Bone cancer is a group of rare tumors. Primary malignant tumors are 50% osteosarcoma. The development of chondrosarcoma is more typical for the pelvic bones. In most cases, diseases of this group are diagnosed in children and young people under 30 years of age. About a tenth of the cases are elderly people, in whom the development of cancer can be triggered by other diseases of the musculoskeletal system.
- Causes and risk factors for developing pelvic bone cancer
- Stages of the disease
- Types of disease
- Clinical picture of osteosarcoma
- How does chondrosarcoma manifest?
- Metastasis of chondrosarcoma
- Diagnosis of the disease
- Therapy methods
- Complications
- Forecast
- Prevention
Causes and risk factors for developing pelvic bone cancer
Factors that predispose to the development of the disease are some disembryonic disorders, as well as radiation and chemical effects on the body. As a result of an experiment on animals, the occurrence of bone cancer was revealed after the effect of radioactive strontium on the body. Precancerous conditions are considered to be osteochondral exostoses and deforming ostosis (Paget's disease).
Osteosarcoma most often develops during periods of increased bone growth. Therefore, adolescents, especially young men, are more at risk of developing this tumor.
Factors contributing to the development of Ewing's sarcoma
There are no reliably confirmed causes and data on the factors influencing the formation of bone tumors. In some cases, a correlation of cancer with traumatic destruction of bone tissue or post-traumatic changes in its structure is revealed.
A number of scientists believe that it is based on a hereditary predisposition caused by various types of gene mutations. In particular, we are talking about the RB1 gene or Paget's disease, as well as some skeletal anomalies (enchondroma, aneurysmal bone cyst). Unfavorable factors include long-term and high-dose exposure to ionizing radiation. However, in the vast majority of patients there is no connection with predisposing factors.
Stages of the disease
The basis for staging bone cancer is the international TNM system. It includes determining the primary tumor site, local spread of the tumor, and the presence of distant metastases.
Thus, there are 4 stages of bone tumors:
- Stage I. The malignant tumor does not extend beyond the bone or involves the cortical layer, and has a high or moderate level of differentiation. There is no damage to lymph nodes or distant metastases.
- Stage II. The tumor does not extend beyond the bone or beyond the cortex, but has a low degree of differentiation or is undifferentiated.
- Stage III. A neoplasm of any degree of differentiation without boundaries in the affected bone.
- Stage IV. Tumor of any size and any differentiation with metastases.
This cancer staging system is the basis for assessing a patient's survival prognosis. It also helps in selecting treatment tactics and the type of surgical intervention.
Bone cancer: how long do they live?
The prognosis for bone neoplasia depends on many factors:
- site of development of the primary tumor;
- type of cancer;
- size of the tumor mass before treatment;
- presence/absence of metastases;
- level of tumor response to therapy;
- general condition of the patient’s body;
- psychological mood.
Unfavorable factors that worsen the patient's survival prognosis include a high tumor volume (100 ml or more), damage to the pelvic bones, metastasis to various lymph nodes and bone marrow.
Types of disease
There are several types of primary cancer that can cause damage to the pelvic bones. These include: osteosarcoma, chondrosarcoma and Ewing's sarcoma.
Osteosarcoma
Osteogenic sarcoma is the most common type of bone cancer. Most often, the disease occurs in children and young people under 20 years of age, but older people aged 60-70 years are also affected. The favorite localization of osteosarcoma is the femur and tibia. This tumor rarely affects the pelvic bones.
Chondrosarcoma
This type of cancer occurs primarily in people over 40 years of age. Chondrosarcoma consists of cartilage tissue cells. It is for this type of cancer that the most common location is the pelvic bones.
Clinical picture of osteosarcoma
The disease manifests itself as a progressive increase in the volume of the affected part of the body. The main symptoms of osteogenic sarcoma of the pelvic bones:
- “Deep” increasing pain over several weeks or months.
- The skin over the tumor may become hyperemic and swollen. A pronounced venous pattern is often identified in this area.
- With a large volume of damage, movements in the hip joint may be limited; in some cases, effusion in the joint cavity is detected.
In the area of tumor growth, a painful, dense formation can be felt, which is fused to the bone. A local increase in skin temperature may also be observed.
How does chondrosarcoma manifest?
The severity of clinical manifestations of chondrosarcoma depends on its morphological structure. Well-differentiated tumors are characterized by long-term slow growth (over 4-5 years) with low severity of symptoms. Such formations can reach significant sizes. With anaplastic chondrosarcomas, which often affect young people, symptoms develop faster, on average within 3 months.
The main symptoms of the disease are pain in the area of tumor growth. The pain is constant, characterized by a progressive increase in intensity. Other local manifestations (increased venous pattern, local increase in temperature, dysfunction of a nearby joint) are less common than with osteosarcoma and are less pronounced.
Book a consultation 24 hours a day
+7+7+78
conclusions
Surgical treatment of neurogenic tumors of the sacrum leads to a decrease in pain intensity, but does not lead to regression of neurological symptoms. The most effective method of controlling symptoms and regressing symptoms of compression of the roots of the sacral plexus is the method of en-bloc tumor resection.
