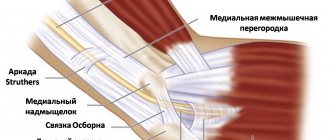
Ulnar nerve compression (UCN) can occur in two places: at the elbow and at the wrist. SLN at the elbow joint occurs in the cubital tunnel (cubital tunnel syndrome). Ulnar nerve neuropathy in the cubital tunnel is the second most common compression neuropathy (the first most common neuropathy is associated with entrapment of the median nerve in the carpal tunnel). Ulnar neuropathy is less commonly seen in Guyon's canal (Guyon's canal syndrome/ulnar carpal syndrome).
Causes
SLN in the cubital and Guyon's canals occurs due to repetitive compression due to support on the elbows or wrists (cyclist's palsy) or prolonged flexion of the elbow. It can also occur due to trauma, swelling, fracture, vascular and bone pathologies/disorders.
Ulnar carpal syndrome occurs when the ulnar nerve becomes compressed between the hook of the hamate bone and the transverse carpal ligament. Guyon's canal syndrome is considered an overuse injury that is typically caused by direct pressure on the handlebars (eg, bicycle handlebars, weight lifting, heavy equipment) and is thus sometimes referred to as "steering wheel palsy." This syndrome may also result from intense gripping, rotation, or repetitive movements of the wrist and hand. Impingement can develop if the hand is flexed and the elbow is abducted for an extended period of time.
The incidence of injuries leading to ulnar nerve compression is unknown; however, ulnar neuropathy has been documented after distal humerus fractures, of which up to 10% are associated with elbow dislocation, and can also develop following any complex trauma to the elbow or wrist.
Treatment of epicondylitis
When making a diagnosis, your doctor will take many factors into account: how your symptoms developed, how active you are, what sports you play, how old you are, and whether you have had any elbow injuries.
To make the diagnosis more accurate, the doctor may order additional tests: ultrasound of the elbow joint, x-rays to clearly image dense structures, magnetic resonance imaging (MRI) to image the soft tissues of the body, including muscles and tendons.
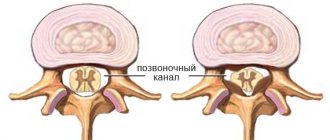
If your doctor thinks your symptoms may be related to a neck problem, an MRI of your neck may be ordered to see if you have a herniated disc or arthritic changes. Both of these conditions can cause arm pain. The most common methods for treating tennis elbow are:
- Limitation of movements, rest and peace
. These are the first steps towards relieving inflammation. You will need to stop/reduce exercise, heavy work, and other activities that cause painful symptoms for several weeks. - Cold compresses
. - Medicines
. You can take an anti-inflammatory drug, acetaminophen or ibuprofen, to reduce pain and swelling. Non-steroidal anti-inflammatory drugs (NSAIDs) containing diclofenac, ketoprofen or others that act symptomatically and do not cause tissue regeneration can also be prescribed. - Physiotherapy
. Special exercises help strengthen the muscles of the forearm. Massage, iontophoresis and laser therapy are effective to improve muscle healing. - Wearing bandages and orthoses
. Using a bandage placed in the center of the back of the forearm promotes rapid recovery. The orthosis massages the tissues during exercise, stimulates metabolism and blood circulation and helps relieve swelling. - Steroid injections
. Steroids (cortisone) are very effective anti-inflammatory drugs. They are injected into the area around the lateral epicondyle to relieve symptoms. - Plasmolifting
. Blood is taken from the patient, then the resulting material is centrifuged to obtain plasma. Platelet-rich plasma (PRP) injections are intended to improve the biological environment of the tissue. Platelets are known for their high concentration of growth factors, which can be injected into the affected area. - ESWT
(Extracorporeal Shock Wave Therapy) - shock wave therapy. Sound waves of different frequencies create “microtraumas” that promote the body’s natural healing processes. Many doctors consider shock wave therapy experimental, but numerous studies confirm the effectiveness of the method.
