrence; you need to provide the specialist with a complete medical history and the results of earlier studies (if any). The specialist will conduct a visual examination and palpation, and refer you for tests. During the examination, the doctor pays special attention to neck mobility, muscle tone, skin sensitivity and identifies the most painful areas.
To identify the condition of muscles, ligaments, blood vessels, and to detect inflammatory processes or tumors, an informative and safe diagnostic method is prescribed - MRI of the cervical spine. During an MRI of osteochondrosis, the patient lies on a special sliding table with his back. Rollers are placed on the patient's head to relieve muscle tension, and the limbs are secured with belts. Any slight movement during the procedure can affect the quality of the result. Next, the table moves into the tomograph area. The procedure does not cause pain. The tomograph makes a lot of noise during scanning, so you can use headphones to avoid discomfort.
If MRI is contraindicated, there are other diagnostic methods such as computed tomography and radiography. X-ray is suitable only for primary diagnosis and does not provide a layer-by-layer image of the affected tissue. However, this study is the simplest and most economical, allowing you to examine the patient’s body in several projections. Due to the strong radiation exposure to the body, radiography cannot be performed frequently.
During a computed tomography scan, a scan is performed using one or more beams of ionizing rays. They pass through the human body and are recorded by detectors. The detectors move along the patient's body in opposite directions and record up to 6 million signals. The image displays tissues of different densities with precise definition of the boundaries of organs and the affected areas in the form of a section. The procedure allows you to obtain a layer-by-layer image.