In patients with malignant neurogenic tumors of the sacrum and sacral region, maximum survival and maximum disease-free period are achieved with en-bloc tumor resection. This type of surgical intervention is complex and is often associated with the development of postoperative complications and negative consequences associated with the intersection of nerve formations.
The choice of treatment strategy should be based on the individual characteristics of each case and take into account the functional status of the patient and his ability to tolerate treatment, the correlation between the purpose of treatment and its consequences, as well as the biological properties of a particular tumor.
The authors declare no conflict of interest.
Diagnosis of the disease
Based on complaints and examination of the patient, a specialist may suspect pelvic bone cancer, but an accurate diagnosis can be made using the following instrumental research methods:
- X-ray diagnostics. Taking an image in two projections is mandatory if bone cancer is suspected. The main radiological symptoms of malignant bone tumors are foci of destruction of a plastic, lytic or mixed nature. The lesions do not have clear boundaries. A common symptom is periostitis with a needle or bulbous pattern.
- Osteoscintigraphy. The severity of the malignant process in the bone is characterized by the intensity of accumulation of the radiopharmaceutical. This study is used both to identify hidden lesions inside and outside the bone, and for the purpose of differential diagnosis with bone metastases.
- Computed tomography allows you to clarify the boundaries of tumor formation. Using CT, you can also determine the nature of the location of the primary lesion in relation to the surrounding soft tissues.
- A histological examination is mandatory to establish a diagnosis of bone cancer.
Sometimes it becomes necessary to perform phlebography or angiography. These studies help to clarify the location of the vessels near the tumor before performing surgery.
Diagnostics
To make an accurate diagnosis and identify the level of prevalence of the oncological process, a set of diagnostic procedures is used:
- Physical examination.
- X-ray examination of the lesion site in different projections, angiography.
- Ultrasound examination of various systems and organs.
- CT scan of the primary tumor site. The study allows you to most accurately determine the volume of the tumor mass, the presence or absence of its spread along the bone canal, and connections with the tissues surrounding the neoplasia (vessels and nerve fibers).
- Histological examination of biopsy materials from different places.
- If necessary, consultation with specialists in various fields.
- Blood tests to determine lactate dehydrogenase (LDH) levels. It is an indicator of the level of cell damage, which increases sharply in cancer.
Based on a set of data, an accurate diagnosis is made. Some of these methods, in particular CT and MRI, are also used to evaluate the results of a particular therapy method. The following criteria are used for this:
- The full effect is regression of the tissue component of the tumor, osteolytic foci and metastases.
- The partial effect is stabilization of the oncological process, reduction of the tumor mass by 50 percent or more of the initially determined level.
- Progress of the disease - an increase in the volume of the lesion, the appearance of new lesions, metastases.
Therapy methods
The goal of treatment is to remove the tumor along with part of the healthy bone and surrounding tissue (taking into account zonation), as well as to prevent recurrence and metastasis. Most often, combination cancer treatment is used using chemotherapy and/or radiation methods in combination with surgery.
Surgery
The extent of the operation is determined based on the results of histological examination, tumor size, and general condition of the patient. Often, along with the tumor, it is necessary to remove the muscular-fascial sheath (sheath principle). If the fascial border is technically difficult to access, then the layer of muscles that surrounds it is removed (zonal principle). These features must be taken into account when planning the operation.
The gold standard of surgical treatment is organ-conserving surgery. Such an intervention for cancer of the pelvic bones is interiliac-abdominal resection.
If the tumor affects the hip joint, then endoprosthetics can be performed simultaneously. The use of an endoprosthesis allows one to quickly improve the patient’s quality of life while fully restoring limb function.
Radiation therapy
The method of radiation therapy is selected taking into account the morphological type of cancer and its radiosensitivity. This treatment is used together with chemotherapy, as well as in the process of preoperative preparation.
Chemotherapy
Most often, several drugs are used that mutually potentiate each other's effects. If there is a solitary (single) lesion in the pelvic bones and subsequent surgical intervention, chemotherapy is carried out locally. The antitumor drug is delivered directly to the pathological focus using an arterial catheter. This method is highly effective because it helps to achieve an increased concentration of the drug in the tumor. For a generalized process, systemic chemotherapy is used.
Bone cancer: treatment
After a detailed examination, complex therapy is prescribed. The sequence of traditional treatment methods and their intensity are selected by specialists depending on the stage and characteristics of the oncological process.
Multicomponent polychemotherapy with drugs in different combinations is carried out, taking into account the response of the tumor to the course of treatment. Histologically, a normal tumor response to a chemotherapy session is the presence of a residual amount of living tumor cells in the lesion, in a volume of less than 10%.
Ewing's sarcoma is a radiosensitive tumor, so radiation therapy is prescribed to combat it. However, it is more often performed in those patients in whom induction therapy has been effective. Irradiation of the primary bone tumor is carried out after 3-4 courses of chemotherapy.