Approximately 80% to 95% of patients achieve success with conservative treatment. If symptoms do not disappear after 6-12 months of conservative treatment, surgical intervention will be required. Author: Serdyuchenko Sergey Nikolaevich Orthopedic traumatologist of the highest category
Clinical picture
Symptoms of ulnar nerve compression include tingling in the 4th and 5th fingers, weakness when grasping objects with the hand, pain and tenderness in the ulnar aspect of the wrist, forearm and hand, muscle atrophy, and inability to straighten the 4th and 5th fingers (a sign of blessing).
Cubital tunnel syndrome can manifest itself in varying degrees of severity:
Grade I: Mild symptoms such as:
- Periodically occurring paresthesia.
- Some decrease in sensitivity of the dorsal and palmar surfaces of the fifth and medial parts of the fourth fingers.
- No movement disorders.
Grade II: Moderate and persistent symptoms such as:
- Paresthesia.
- Hypesthesia of the dorsal and palmar surfaces of the fifth and medial parts of the fourth fingers.
- Mild weakness in the muscles innervated by the ulnar nerve.
- Early signs of muscle atrophy.
Grade III: Severe symptoms such as:
- Paresthesia.
- There is obvious loss of sensation on the dorsal and palmar surfaces of the fifth and medial aspects of the fourth fingers.
- Significant functional and motor impairments.
- Muscular atrophy of the deep muscles of the hand.
- Inability to straighten the fourth and fifth fingers (a sign of blessing).
Symptoms of Guyon's canal syndrome include:
- Muscle atrophy - mainly in the hypothenar and interosseous muscles, without affecting the palmar muscles:
- weakness when abducting and adducting the fingers (interosseous muscles);
- weakness in adduction of the thumb (abductor pollicis muscle).
- Sensation loss and pain that may involve the palmar aspect of the fifth finger and the medial aspect of the fourth finger, but the dorsal and medial aspect of the fourth finger and the dorsal aspect of the fifth finger do not lose sensation.
- The symptom of a “clawed” hand (a sign of blessing) may be present.
Treatment of cubital tunnel syndrome
The vast majority of such cases of the disease require non-surgical treatment. Non-surgical treatment options for cubital tunnel syndrome include:
- load reduction,
- temporary refusal of intense training,
- taking anti-inflammatory non-hormonal drugs.
Good remedies for treating cubital tunnel syndrome are anti-inflammatory non-steroidal ointments, taking vitamins and the patient undergoing a course of physiotherapy.
Surgical treatment of cubital tunnel syndrome is prescribed if therapeutic methods have not produced results after 12 weeks. During surgery, segments of the canal wall are removed from the patient and the tendon arches are cut. If it is impossible to expand the canal surgically, the nerve is completely removed from it, placing it between muscle tissue and fatty tissue.
Physiotherapeutic examination
Elbow carpal syndrome: It is important to rule out other diagnoses that may be related to the elbow joint. Physical examination includes:
- Assessment of range of motion of the wrist and fingers.
- Manual muscle testing of the ulnar nerve muscles innervated distal to Guyon's canal.
- Sensory examination of the cutaneous branches of the ulnar nerve distal to Guyon's canal
- Assessment of atrophy of the deep muscles of the hand.
Friends, on April 11-12 in Moscow there will be a seminar by Anna Ovsyannikova “Fundamentals of anatomy and biomechanics of the hand. Diseases and injuries of the hand and fingers." Find out more...
Special tests
- "Card" test.
- Froment's sign
- Tinnel's sign in Guyon's canal.
- The Ulnar Nerve Neurodynamic Test (ULTT3) may increase the patient's symptoms.
Diagnostic tests to determine ulnar nerve compression
- Visualization of osteoarthritis, osteophytes or bone cysts.
- Nerve conduction studies (EMG).
- If there is a suspicion of a fracture/dislocation, a plain X-ray.