If neoplasia is detected in the early stages, the tumor is removed, if possible. The scope of the operation is determined in each specific case. However, it should be understood that radical resection of the lesion cannot always be performed, for example, if the pelvic bones or spine are affected. But with the relative availability of neoplasia located in the ribs, collarbone, fibula, scapula, and upper extremities, this type of treatment has significant advantages. Advanced surgical techniques allow for gentle surgical interventions that preserve the organ as much as possible. This combined approach (situational radical resection of the tumor with intensive methods and dosages of chemoradiotherapy) reduces the likelihood of relapses and spread of the process to distant organs.
In the presence of metastases in the bone marrow, intensive chemotherapy is carried out with combined megadoses of various drugs, with irradiation of a large area of the body and subsequent surgery for a bone marrow transplant from a donor.
Rehabilitation measures (psychological, medical, social) are extremely important for the survival of patients. They should be individually oriented and carried out at various stages of patient management: hospital, dispensary. After performing organ-preserving operations, courses of therapeutic exercises are conducted in order to restore the mobility of the operated limb.
Complications
Malignant bone tumors, especially osteosarcoma, are characterized by hematogenous metastasis. The most common localization of metastases is lung and brain tissue.
It is also common for bone cancer to recur even after complete treatment. 95% of local relapses occur within 2 years after surgery. In this regard, radiography is recommended every 3 months during the first year after tumor removal, once every six months in the second year and subsequently - once a year.
Resection of the pelvic bones with tumor removal and endoprosthetics
Patient O., 25 years old, came to the clinic at her place of residence with complaints of lameness, pain in the groin area on the right, mainly at night, radiating to the right knee joint. During pregnancy, at 6-7 months, the pain spread to the pelvic bones, and a seal appeared in the area of the right half of the pelvis. During childbirth on January 1, 2014, weakness in the right leg and numbness of the limb were noted. A week later, pain appeared in the lower back. She was examined by a gynecologist, a CT scan of the brain and abdominal cavity, and an X-ray of the lungs and pelvis were performed. The examination revealed a mass in the area of the right half of the pelvis. A biopsy was performed: the histological picture may correspond to chondrosarcoma (Grade 1). It is also impossible to exclude the chondroblastic variant of osteosarcoma, but histologically there is more evidence for a cartilaginous tumor.
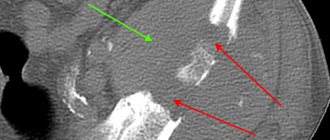
Conclusion on the X-ray examination dated 02/10/2014: the X-ray of the pelvic bones shows predominantly lytic destruction of the body and horizontal branch of the right pubic bone with swelling, spicule-like periostosis and a fairly clearly defined, large extraosseous component with areas of pathological osteogenesis, with a total size of 10*9 cm. Pathological fracture of the horizontal ramus of the right pubic bone. The X-ray picture may be consistent with osteosarcoma of the right pubic bone, complicated by a pathological fracture. The presented photographs of the pelvis and CT scan reveal lytic destruction of the bones of the right half of the pelvis.
In March 2014, the patient underwent surgery in our clinic. She underwent resection of the pelvic bones with tumor removal and endoprosthetics. The morphological diagnosis based on the examination of the surgical material was chondroblastic osteosarcoma of the right pubic bone, Grade 3, with soft tissue invasion. No tumor growth was detected at the resection margins, as was the case in all removed lymph nodes.
The postoperative period proceeded without complications. In October 2014, the patient could already move independently without support. Currently he feels satisfactory.
We observed an even more interesting case 2 years ago. From a surgical point of view, the clinical situation was difficult, but the uniqueness of the observation lies in the fact that after the operation the patient was able to carry and give birth to a healthy child.
Patient B., 40 years old, went to the local clinic in December 2011 with complaints of severe pain in the right hip joint and lameness. 4 blockades were performed, later she was consulted by a neurologist, and the radicular syndrome was treated with conservative drugs without a pronounced effect.
Over time, complaints increased; in June 2012, when examined according to a series of radiographs, no pathology was detected, however, according to MRI and CT in November 2012, a focus of osteolytic destruction without clear contours, measuring up to 4.5x3.2x1, was determined in the body of the right ilium. 7 cm, the structure of the lesion is heterogeneous.
The patient was admitted to our clinic, was examined, and was diagnosed with chondrosarcoma of the ilium with destruction of the cortical layer and growth to adjacent soft tissues, Grade 2. A small area of chondrosarcoma growth (0.6 cm in diameter) was found in the proximal part of the femoral neck.
After the necessary preparation, the patient underwent resection of the pelvic bones with tumor removal and endoprosthetics. There were no complications in the postoperative period; the patient quickly returned to independent motor activity. The rehabilitation after the surgical intervention was so complete that in 2014 the patient was able to carry and give birth to a child.
It should be noted that performing simultaneous oncological endoprosthetics in surgery for tumors of the musculoskeletal system significantly reduces the rehabilitation time of patients and increases their quality of life. Before the use of endoprostheses, such operations were performed without replacing the defect. Patients who underwent surgery walked with or without support, but with a significant limp.