Diagnostic measures
The diagnosis is made based on the patient’s complaints, external examination, and medical history. Indirect confirmation of a pinched nerve is the presence of previous injuries, endocrine, neurogenic, and articular pathologies. The Froman tests are the most informative in diagnosing compression of nerve fibers. The doctor asks the patient to squeeze the table top so that it is between his thumbs and forefingers. Even with minor pinching, the thumbs will move sideways or bend at the interphalangeal joints.
The next test is to grip a paper sheet with the side surfaces of straightened fingers. A patient with a pinched ulnar nerve will not be able to cope with the task. He will be able to hold a sheet of paper, but at the same time he will bend his fingers (“claw-shaped bird’s hand”).
Froman test.
Then the doctor identifies Tinnel’s symptom and determines the degree of its severity. It presses on the skin located above the cubital canal of the elbow joint. This movement causes a tingling sensation in the thumb, index and middle fingers. The severity of the symptom is detected by changing the intensity of pressure.
| Instrumental and biochemical studies to identify pinched ulnar nerve | The essence of the diagnostic measure |
| Radiography | It is carried out to assess the consequences of injuries and the condition of the elbow joint. The resulting images visualize bone structures and the contours of joint spaces. The study allows you to detect bone growths (osteophytes) that compress nerve fibers |
| MRI or CT | The method is most informative for inflammation of tendons, muscles, ligaments, and soft tissues. Helps to dynamically assess the blood supply to all connective tissue structures of the elbow |
| Electromyography | The study is carried out to identify muscle damage, localization and spread of pathology. Allows you to detect one of the leading signs of pinching - muscle atrophy |
| Electroneurography | This method of studying the speed of electrical impulses along nerves helps to detect innervation disorders. A functional test reveals damage to peripheral nerves, the level and nature of the damage |
| Biopsy | A biochemical study is carried out if there is a suspicion of compression of the nerve by a neoplasm. It helps differentiate malignant and benign tumors |
Criteria for evaluation
- Disabilities of the Arm, Shoulder, and Hand (DASH) is a 30-question questionnaire designed to assess patient function and symptoms.
- The Patient Specific Functional Scale (PSFS) is a questionnaire used to assess a patient's activity limitations and functional outcomes.
- The DASH assessment criteria are a questionnaire that assesses a patient's functional ability and symptom severity.
- The Upper Extremity Functional Inventory (UEFI) is a 20-question questionnaire designed to measure the severity of complex tasks performed throughout the day.
Dragonfly
Lie on your stomach with a small pillow under your chest. Extend your arms out to the sides, elbows straight, and thumbs pointing toward the ceiling. Slowly raise your arms toward the ceiling, tense your shoulders, and lower them smoothly. 2 sets of 15 reps. To increase the effectiveness of the exercise, you can pick up small weights.
Physical therapy
- An impairment assessment approach may be used to identify strength deficits, decreased range of motion, and problems in achieving functional goals.
- The source of pain must be treated in conjunction with the disorder.
- After treatment, re-evaluate the functional tasks that caused pain to determine the effect of treatment.
- Create an exercise program to do at home to treat impairments and perform functional tasks.
A study conducted by Swernlov compared three types of treatment for patients with elbow tunnel syndrome. All three groups showed positive results; the control group showed similar improvement as the intervention groups.
- Splint group protocol —patients wore an elbow splint every night for 3 months to prevent elbow flexion greater than 45 degrees.
- Neural glide protocol – patients did neurodynamic exercises twice a day in six different positions, which were held for 30 seconds (three sets); the break between repetitions was 1 minute. Patients were instructed how to perform these exercises until their next follow-up visit, which was 1–2 weeks later. If no symptoms were found at the next visit to the doctor, the frequency of exercise was increased to three times a day with the position held for 1 minute (every day for 3 months).
- Control Group Protocol – The control group received only educational recommendations.
According to a study report by Coppieters, administration of elbow joint mobilization, thoracic spine and rib thrust manipulation, and ulnar nerve glide/tension techniques for 6 sets was associated with a reduction in elbow pain and a significant improvement in scores on a self-assessment questionnaire. cervical spine for at least ten months of observation. Patients reported a history of symptoms in the two months prior to physical therapy.
Treatment of ulnar nerve neuritis
First of all, it is necessary to eliminate the causes of the disease:
- if neuritis is caused by an infection, then antibiotics or antiviral agents are prescribed - the exact prescription is made by the doctor after a series of studies;
- if neuritis is caused by vascular disorders, then in the absence of contraindications, vasodilators are prescribed;
- To effectively get rid of neuritis of a traumatic nature, it is necessary to ensure complete immobility of the injured limb.
Next, it is necessary to eliminate the inflammatory process. For this purpose, drugs with analgesic, anti-inflammatory and proto-edematous action are prescribed. B vitamins are effective in relieving inflammation. After 2 weeks from the start of taking medications, in some cases anticholinesterase drugs and stimulants of biogenic processes can be prescribed.
Physiotherapeutic procedures, which can be prescribed after 1 week of treatment, can increase the effectiveness of treatment and restore lost functions. The most effective of them, widely used in the treatment of neuritis of various types, include:
- electrophoresis with novocaine and other drugs;
- ultraphonophoresis;
- electrical stimulation;
- impulse currents;
- acupuncture;
- UHF.
Massages, exercise therapy and other procedures may also be prescribed. Doctors from the Health Workshop network of clinics will help determine the most effective treatment methods for each individual case, make a prognosis for recovery and provide comprehensive support to the patient on his path to recovery!
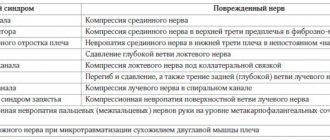
Differential diagnosis
The cervical spine and shoulder girdle should be examined to rule out diagnoses that may relate to the elbow joint. There are many differential diagnoses for ulnar nerve entrapment.
- Elbow fracture/dislocation.
- Cervical radiculopathy.
- Thoracic outlet syndrome.
- Peripheral vascular disease.
- Damage to the collateral ligament of the elbow joint.
- Rheumatoid arthritis.
- Medial epicondylitis.
- Acute polyradiculoneuritis (Guillain-Barré syndrome).
- Neuropathy associated with alcohol (ethanol) consumption.
- Amyotrophic lateral sclerosis.
- Tumor of the apex of the lung.
- Primary bone tumors.
- Peripheral polyneuropathy.
Rehabilitation
Special rehabilitation for quick recovery of the elbow is not always required. For severe bruises, magnetic therapy will help; it is also prescribed for sprains and closed injuries of the elbow joint and forearm bones. If traumatic synovitis is excluded, then from the first days a light massage is given and exercise therapy is carried out, which will prevent the development of deformities and stiffness.
How to develop the elbow joint correctly? Any violence is excluded. If you cannot straighten your arm, you do not need to make additional efforts. It is better to take a repeat (or primary) x-ray and make sure there are no hidden disorders.
Key Points of Physical Therapy
- Special tests used in diagnosing ulnar nerve entrapment have very high sensitivity - 0.98 or higher - and are therefore very useful in making the diagnosis.
- Conservative treatment is effective in approximately 50% of cases, while surgery is effective in 60-95% of cases.
- Conservative treatment has been shown to be effective when introducing the use of orthoses and manual therapy, including neurodynamics and joint mobilization; however, a recent study highlighted that more research is needed to know when conservative versus surgical treatment is needed.
- A patient who begins conservative treatment earlier has a 30% higher chance of avoiding surgery.
Rehabilitation
Rehabilitation is an important point necessary to prevent the formation of adhesions, contractures and a rapid recovery.
Rehabilitation measures should begin as early as possible. After just 2–3 days, it is recommended to begin gradually doing therapeutic exercises, doing gentle exercises, and hand movements.
The earlier start of motor activity in the damaged joint is the most important stage of rehabilitation, since prolonged immobility leads to a decrease in the secretion of synovial fluid and the formation of contractures.
Correct diagnosis, correct treatment with a short period of immobilization, rehabilitation with an early start of physical activity in case of an elbow injury minimize the risks of complications and speed up the recovery period.